Multiple myloma

Multiple myeloma
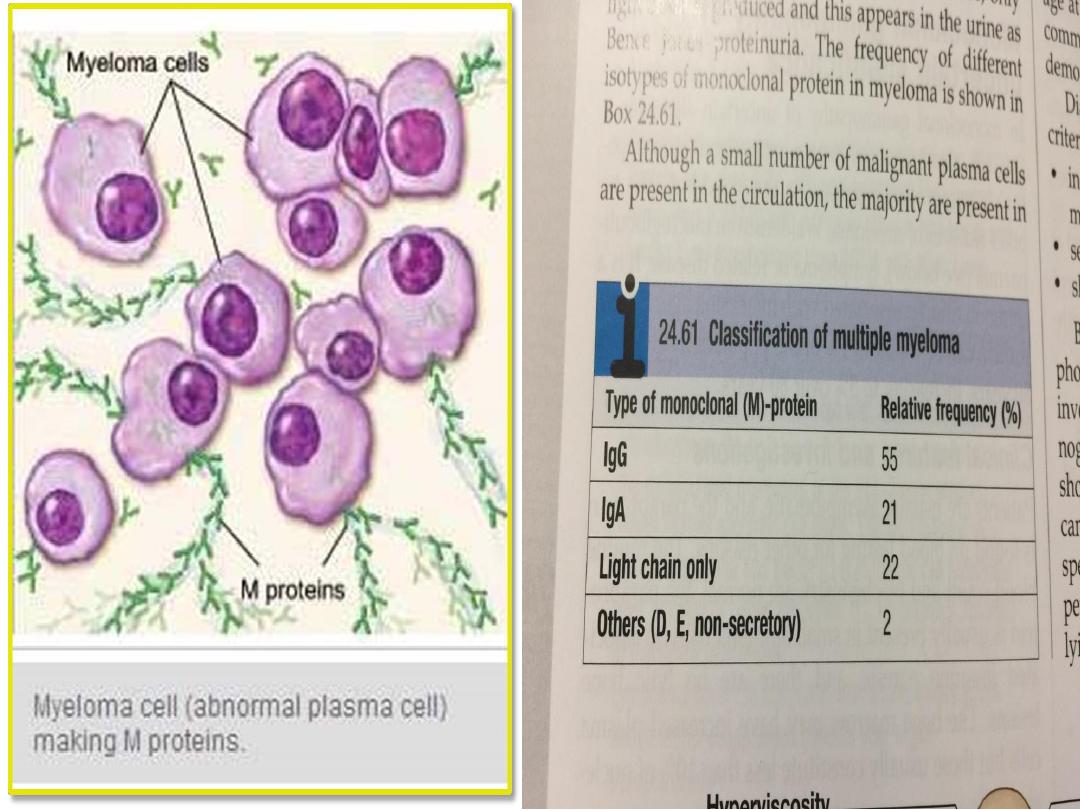
• This is a malignant proliferation of plasma cells.
Normal plasma cells are derived from B cells and
produce immunoglobulins which contain heavy and
light chains.
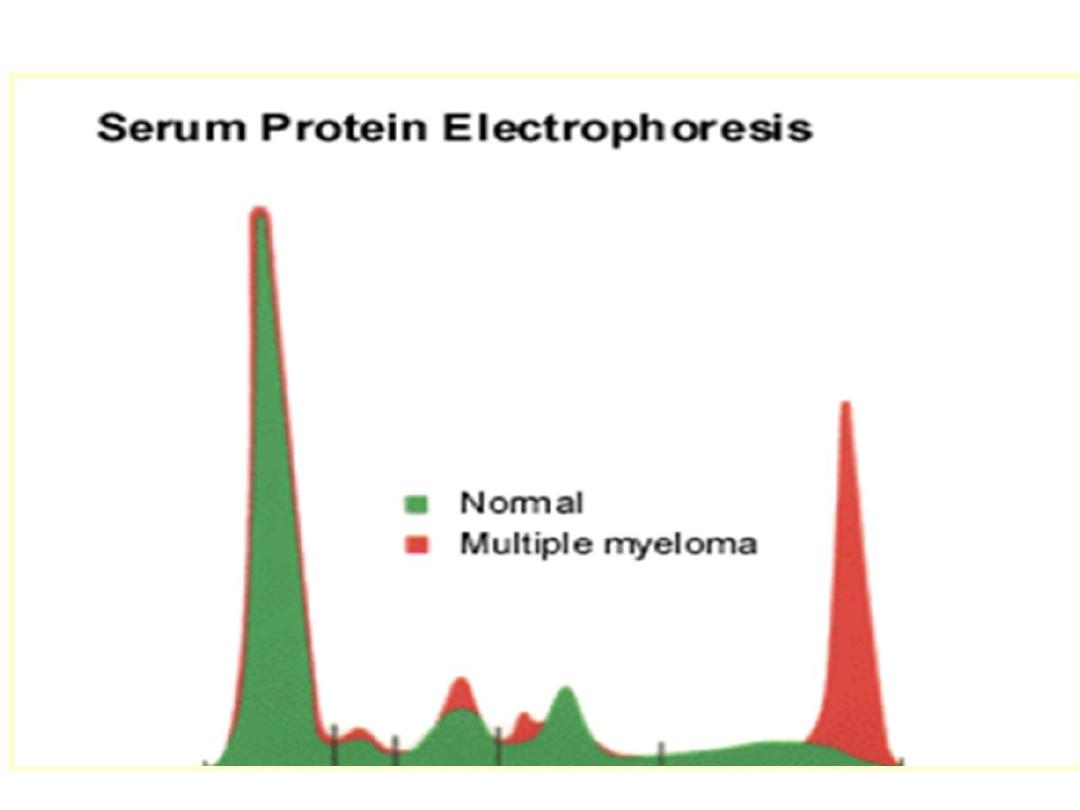
• Normal immunoglobulins are polyclonal, which
means that a variety of heavy chains are produced
and each may be of kappa or lambda light chain
type
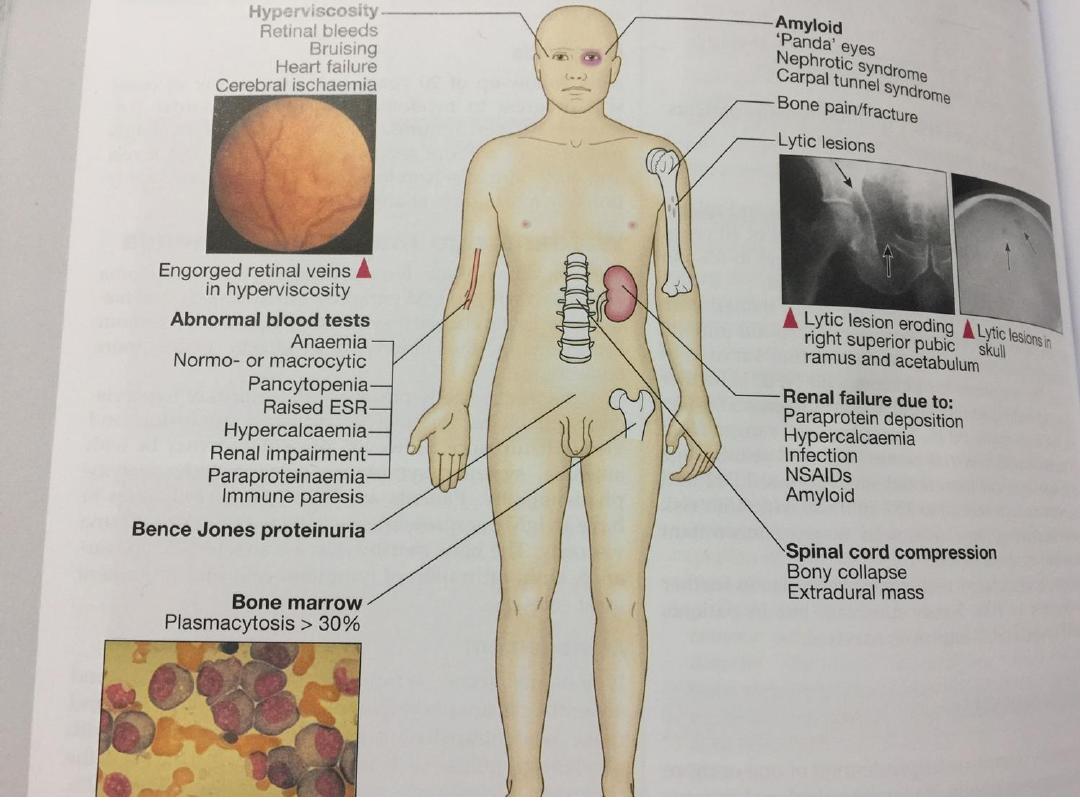
• In some cases, only light chain is produced and this
appears in the urine as Bence Jones proteinuria.
• The malignant plasma cells produce cytokines,
which stimulate osteoclasts and result in net bone
reabsorption.

• The resulting lytic lesions cause bone pain, fractures
and hypercalcaemia.
• Marrow involvement can result in anaemia or
pancytopenia.

Clinical features and investigations
• The incidence of myeloma is 4/100 000 new cases
per annum, with a male to female ratio of 2 : 1
• The median age at diagnosis is 60–70 years and the
disease is more common in Afro-Caribbeans.
Diagnosis of myeloma requires two of the following
criteria:
1. increased malignant plasma cells in the bone
marrow
2. serum and/or urinary M-protein
3. skeletal lytic lesions.
