Hematological emergency
Done by\Haneen Malik NajiSupervised by\ Dr. Amer shareef
Abstract
Hematological emergencies are defined as acute life-threatening conditions in hematological dis-eases due to benign blood disorders or hematological malignancies or as a result of its treatment.
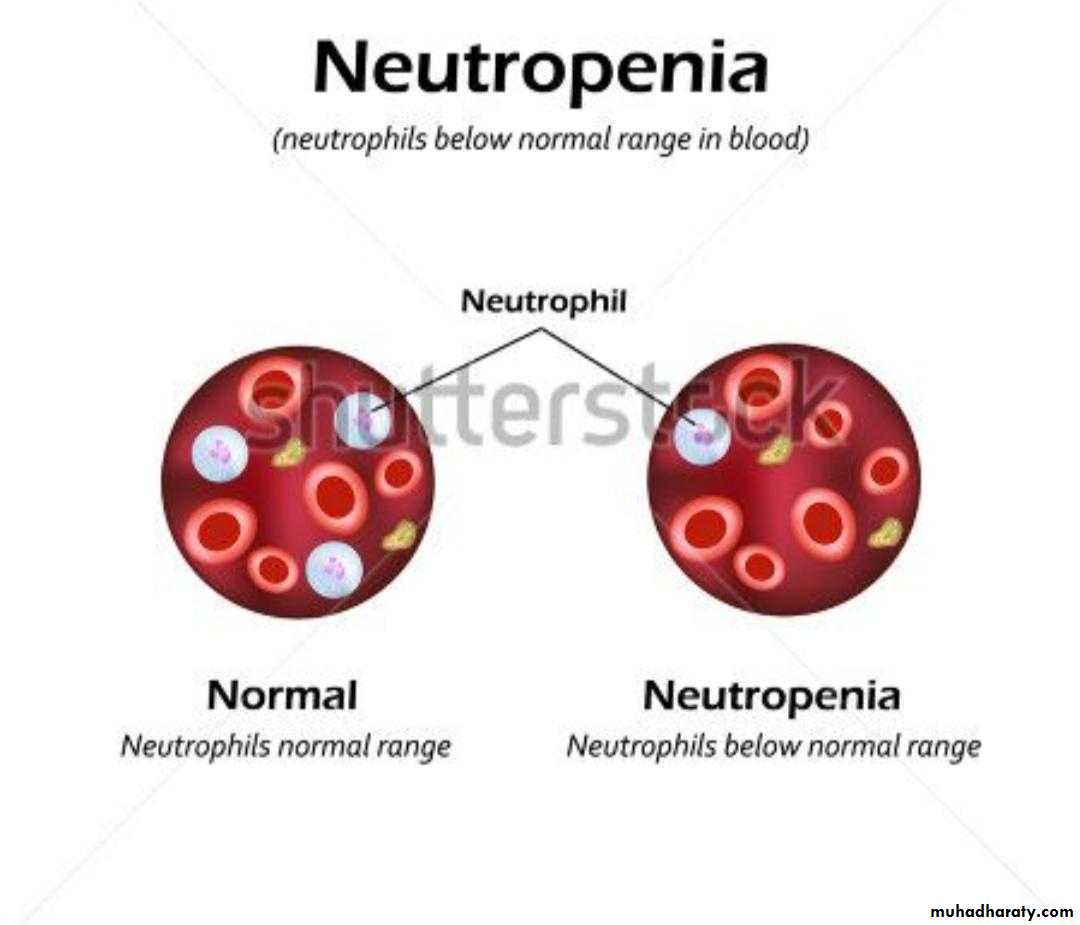
Neutropenic fever:
Febrile neutropenia is the development of fever, often with other signs of infection, in a patient with neutropenia, an abnormally low number of neutrophil granulocytes (a type of white blood cell) in the bloodTreatment
It is superemergency case ,treated by sevepen vial
