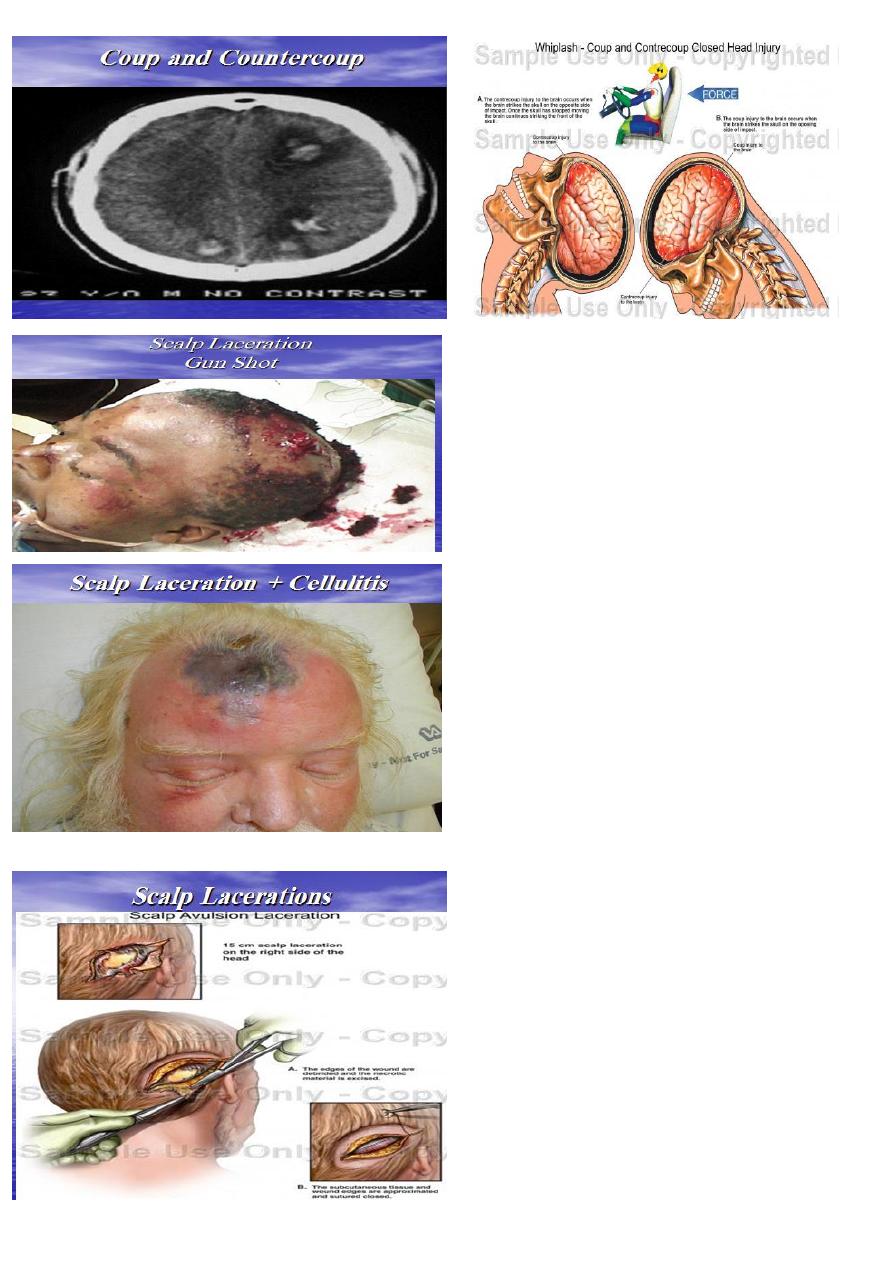
Dx : Scalp wound (laceration)
Complication : 1) sever hemorrhage if not controlled.
2) infection : cellulitis.
Management of Scalp laceration
• Plain X-ray is performed.
• Shaving widely around the wound.
• Closure in 2 layers
• Antibiotic if there is infection
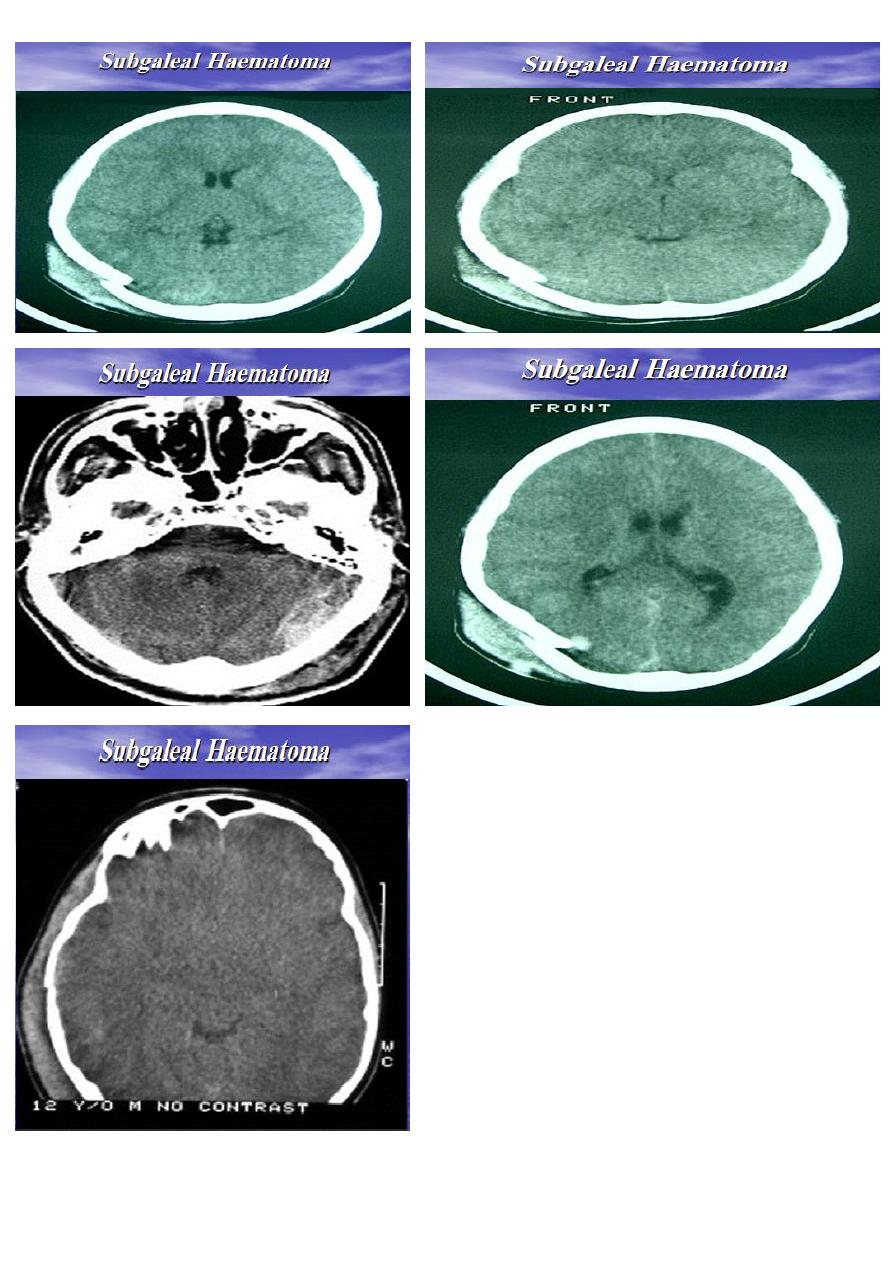
May be subgaleal or subpericranial.
Investigation : CT.
Management of Scalp Haematoma (Subgaleal
Haematoma) :
Leave the lesion alone.
It should not be tapped.
Correction of anaemia in children
less than 1 year of age.