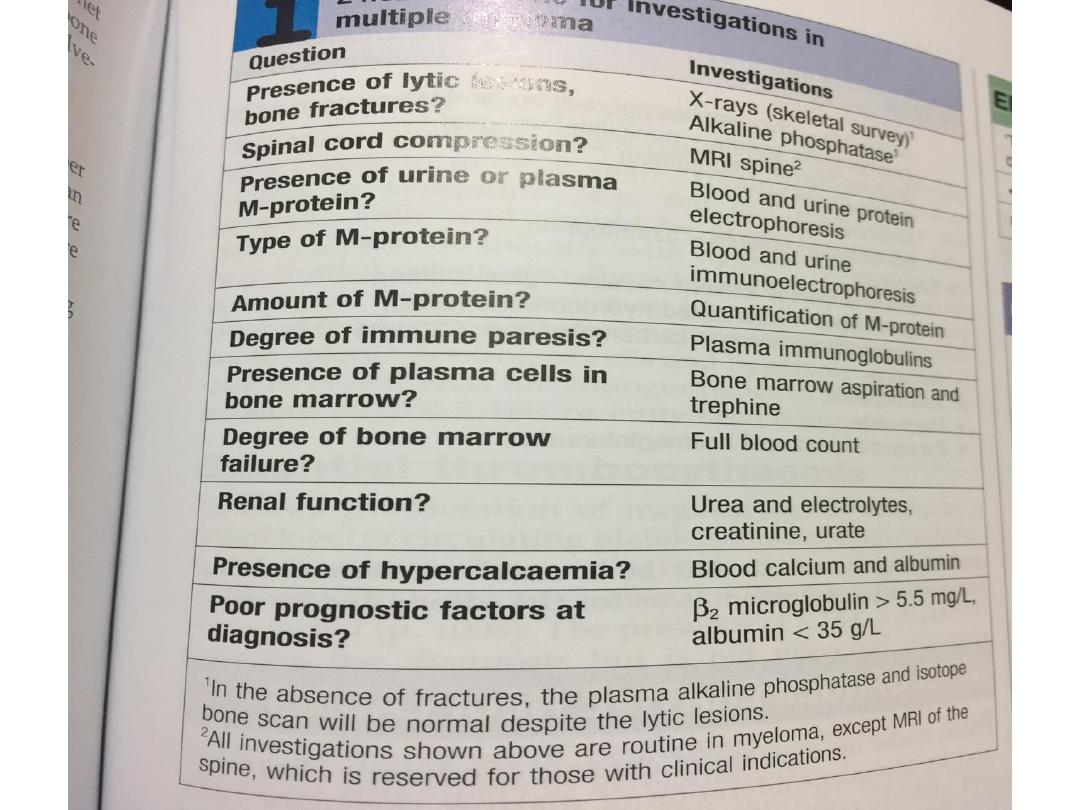
• Bone marrow aspiration, plasma and urinary
electrophoresis, and a skeletal survey are thus
required.

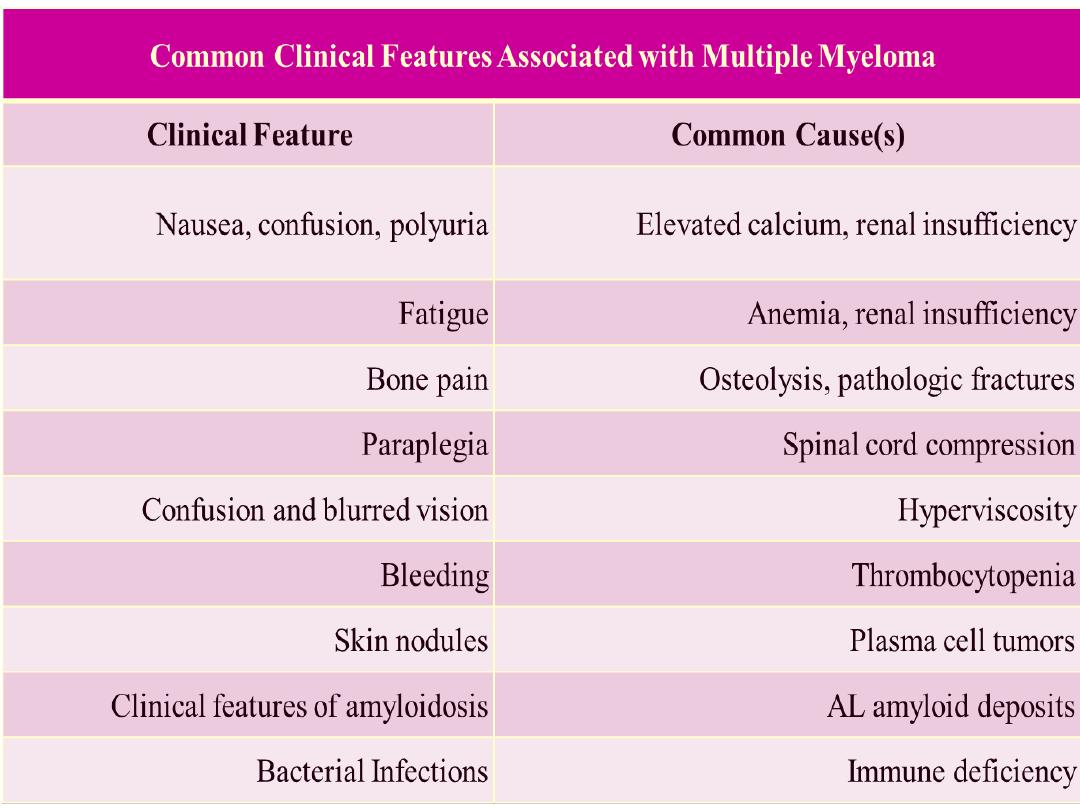
• The presentation of MM can range from asymptomatic
to severely symptomatic, with complications requiring
emergent treatment.
• Systemic elements include bleeding, infection, and
renal failure; pathologic fractures and spinal cord
compression may occur.
• The acronym CRAB emphasizes the most useful clinical
and laboratory features of symptomatic multiple
myeloma: elevated Calcium, Renal insufficiency,
Anemia, and Bone lesions. The clinical features of
multiple myeloma are inconsistent, however, and mild,
early symptoms can mimic many other diseases Bone
pain, which is reported by about 60% of patients at the
time of diagnosis, is the symptom that most
immediately focuses clinicians’ attention on multiple
myeloma. On the other hand, in a population that is
typically in the late 50’s or older at disease onset, bone
pain is also a common and nonspecific finding.