peprasilen tazopactem
meropenen
sephetazepium
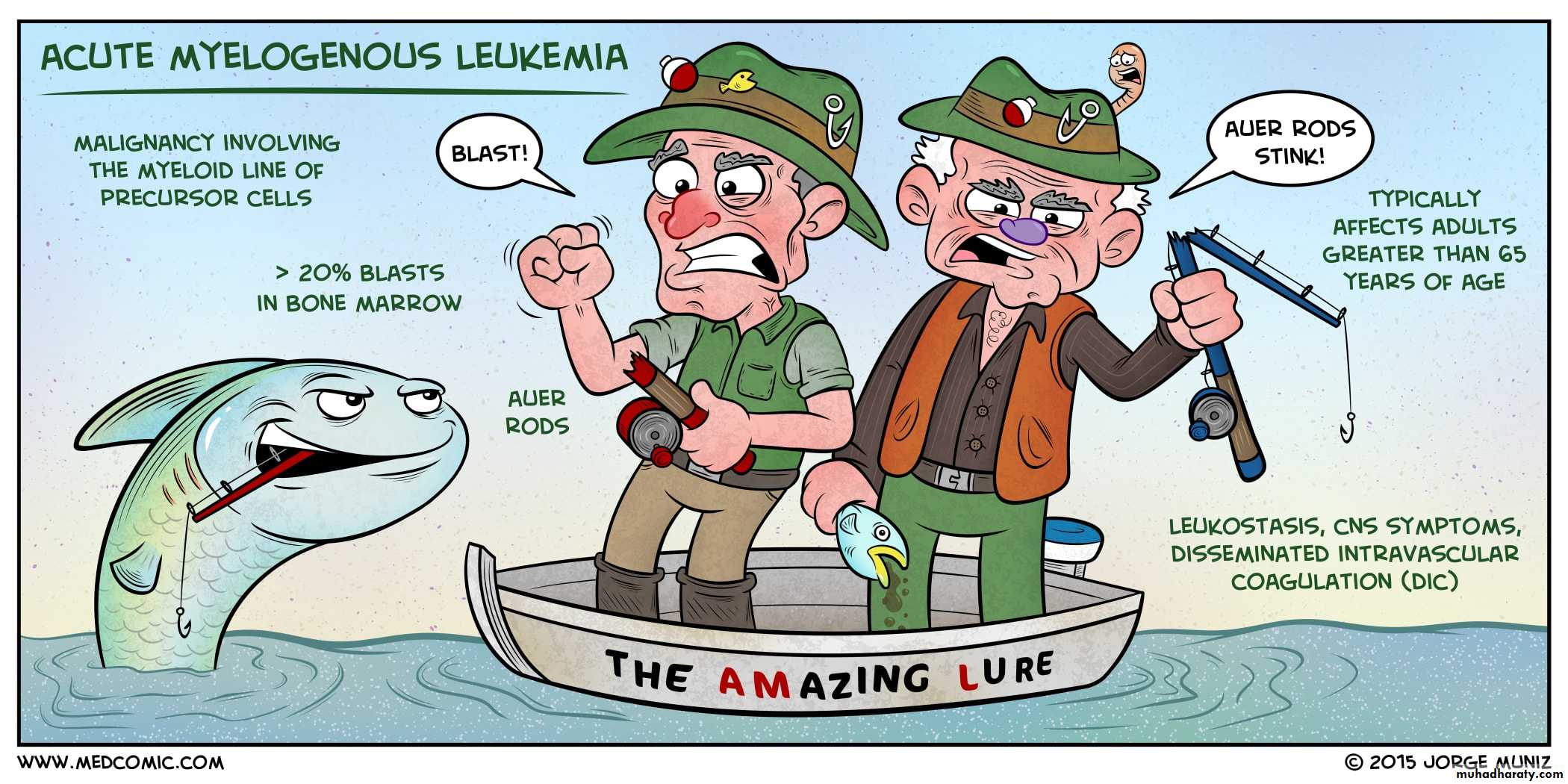
Acute myeloid leukemia
is a cancer of the myeloid line of blood cells, characterized by the rapid growth of abnormal cells that build up in the bone marrow and blood and interfere with normal blood cells. Symptoms may include feeling tired, shortness of breath, easy bruising and bleeding, and increased risk of infection.Occasionally, spread may occur to the brain, skin, or gums. As an acute leukemia, AML progresses rapidly and is typically fatal within weeks or months if left untreated.