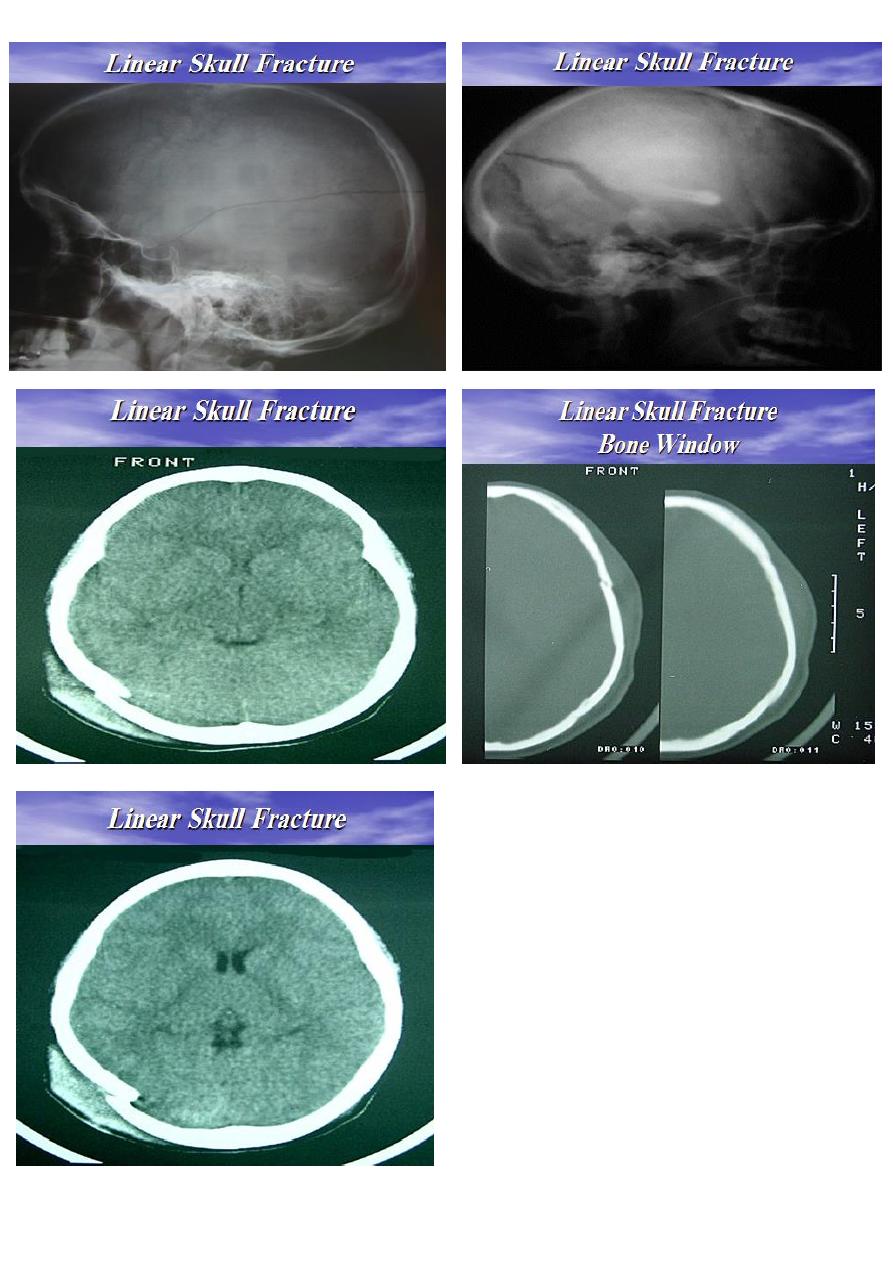
Type : May be closed or opened.
Cause : Result of blunt trauma.
Investigation : Usually require computed tomography .
Treatment : no specific neurosurgical management.
Patient should be admitted for 48 hours of observation
Complication :Fractures crossing the squamous
temporal bone may lacerate middle meningeal vessels
and cause extradural haematoma.
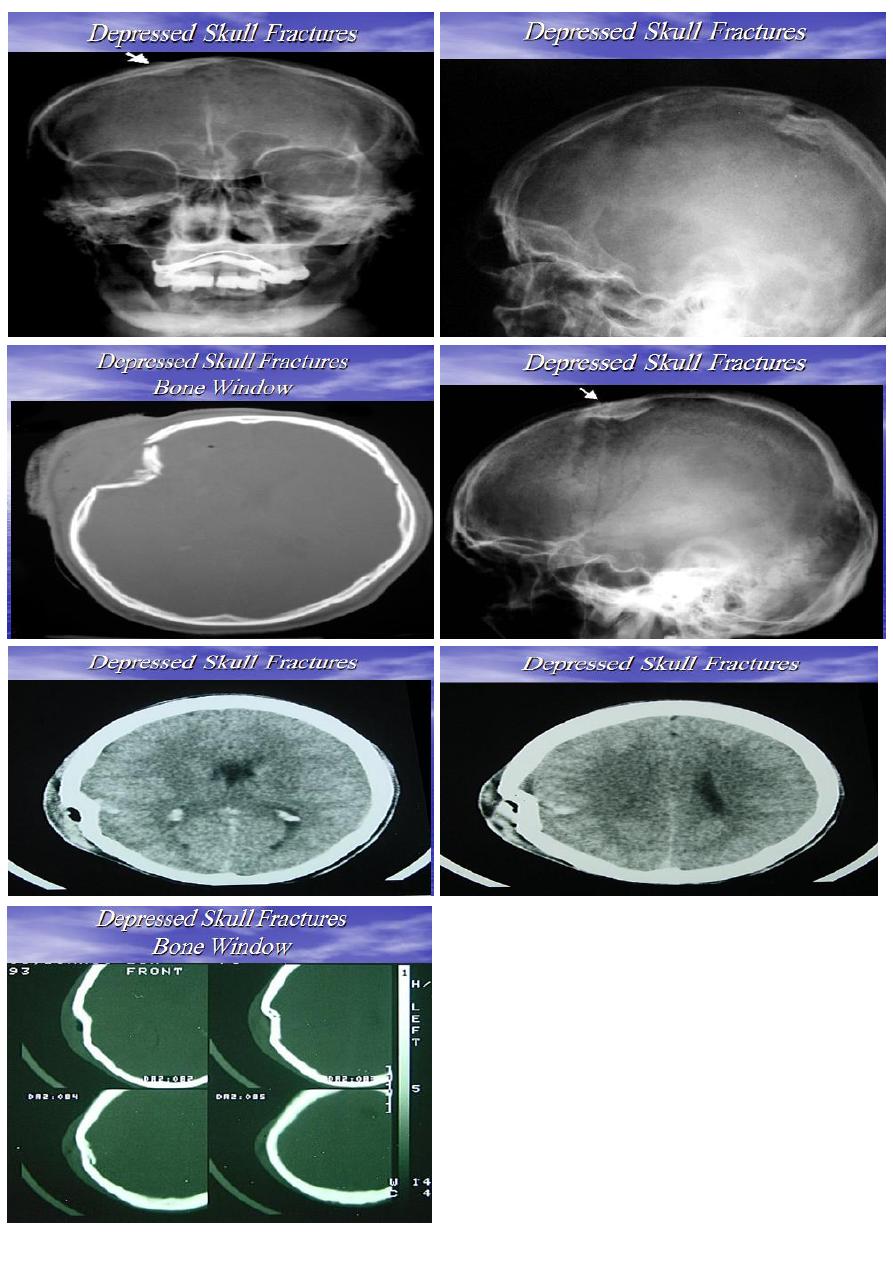
Cause : Usually result from sharper trauma.
TYPE : Depressed skull fractures may be:
Closed depressed fractures
Compound depressed fracture (opened)
Investigation: Plain X-ray visualize the depressed Seg.
Treatment : usually conservative measures
Indications for surgery to raise closed depressed F.
1. Large depressed segment with
possibility of dural tear.
2. Alleviate mass effect.
3. Cosmetic purposes.
4.
To prevent secondary infection
.