Clinical signs and presenting symptoms
• Musculoskeletal examination:
1. Bony tenderness
2. pain without tenderness
• Neurologic assessment:
1. Sensory level change (ie, loss of sensation below a
dermatome corresponding to a spinal cord
compression)
2. Neuropathy.
3. Myopathy, positive Tinel sign, or positive Phalen
sign .

• Dermatologic evaluation:
1. Pallor from anemia,
2. Ecchymosis,
3. Purpura from thrombocytopenia,
• Extramedullary plasmacytomas (most commonly in
aero digestive tract but also orbital, ear canal,
cutaneous, gastric, rectal, prostatic, retroperitoneal
areas)
Clinical signs and presenting symptoms
• Abdominal examination: Hepatosplenomegaly
• Cardiovascular evaluation: Cardiomegaly
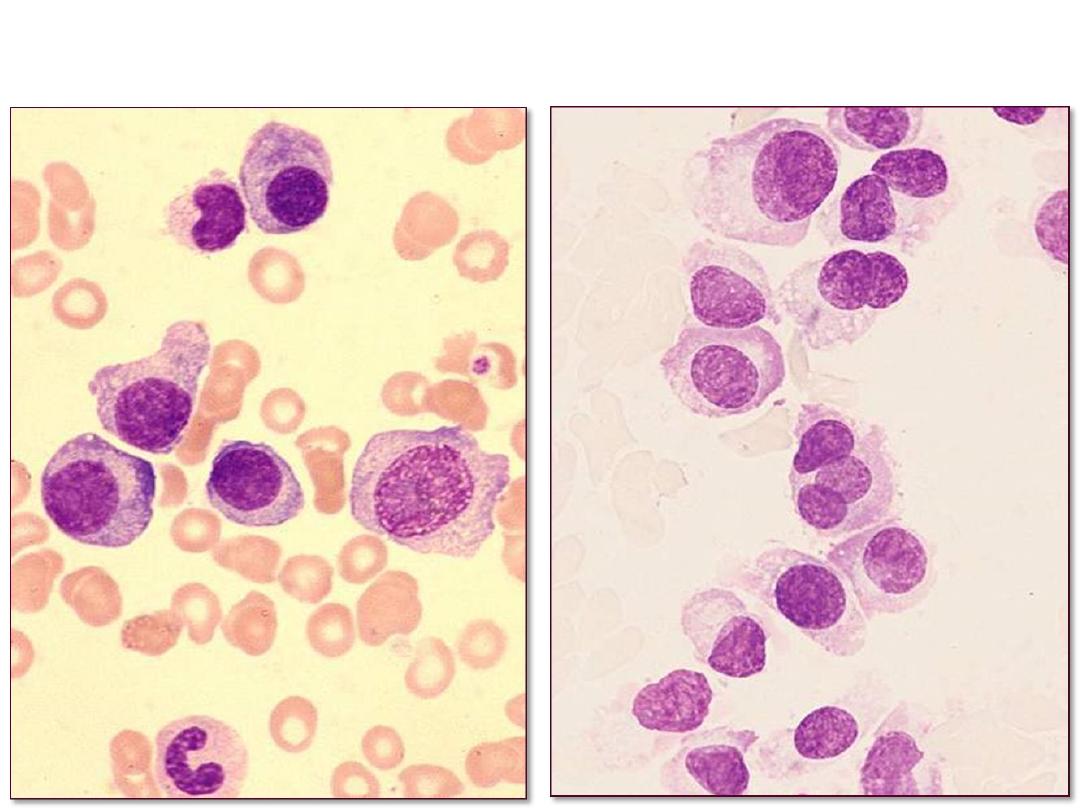
• Bone Marrow Aspiration

Recommended laboratory tests for diagnosis,
prognosis and risk stratification
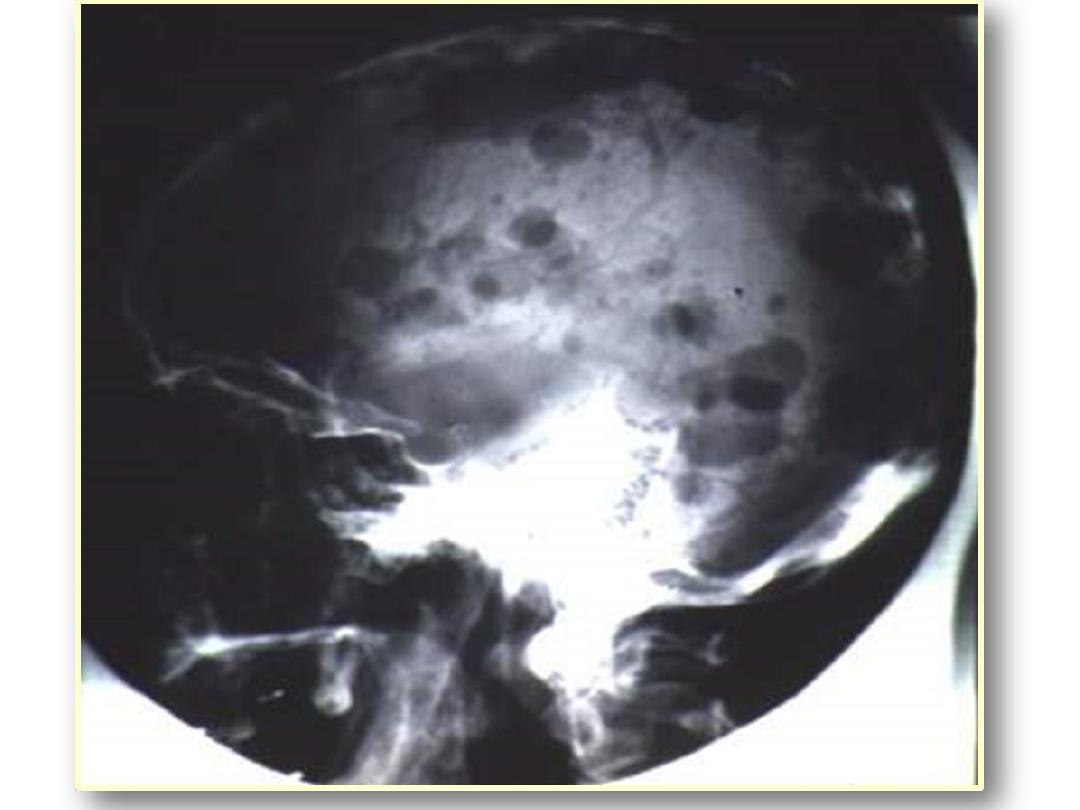
2. Imaging modalities
• Radiological skeletal bone survey, including spine,
pelvis, skull, humeral and femurs is necessary.