Risk factor
include smoking, previous chemotherapy or radiation therapy, myelodysplastic syndrome, and exposure to the chemical benzene. And geneticSign and symtom
drop in red blood cell count (anemia) can cause fatigue, paleness, and shortness of breath. A lack of platelets can lead to easy bruising or bleeding with minor trauma.The early signs of AML are often vague and nonspecific, and may be similar to those of influenza or other common illnesses. Some generalized symptoms include fever, fatigue, weight loss or loss of appetite, shortness of breath, anemia, easy bruising or bleeding, petechiae
Treatment:
First-line treatment of AML consists primarily of chemotherapy, and is divided into two phases: induction and postremission (or consolidation) therapy. The goal of induction therapy is to achieve a complete remission by reducing the number of leukemic cells to an undetectable level;Thrombotic thrombocytopenic purpura
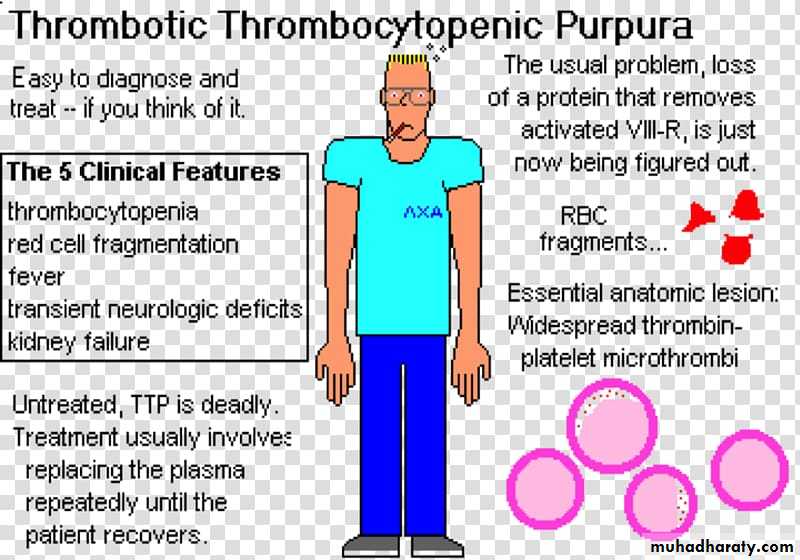
is a blood disorder that results in blood clots forming in small blood vessels throughout the body. This results in a low platelet count, low red blood cells due to their breakdown, and often kidneys, heart, and brain dysfunction Symptoms may include large bruises, fever, weakness, shortness of breath, confusion, and headache ,Repeated episodes may occur.Causes may be autoimmune or genetic
Treatment
Instantons Fresh frozen plasma administrationIf delay .. plasma exchange is
performed (not plasma paresis)
• Glucocorticoid, a mild hope for reducing the auto antibodies against ADAMTS-
Immune thrombocytopenic purpura (ITP)
idiopathic thrombocytopenic purpura, is a type of thrombocytopenic purpura defined as an isolated low platelet count with a normal bone marrow in the absence of other causes of low platelets.] It causes a characteristic red or purple bruise-like rash and an increased tendency to bleed.ITP is diagnosed by identifying a low platelet count on a complete blood count (a common blood test). However, since the diagnosis depends on the exclusion of other causes of a low platelet count, additional investigations (such as a bone marrow biopsy) may be necessary in some cases.