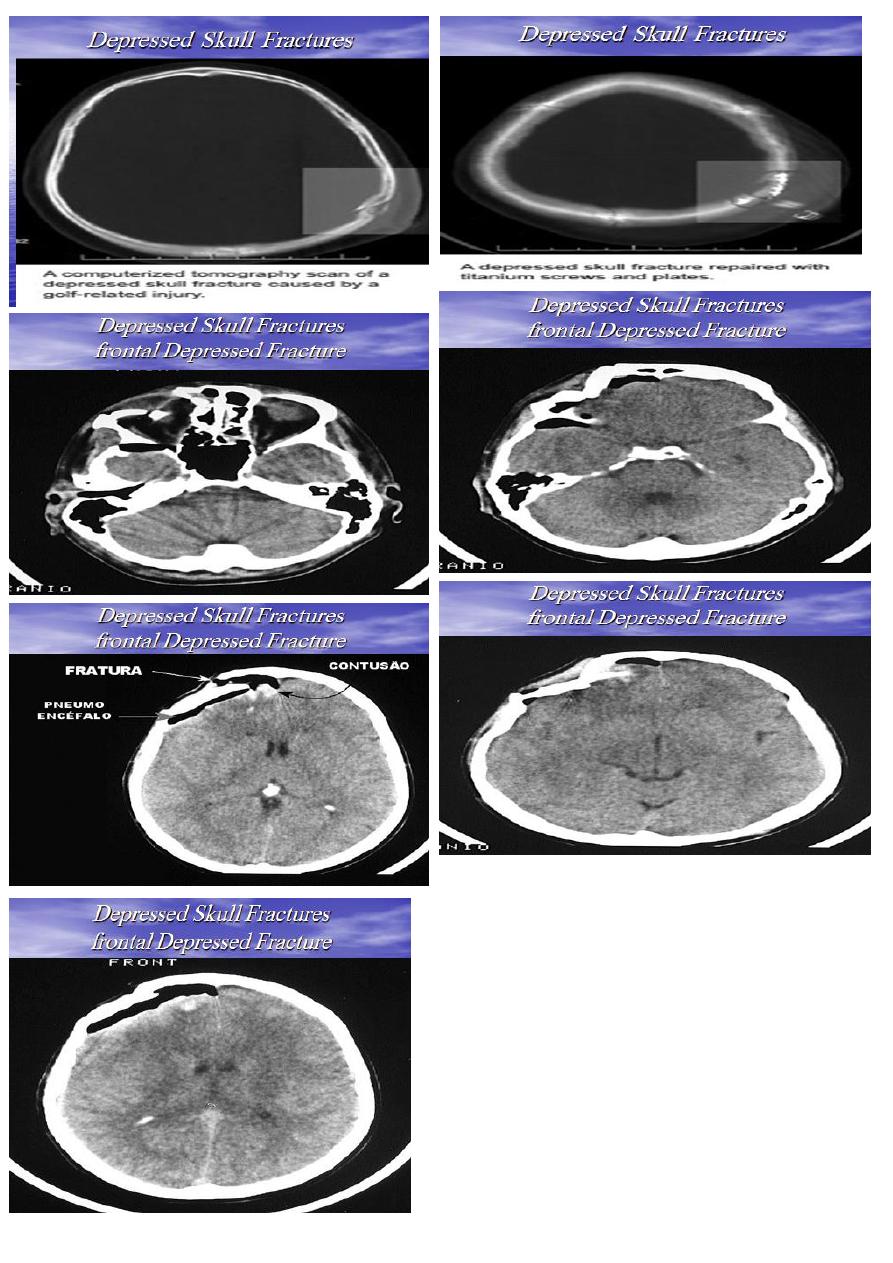
Complications of depressed fractures
1. Dural tear leading to prolapse of the brain.
2. Infection; may lead to osteomyelitis or meningitis.
3. Epilepsy: either early or late.
4. Cosmetic deformity.
5. Sever bleeding from one of the venous sinuses.\
Treatment of compound depressed fracture
1. Foreign bodies are meticulously removed.
2. The depressed segment is gently elevated to avoid
tearing of the dura.
3. Any prolapsed or necrotic tissue is sucked and
haemostasis is performed.
4. Any dural tear is repaired.
5. Removed bone segments are cleaned and replaced.
6. The pericranium and the scalp are sutured.
7. Prophylactic antibiotics are administered..
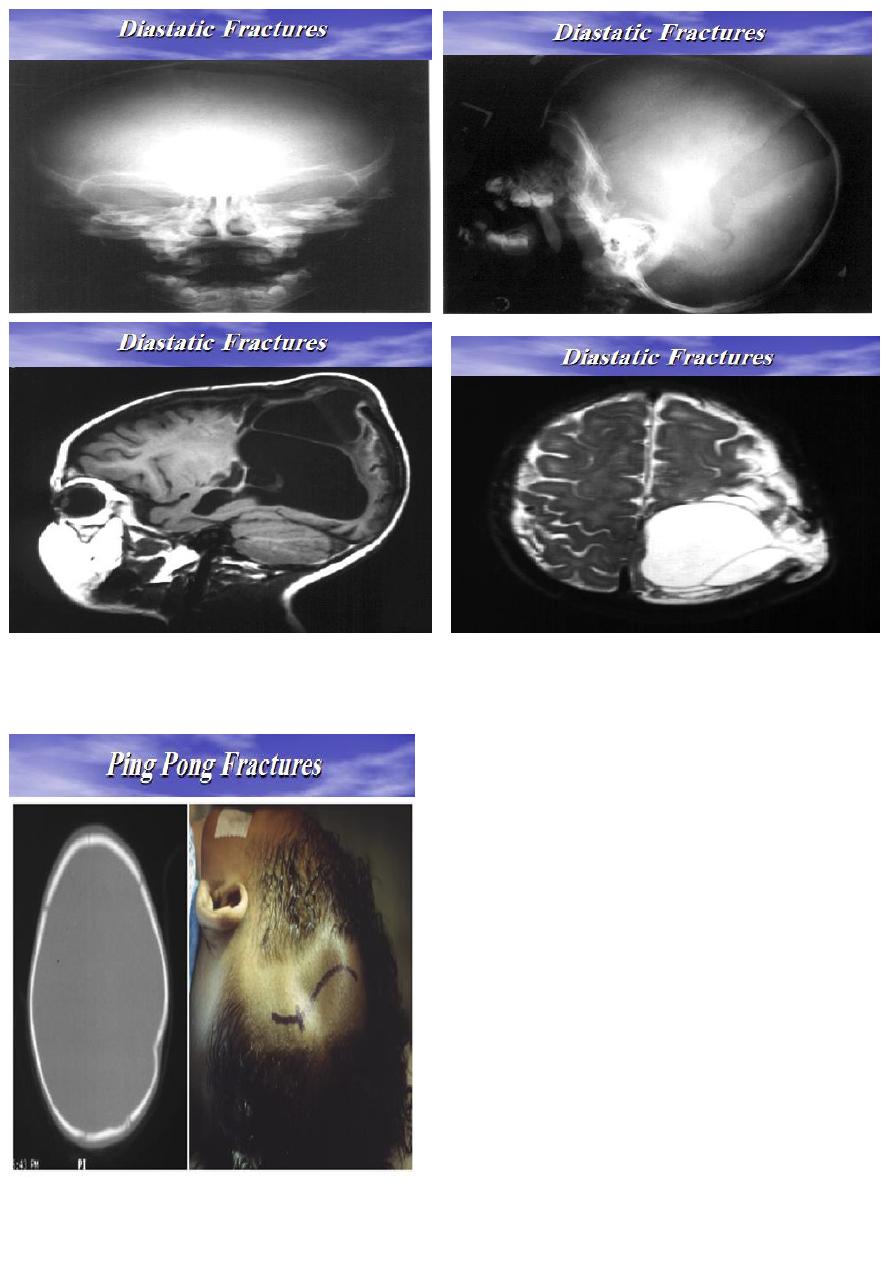
It is separation of a cranial suture line.
It involves the coronal or lambdoid suture.
Etiology : due to blunt trauma to the cranial vault.
Treatment :
• Fracture will elevate spontaneously if less than
3cm in diameter.
• If the fracture is more than 5cm in diameter, it
may need surgical elevation.