• Magnetic resonance imaging (MRI) or computerized
tomography (CT) scan may be needed to evaluate
symptomatic bony sites
• A skull X-ray shows the classic 'punched-out' lytic
bone lesions. Although the skull lesions are
asymptomatic, extensive vertebral involvement
causes compression fractures, resulting in pain and
loss of height (5 cm on average by the time of
diagnosis).

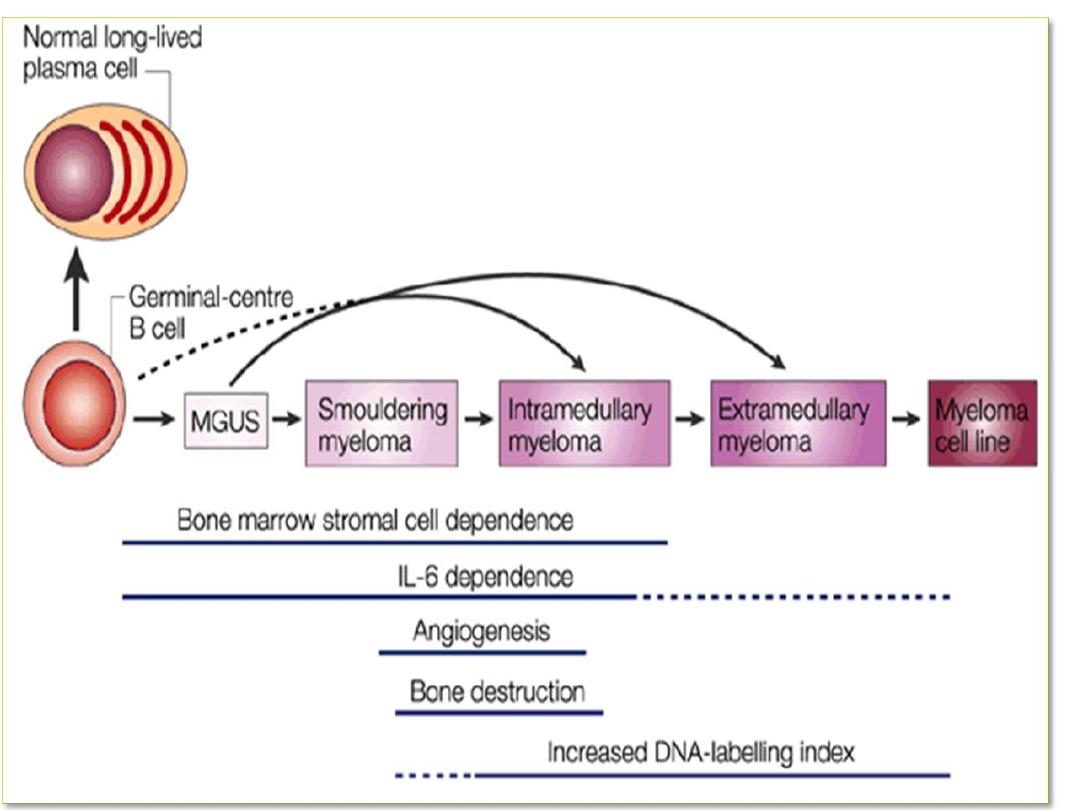
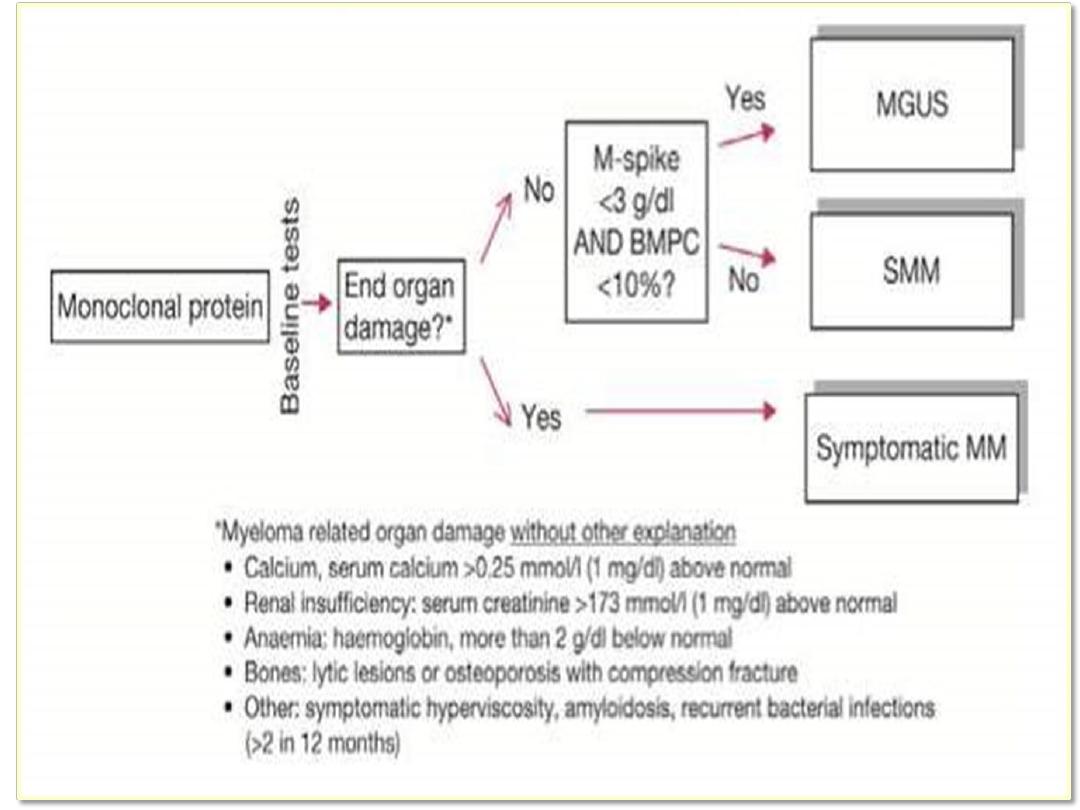
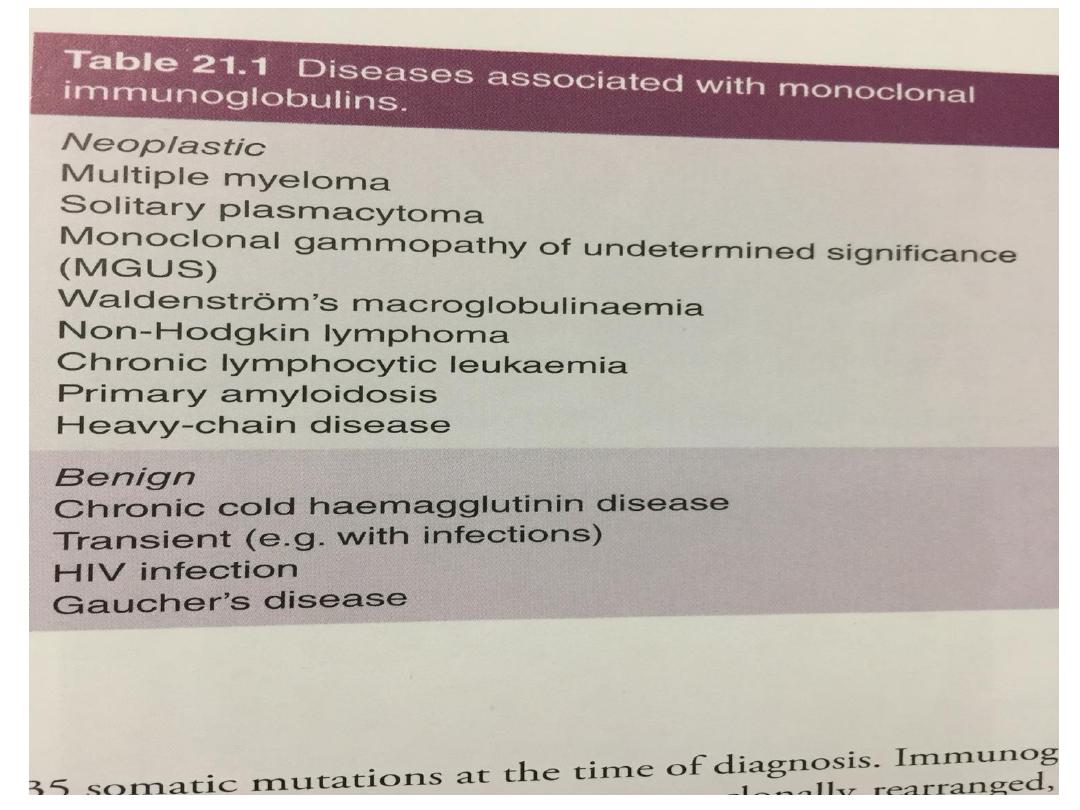
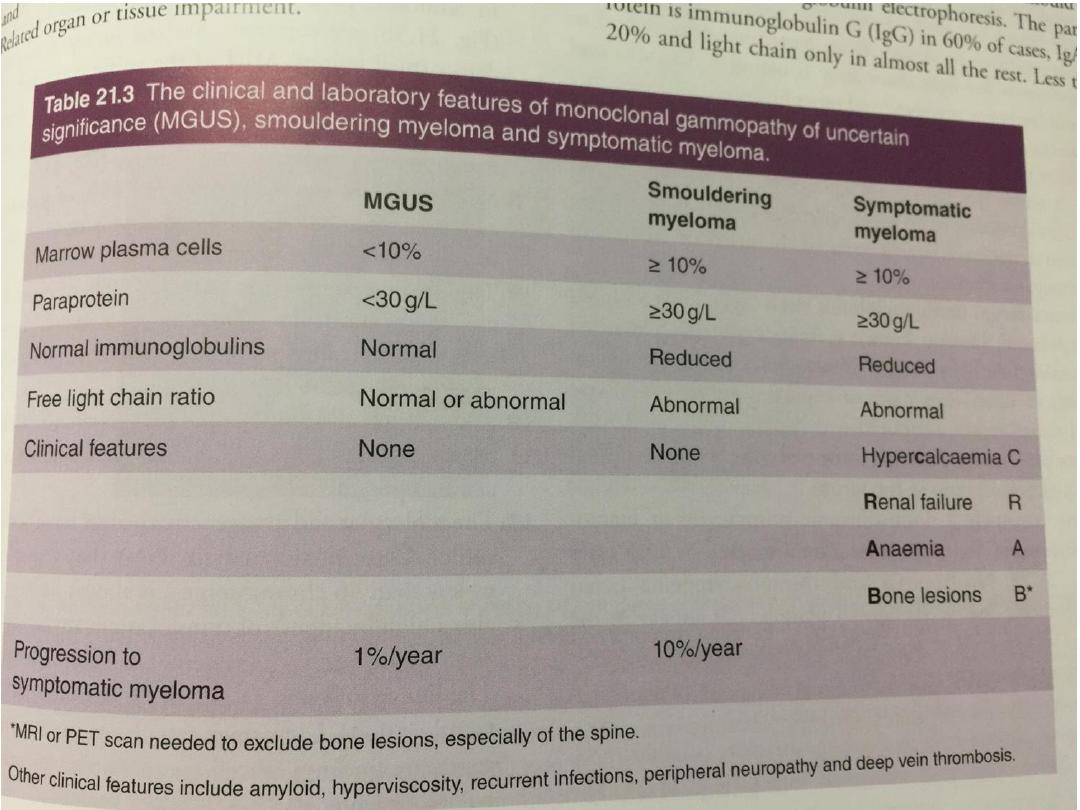
Classification
• It’s important to differentiate between MM and MGUS:
• MGUS:
1. Intact immunoglobulino3 g/100 ml