Comolication
The most dangerous complication of ITP is bleeding, especially bleeding into the brain, which can be fatal. However, serious bleeding is rare.The treatments for ITP can have more risks than the disease itself. The long-term use of corticosteroids can cause serious side effects, including:osteoporosis, cataracts, a loss of muscle mass, an increased risk of infection and diabetes
Treatment
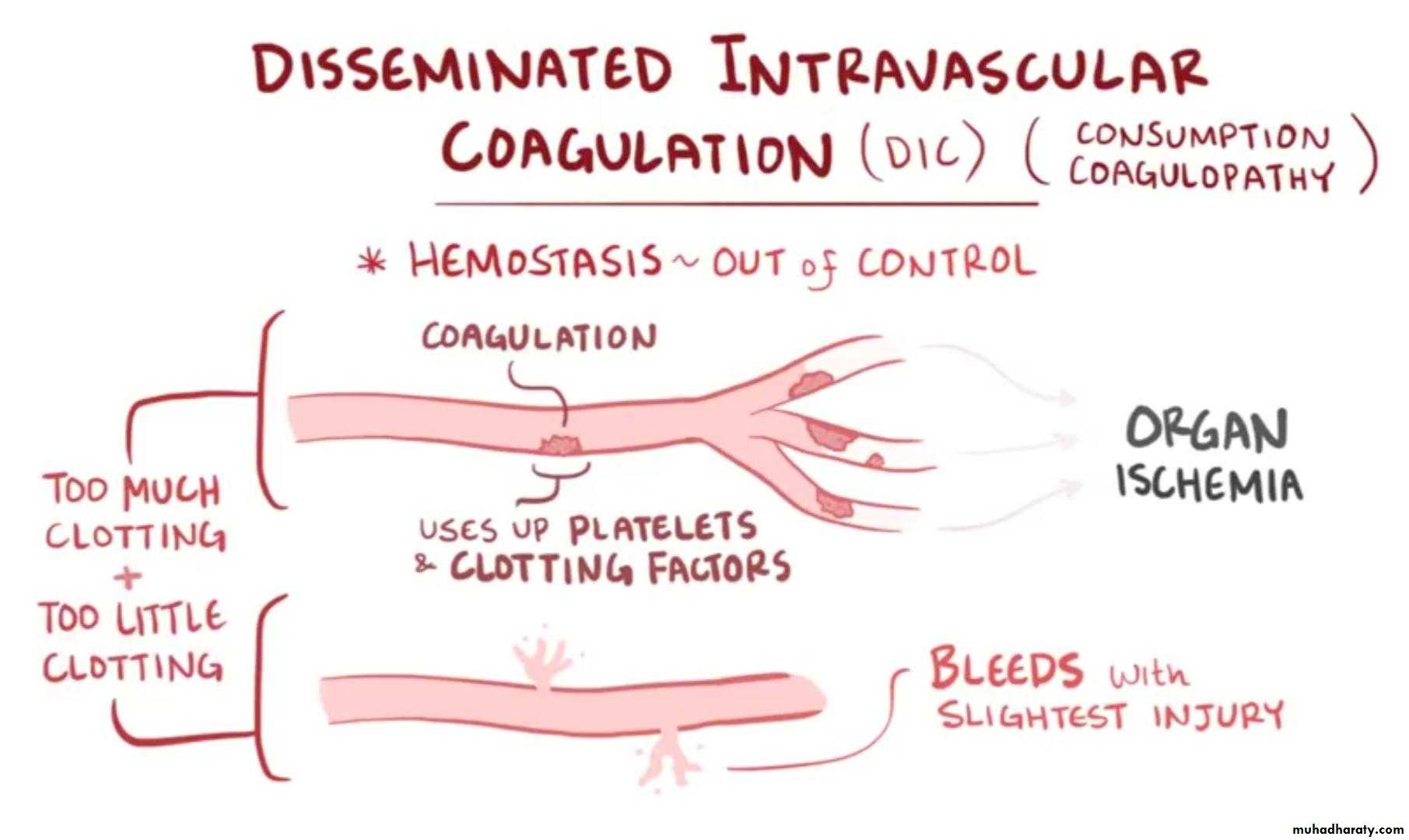
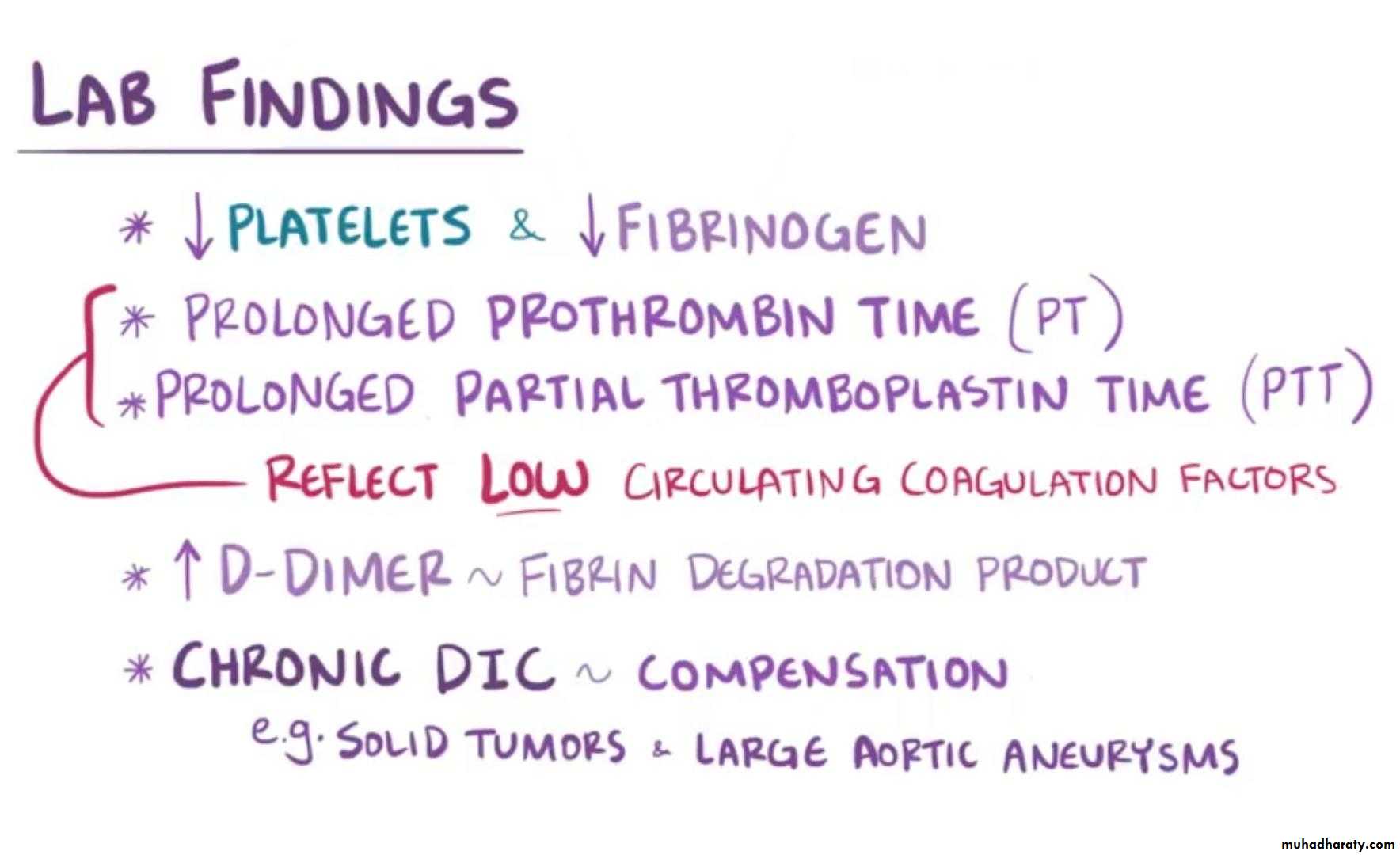
Severe or widespread ITP requires emergency treatment. This usually includes transfusions of concentrated platelets and intravenous administration of a corticosteroid such as methylprednisolone (Medrol), IVIg, or anti-DDisseminated intravascular coagulation (DIC)
is a condition in which blood clots form throughout the body, blocking small blood vessels. Symptoms may include chest pain, shortness of breath, leg pain, problems speaking, or problems moving parts of the body. As clotting factors and platelets are used