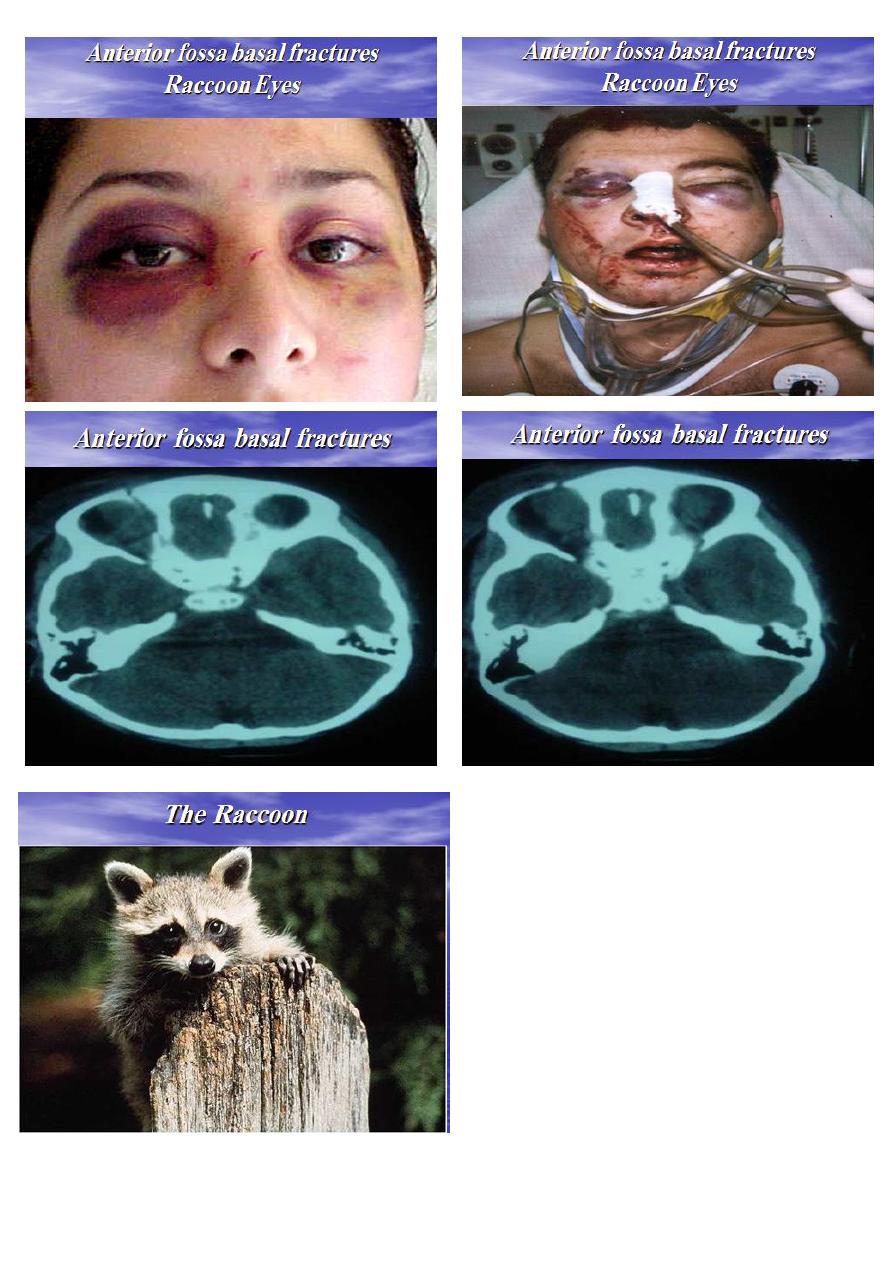
Anterior fossa basal fractures
May open into the frontal or ethmoidal air sinuses, or
run across the cribriform plate.
Clinical presentations:
1. Subconjuctival haematoma.
2. Epistaxis.
3. Anosmia: due to olfactory nerve injury.
4. CSF Rhinorrhoea.
5. Nasal tip parraesthesia: due to injury to the 1st
branch of 5th nerve.
6. Periorbital haematoma or ‘raccoon eyes’.
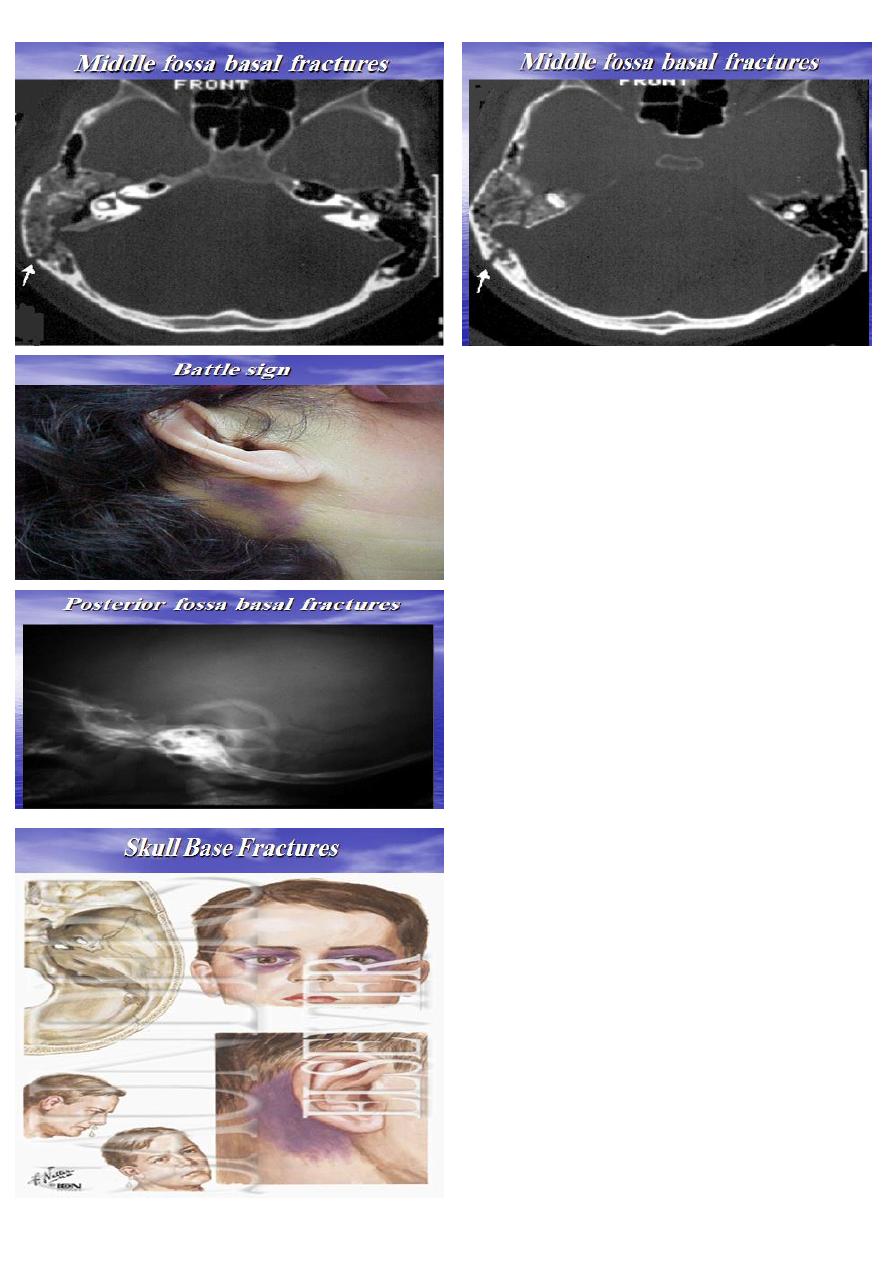
Middle fossa basal fractures
• Involve the pertrous temporal bone.
• Clinical presentations:
1. CSF Otorrhoea.
2. Haemotympanum.
3. Battle sign; discoloration over the
mastoid process.
4. VII and VIII cranial nerve palsies.
Posterior fossa basal fractures
1. Boggy swelling or discoloration at the neck due to
extravasations of blood in the suboccipital region.
2. Injury to cranial nerves: usually involve 9th, 10th, and
11th cranial nerves at the jugular foramen.
3. Retraction of the head and stiffness of the cervical
muscles due to upper cervical nerves irritation.
Etiology : indirect violence on the vault producing
deformation of skull
The essential features of base of skull fractures
1. Escape of cranial contents, e.g. blood, CSF, or
brain matter.
2. Injury of cranial nerves.
3. Signs of brain injury.
Diagnosed on clinical examination.
Management of skull base fractures
1. Prevention of infection: prophylactic antibiotics.
2. Control of CSF leakage: conservative or surgical
intervention.
3. Treatment of associated brain injury.
Indications for surgery
rhinorrhoea more than 10 days , meningitis.