2. Less than10% bone marrow plasma cells
3. Absence of end organ damage
Classification
• The diagnosis of myeloma requires:
1. 10% or more clonal plasma cells on bone marrow
examination or a biopsy proven plasmacytoma.
2. Evidence of end-organ damage
3. Presence of 60% or more clonal plasma cells in the
marrow should also be considered as myeloma
regardless of the presence or absence of end-organ
damage

• Evidence of end-organ damage
(CRAB):Hypercalcemia ,Renal failure,Anemia,Bone
lesions.
• These lesions are related to a plasma cell
proliferative disorder and not explained by another
unrelated disease or disorder.
• Smoldering multiple myeloma (also referred to
asymptomatic multiple myeloma)
• Both criteria must be met:
1. Serum monoclonal protein (IgG or IgA) 3 g/dl
2. (and/or) Clonal bone marrow plasma cells 10%-
60%.
3. And absence of end-organ damage .

Management
• If patients are asymptomatic with no evidence of
end organ damage (e.g. to kidneys, bone marrow or
bone), treatment may not be required.
• Immediate support
• High fluid intake to treat renal impairment and
hypercalcaemia
• Analgesia for bone pain.
• Bisphosphonates for hypercalcaemia and to delay
other skeletal related events
• Allopurinol to prevent urate nephropathy.
• Plasmapheresis, if necessary, for hyperviscosity.