up, bleeding may occur.This may include blood in the urine, blood in the stool, or bleeding into the skin. Complications may include organ failureTreatment
Treatment of DIC is centered around treating the underlying condition. Transfusions of platelets or fresh frozen plasma can be considered in cases of significant bleeding, or those with a planned invasive procedure. Cryoprecipitate can be considered in those with a low fibrinogen level.Treatment of thrombosis with anticoagulants such as heparin is rarely used due to the risk of bleedingRecombinant human activated protein C was previously recommended in those with severe sepsis and DIC
Sickle cell crisis
pain that can begin suddenly and last several hours to several days. It happens when sickled red blood cells block small blood vessels that carry blood to your bones. You might have pain in your back, knees, legs, arms, chest or stomach. The pain can be throbbing, sharp, dull or stabbingTreatment
use supplemental oxygen for patients who are hypoxic , and Packed red blood cells (transfuse 10 mL/kg over 2hr period) for pt with anemia
Analgesia ,IV opioids (morphine or hydromorphone) .. Non-opioid analgesia
NSAIDs
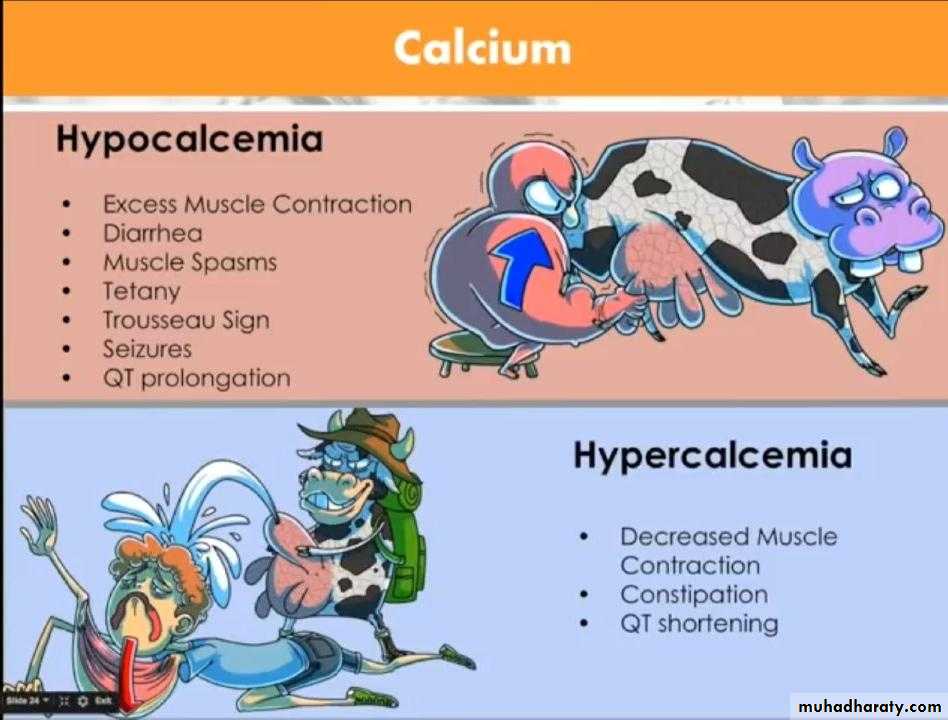
Hypercalcemia
Present in 44% of with canser pt which refer to hematology malignancy , multiple myeloma is most frequensy resposible, follow by aggressive lymphoma and acute leukemia ,Sign and symptom:
Neurologic Fatigue, altered mental status including coma, posterior reversible leukoencephalopathyGastrointestinal Nausea, vomiting, constipation, peptic ulcer disease, and pancreatitis
Cardiovascular Short QT interval on ECG˚, ST segment abnormalities including ST segment myocardial infarction mimic,
malignant ventricular arrhythmias, and hypertension
Renal Nephrogenic diabetes insipidus, acute kidney injury
Treatment
Hypercalcemia’s treatment can be obtained by arresting the pathological bone reabsorption, increasing thecalcium renal excretion or reducing the calcium intestinal absorption.