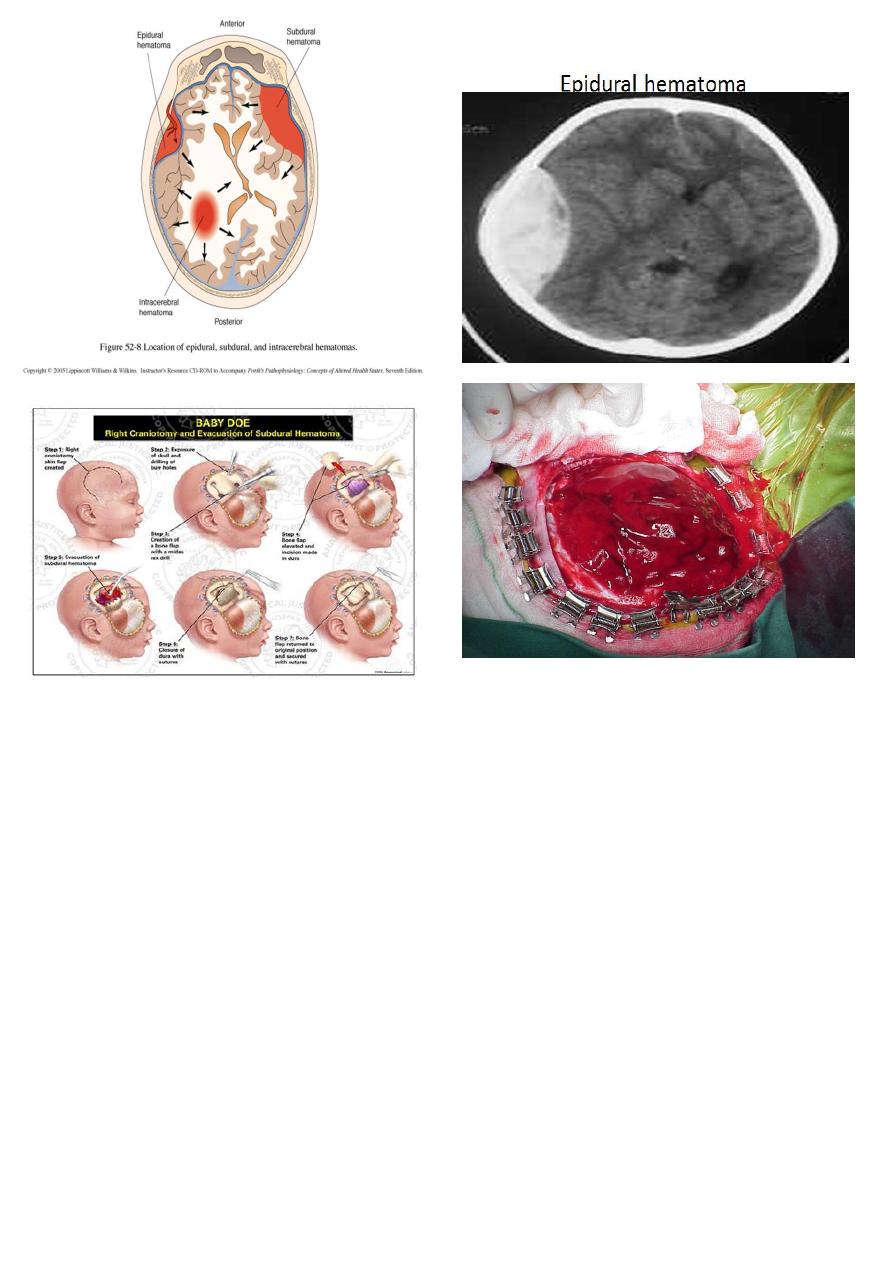
Etiology: Temporoparietal depressed fracture can
disrupt the middle meningeal arterythrough its bony
groove within pterion causing bleeding that dissect
dura from the inner table
Clinical Picture:
1. Stage of concussion: brief period of loss of
consciousness.
2. Stage of lucid interval: patient recover from
concussion, blood will accumulate gradually in the
extradural space.
3. Stage of compression: shown clinically as:
Gradual progressive deterioration in the level of
consciousness.
Contralateral hemiparesis due to cortical
compression.
Tentorial herniation, with compression of
oculomotor nerve, with dilatation of ipsilateral
pupil.
Source of bleeding:
((middle meningeal artery, middle meningeal vein ,
dura venous sinuses))
Investigation : CT scan will show biconvex or lens
shaped hyperdense lesion due to adherence of the
dura to the inside of the cranium at the sites of sutures.
Treatment : Surgical treatment by evacuation of
haematoma via Emergency Craniotomy.
Note : An extradural haematoma is a neurosurgical
emergency that will result in death if the haematoma
is not removed promptly.
Acute Subdural hematoma
Etiology : Usually due to MORE SEVERE injury with a
poorer outcome.
Source of bleeding (haematoma): include:
• Most result from tears of a cortical artery.
• Cortical lacerations or contusions.
• Bleeding from tears in the dural venous sinuses.
• Clinical Picture: patient will present with a picture
similar to that of an extradural haematoma, but there is
persistent loss of consciousness with no lucid interval.
INVESTIGATION : CT scan will show a :
crescent hyperdence collection because blood follows the
subdural space over the convexity of the brain.
Treatment : early evacuation via craniotomy is
mandatory.
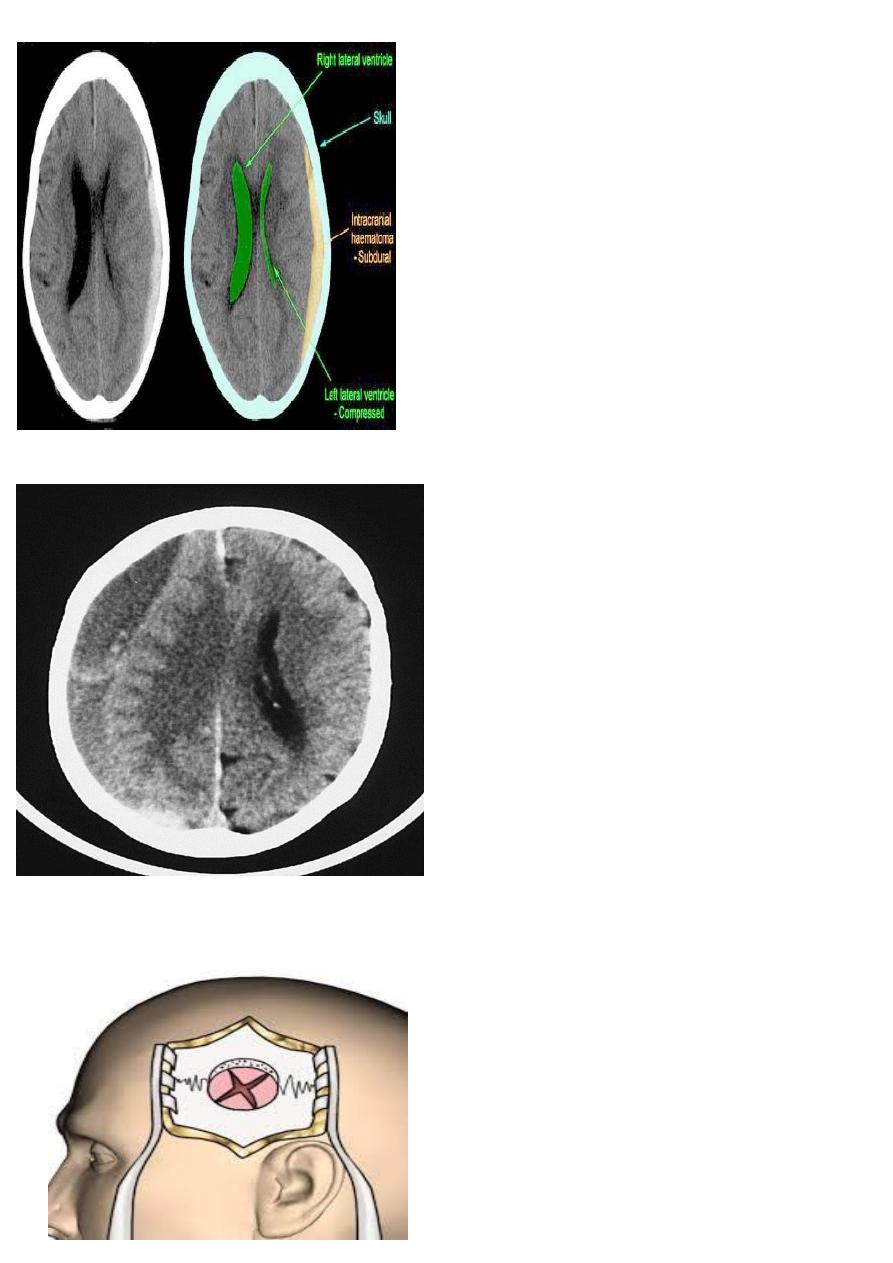
Chronic subdural hematoma
ETIOLOGY : secondary to SLIGHT blow to the head
which may pass unnoticed.
Source of bleeding (haematoma): usually from bridging
veins as they pass to the venous sinuses.
CLINICAL FEATURES :
progressive neurological deficits more than 3 weeks after
the trauma, or progressive headache , memory
disturbances.