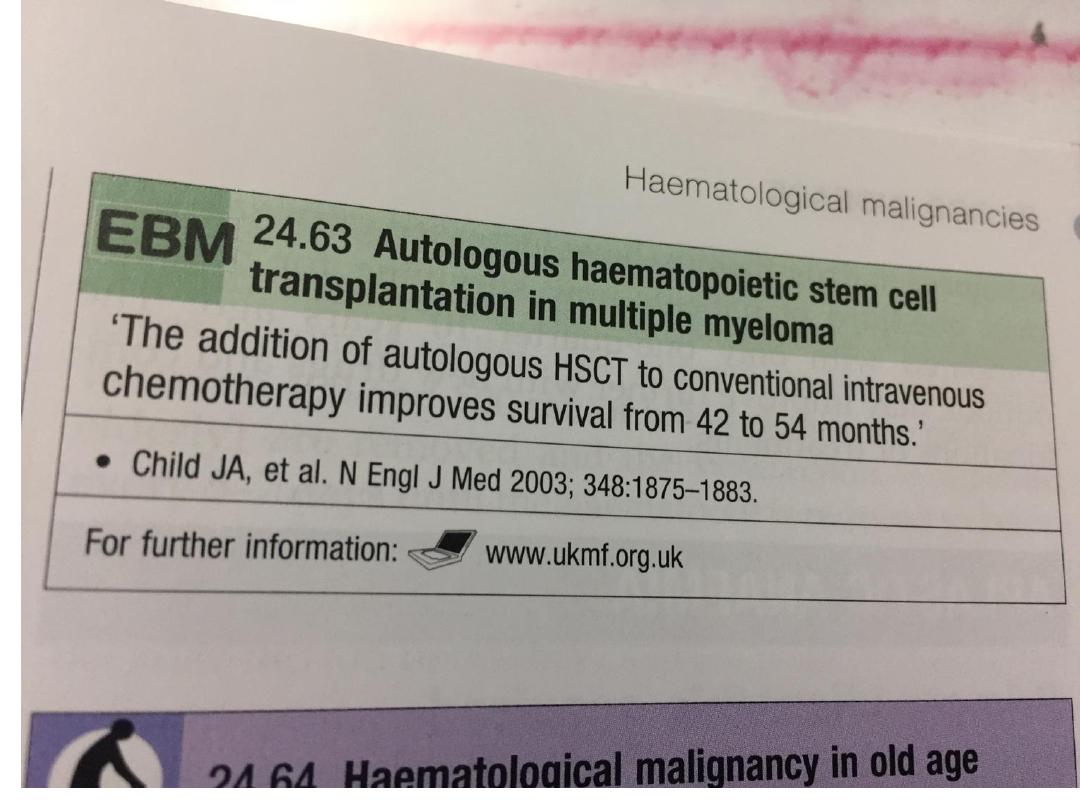
Chemotherapy with or wthout HSCT
• Myeloma therapy has improved with the addition
of novel agents, initially thalidomide and more
recently the proteasome inhibitor bortezomib,
• In younger, fitter patients, standard treatment
includes first-line chemotherapy to maximum
response and then an autologous HSCT,
• Radiotherapy This is effective for localised bone
pain not responding to simple analgesia and for
pathological fractures.
• It is also useful for the emergency treatment of
spinal cord compression complicating extradural
plasmacytomas

• Bisphosphonates Long-term bisphosphonate
therapy reduces bone pain and skeletal events.
These drugs protect bone and may cause apoptosis
of malignant plasma cells.
• There is evidence that intravenous zoledronate in
combination with anti-myeloma therapy confers a
survival advantage over oral bisphosphonates.
• Osteonecrosis of the jaw may be associated with
long-term use; therefore regular dental review is
advisable.

Prognosis
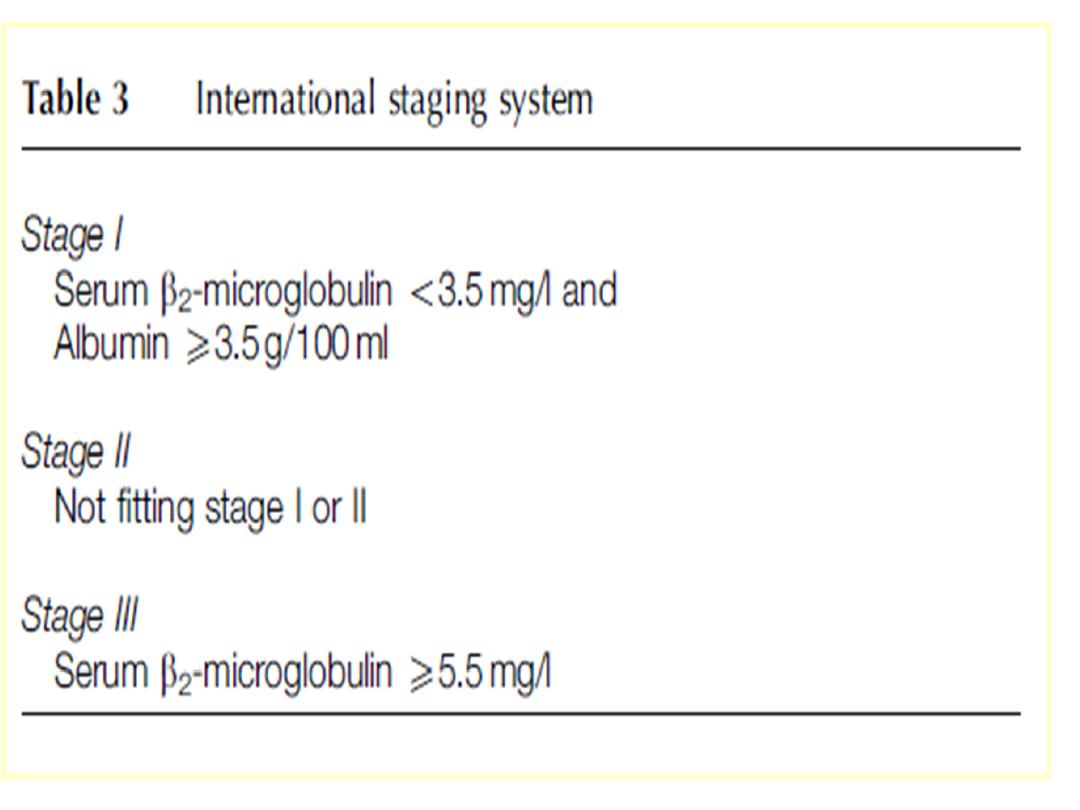
• The international staging system (ISS) identifies
poor prognostic features, including a high β2-
microglobulin and low albumin at diagnosis (ISS
stage 3, median survival 29 months).
• Those with a normal albumin and a low β2-
microglobulin (ISS stage 1) have a median survival
of 62 months.