In the case of asymtomatic or mild hypercalcemia (serum calcium < 12 mg/dL or 3 mmol/L) a supportive
treatment including proper hydration with saline, furosemide, and diet low in calcium may be enough waiting to
treat the underlyng disease..
Treatment
The treatment of moderate hypercalcemia (serum calcium 12 - 14 mg/dL or 3 - 3.5 mmol/L) to severe (serum
calcium > 14 mg/dL or > 3.5 mmol/L) must be more quick and aggressive.
Acute Tumor Lysis Syndrome
The acute tumor lysis syndrome (ATLS) is an oncologic emergency that may arise at the beginning of cytotoxicchemotherapy, especially in the case of tumors by high kinetic, high dimension or with high metastatic load. It is
supported by the massive release of large quantities of nucleic acids, phosphate and potassium by the tumor cells
destroyed.
Treatment
Treatment is first targeted at the specific metabolic disorder.Acute kidney failure prior to chemotherapy. Since the major cause of acute kidney failure in this setting is uric acid build-up, therapy consists of rasburicase to wash out excessive uric acid crystals as well as a loop diuretic and fluids. Sodium bicarbonate should not be given at this time. If the patient does not respond, hemodialysis may be instituted,
Treatment
Acute kidney failure after chemotherapy. The major cause of acute kidney failure in this setting is hyperphosphatemia, and the main therapeutic means is hemodialysis. Forms of hemodialysis used include continuous arteriovenous hemodialysisHemophilia
mostly inherited genetic disorder that impairs the body's ability to make blood clots, a process needed to stop bleeding.] This results in people bleeding longer after an injury, easy bruising, and an increased risk of bleeding inside joints or the brain.Those with a mild case of the disease may have symptoms only after an accident or during surgery. Bleeding into a joint can result in permanent damage while bleeding in the brain can result in long term headaches, seizures, or a decreased level of consciousnessClinical feature
Type A and B carry same symptoms:• Intracranial hemorrhage
• Bruises and hemarthrosis (commonest presenting symptom).
• Malena
• GI bleeding
Hemophilia C: Asymptomatic (only incidental laboratory findings)
Life-threatening complications
• Intracranial bleeding (Most one).• Nasopharyngeal bleeding close throat and airways.
• GI bleeding (obscure, hidden enemy).
• Iliopsoas bleeding (features of appendicitis-pain & tenderness … etc.).
Treatment
• In emergency situations, give cryoprecipitate (contains factor VIII & vWP).
o Not whole blood.
o Not platelets.
• Desmopressin (increase vWF, the chaperon of factor VIII).
• No treatment for hemophilia C.
• Fresh frozen plasma for parahemophilia (It contains all factors except VIII).
• Definitive treatment is by recombinant factor VIII or IX.