INVESTIGATION :
CT scan: the acute clotted blood is initially appears white
(hyperdence), but as it liquefies, it slowly becomes black
(hypodense).
TREATMENT :
They should be drained if they continue to enlarge.
They are evacuated by drilling burrholes over the
collection and washing it out with warmed saline.
Subarachnoid Haemorrhage (SAH)
ETIOLOGY : Trauma is the commonest , aneurysm.
RX : Traumatic SAH is managed conservatively
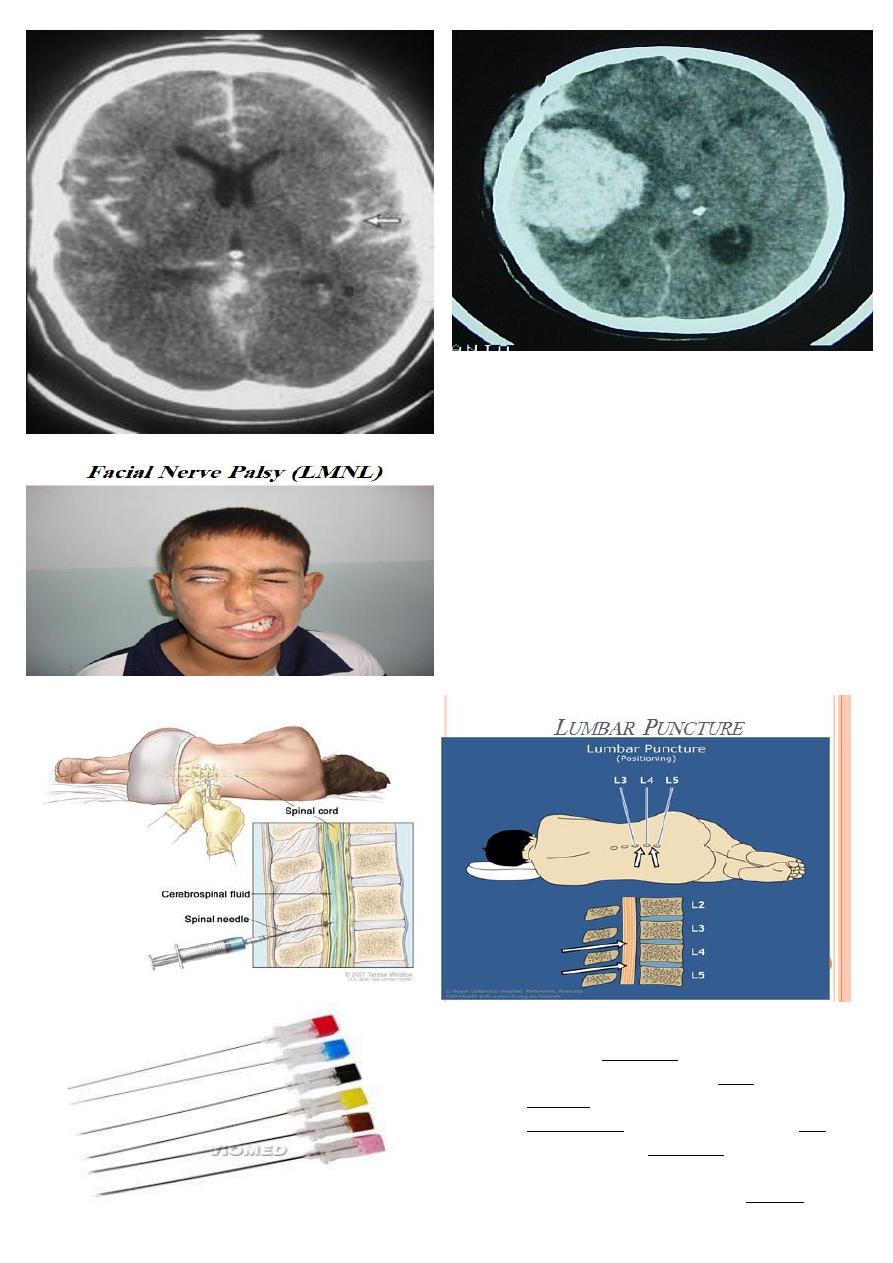
NO LOSS OF SKIN SENSATION
SYMPTOM :
loss of taste, hyperacusis, decrease of salivation and
tears secretion
Lumbar Puncture Indications
1. suspected meningitis
2. subarachnoid hemorrhage SAH
3. cytology in neoplastic diseases
4. measurement of intracranial pressure ICP
5. therapeutic CSF aspiration (benign raised
intracranial pressure)(pseudotumor cerebri).
6. conventional myelography by contrast injection
7. Spinal anesthesia.
Contraindications to Lumbar Puncture
1. raised intracranial pressure.
Features of raised ICP are
1. focal neurological deficit
2. recent seizure
3. papilloedema.
2. Sepsis
3. Bleeding tendency like coagulopathy
4. Abnormal respiration i.e. moribund patient
5. Vertebral deformities ( kyphosis and scoliosis)
Complications of lumbar puncture
1.
2. Cerebellar tonsillar herniation if raised ICP.
3. Injury to the neural structure
4. Back pain
5. infection and meningitis
6. Bleeding
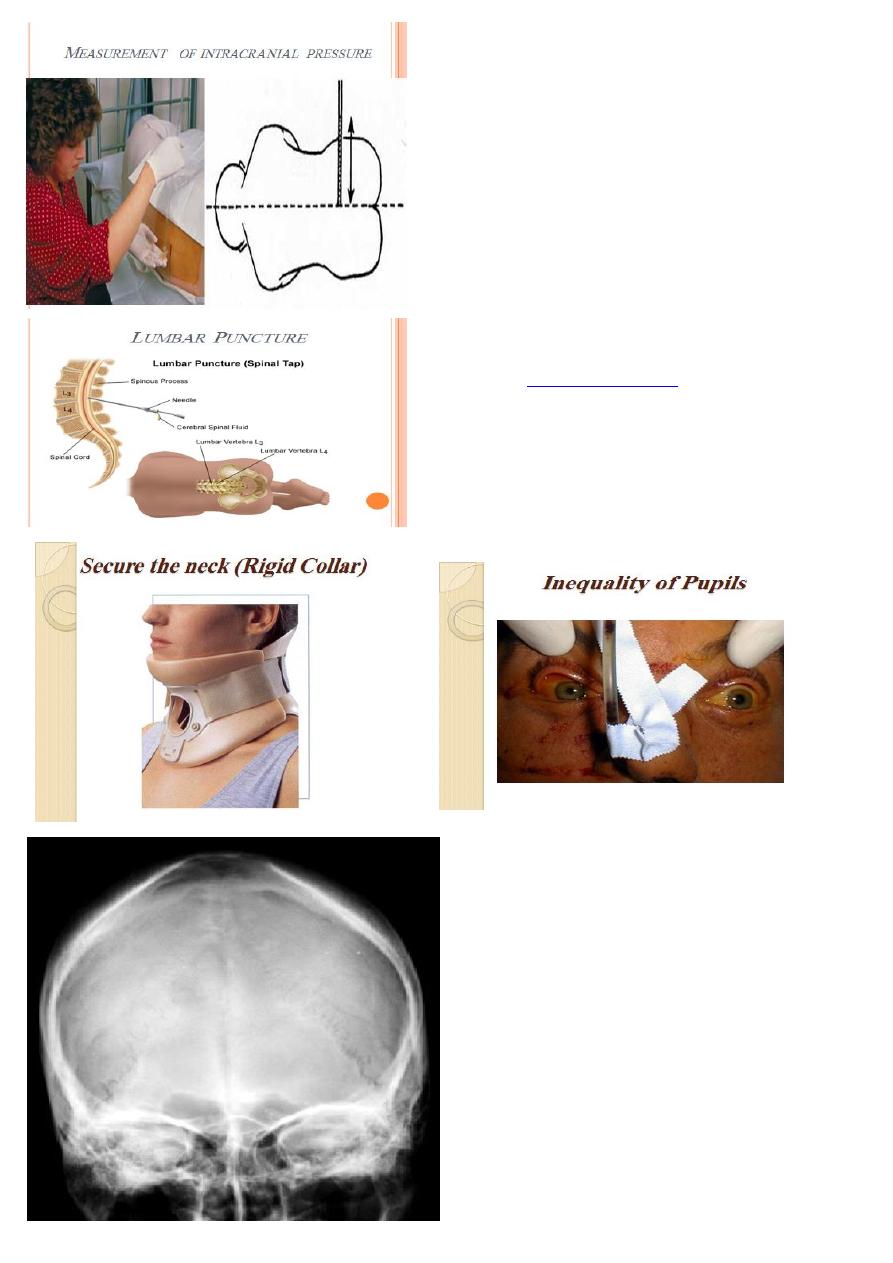
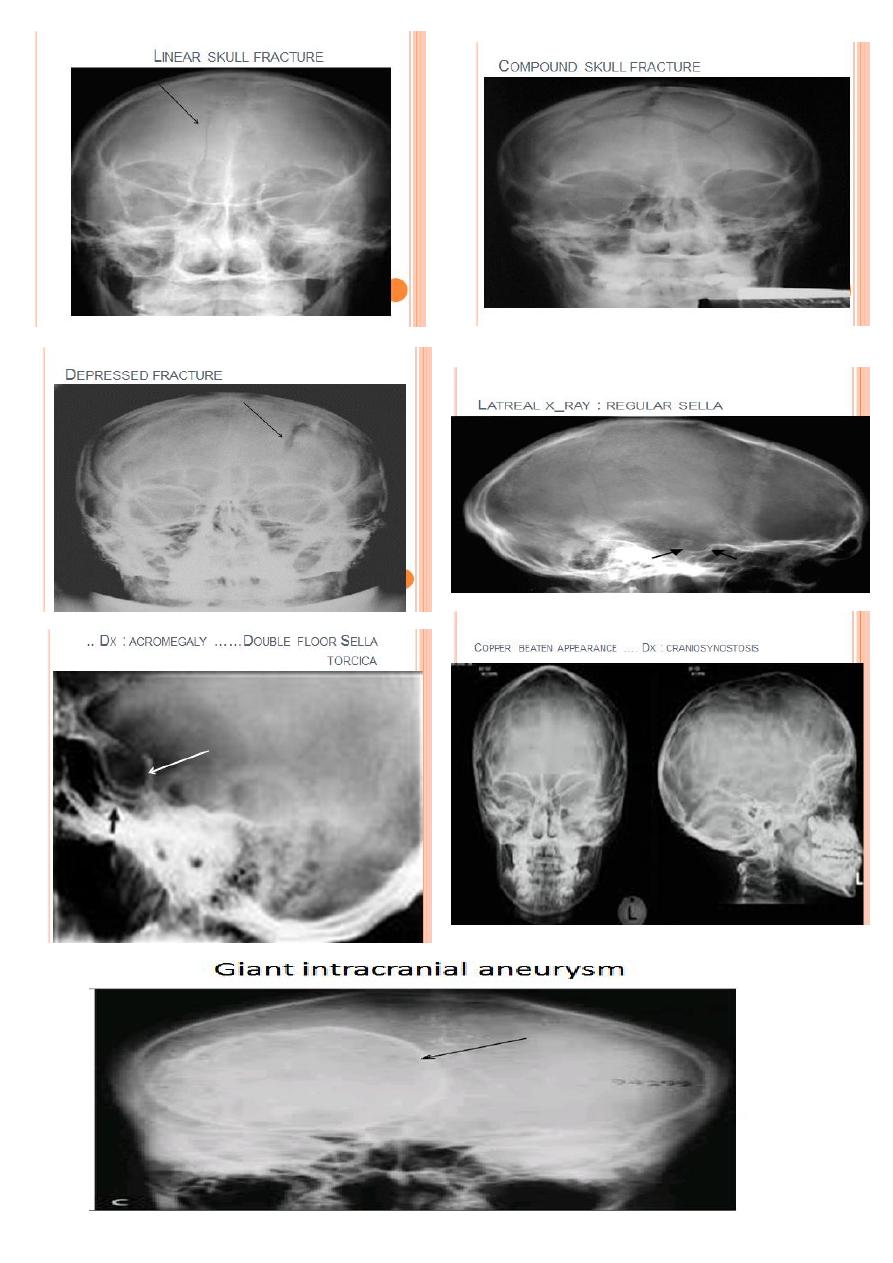
NORMAL SKULL X-RAY
The major abnormalities to look for on a skull X-ray
are:
1. Fractures linear and depressed
2. Hyperostosis, e.g. meningioma.
3. Bone erosion due to skull vault tumours.
4. Abnormal calcification, e.g. tumours such as
meningioma, oligodendroglioma,
craniopharyngioma or calcified wall of an
aneurysm.
5. Signs of long-standing raised intracranial pressure
erosion of the dorsum sellae
Double floor sella torcica
copper beating appearance of the skull vault.
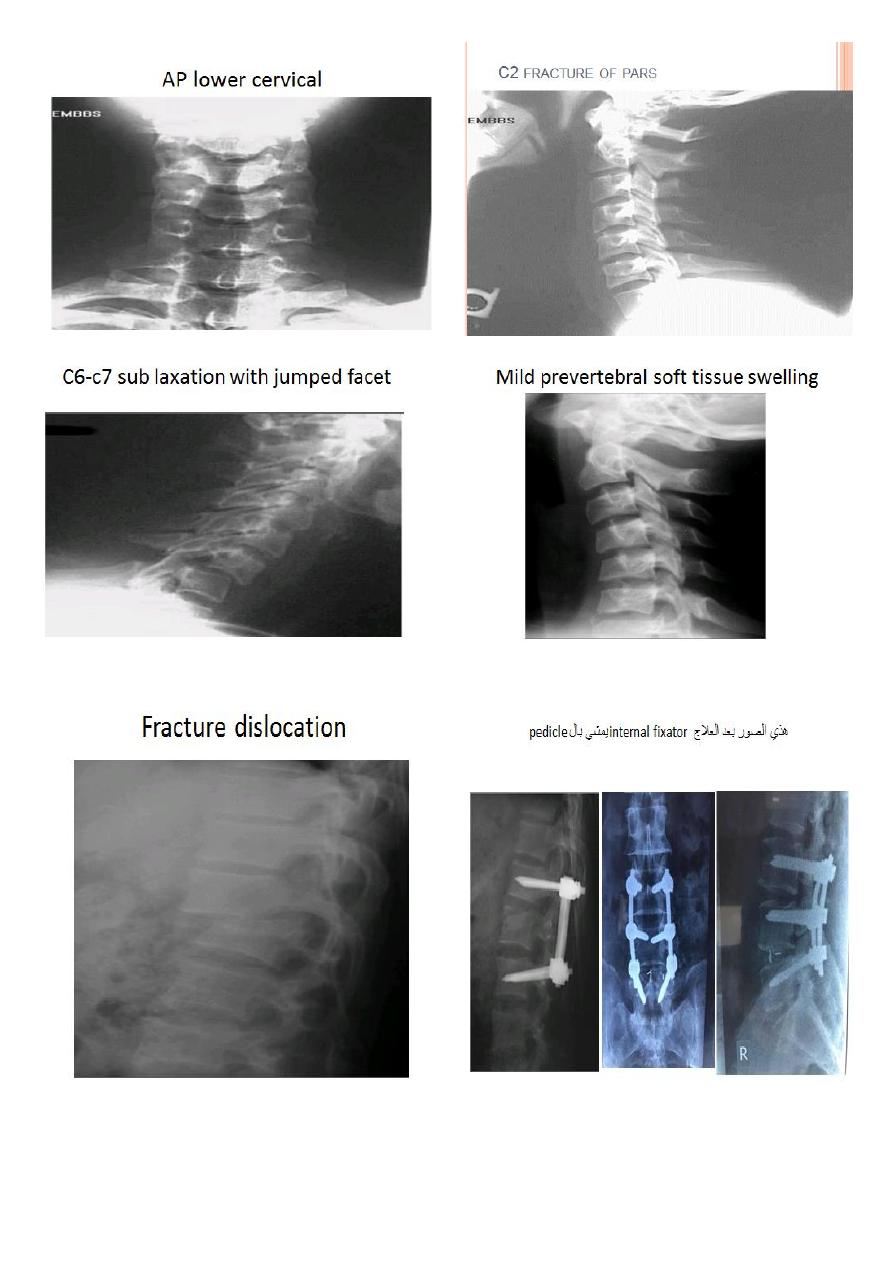
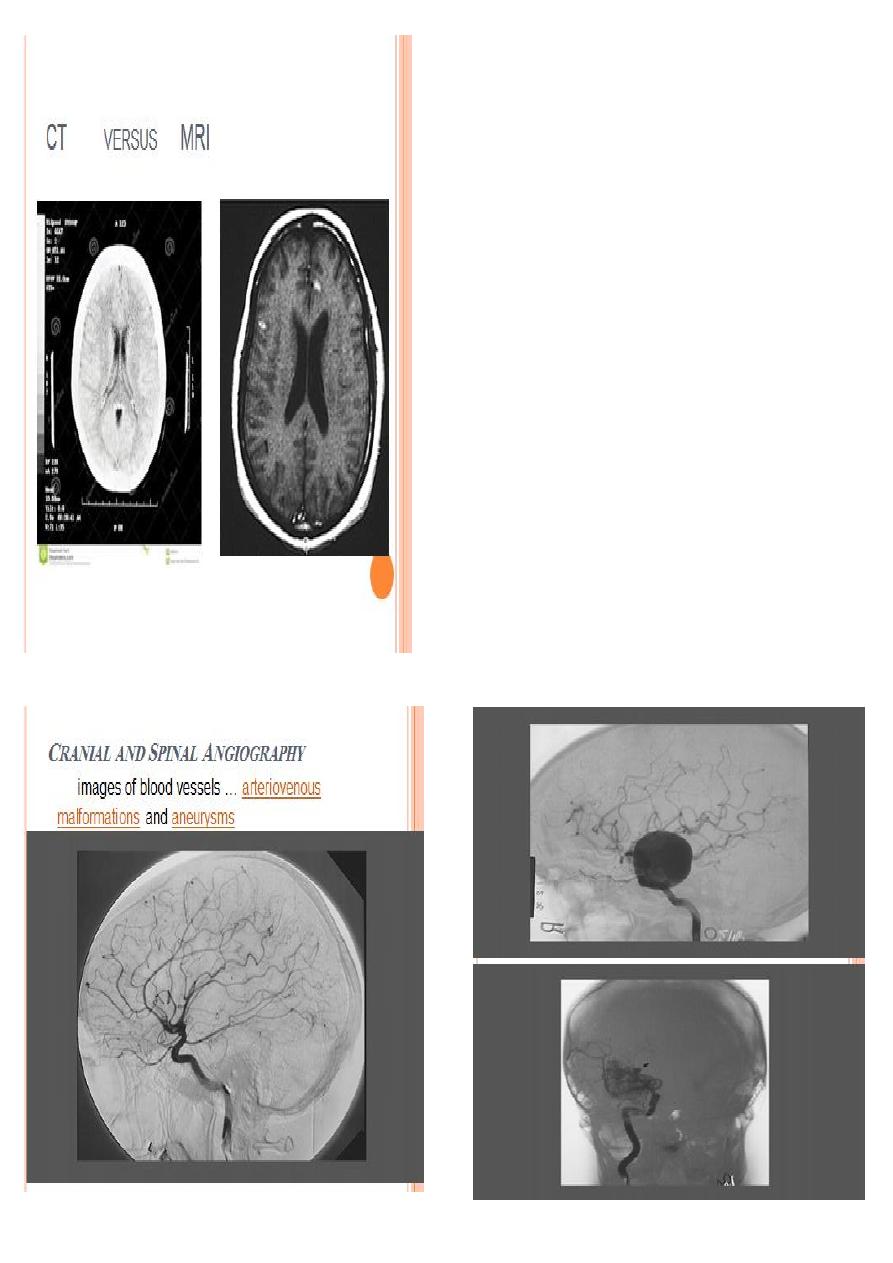
Indications for Computed Tomography in Neurosurgery:
Cranial CT:
1- Diagnosis of acute neurosurgical lesions in the head
and spine, including:
• Skull and spinal fractures.
• Intracranial hemorrhage: like extradural
haematoma
2- Oedema: brain oedema
3- Mass lesions:
4- Hydrocephalus
5- Stroke: differentiate between infarction and
intracranial haemorrhage.
Indications for Magnetic Resonance Imaging
1. Intracranial tumous.
2. cerebral abscess.
3. Arteriovenous malformations.
4. Venous sinus thrombosis.
5. Spinal tumours.
Contraindications to MRI
1. Metallic foreign bodies anywhere in the body
like plating and screwing, cardiac pace maker .
2. Claustrophobia.
3. Gross obesity
4-Uncontrolled movement disorders (Parkinson’s D)
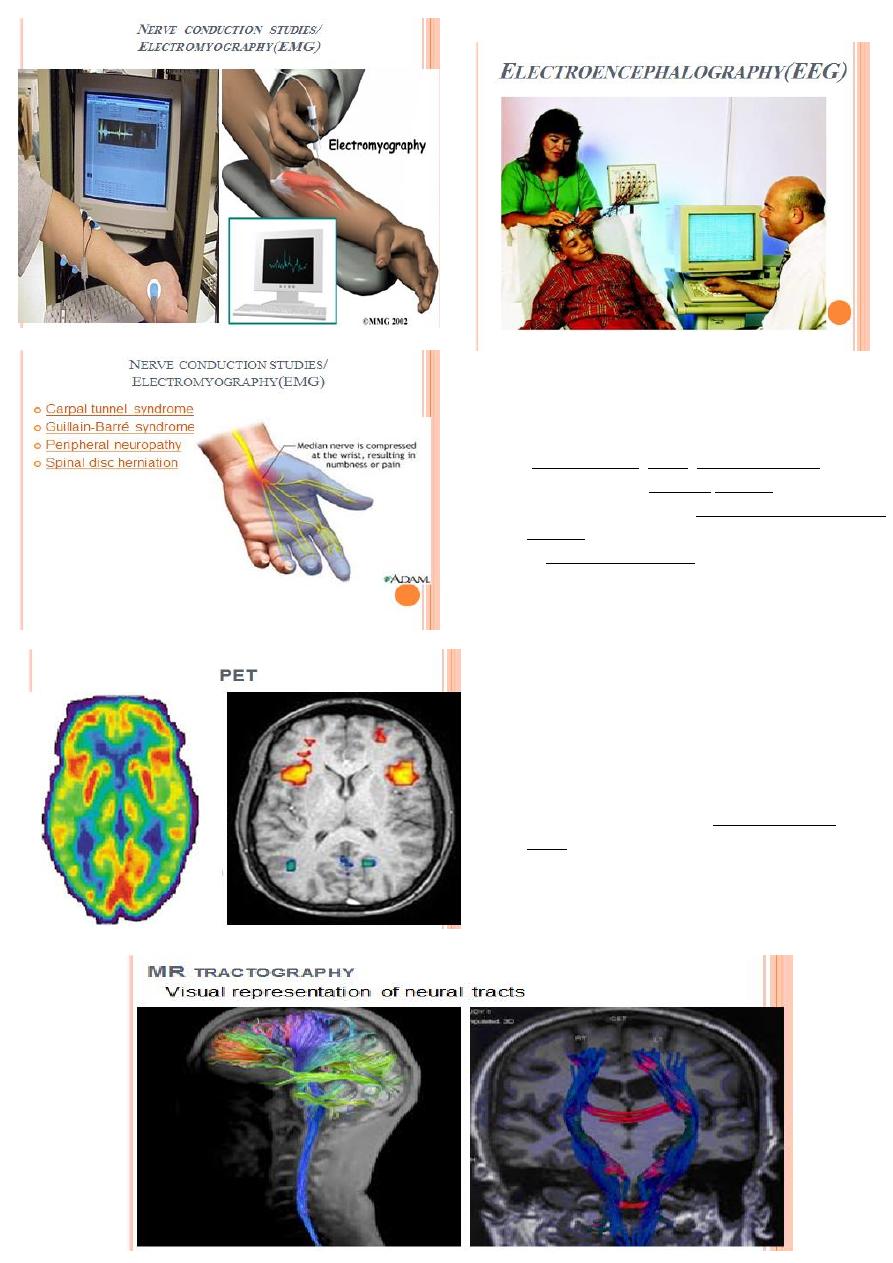
INDICATION OF EEG
Diagnosis and follow up of epileptic patients with
seizure focus localization
sleep disorders, coma, encephalopathies.
To differentiate epileptic seizures from other
types of spells, such as psychogenic non-epileptic
seizures
to characterize seizures for the purposes of
treatment
PET
A positron emission tomography (PET) scan is an
imaging test that can map tissue biochemistry and
physiology i.e functional test
The most commonly used PET tracer being a
labeled form of glucose ( Fludeoxyglucose
(18F) (FDG).
Useful in differentiating ischemic from
neoplastic areas.
