Fifth Stage
Internal Medicine
Dr. Abbas / Lec . 10
1
EPILEPSY
A seizure (from the Latin sacire, "to take possession of") is a clinical manifestation
due to abnormal, excessive, hyper synchronous discharges from an aggregate of
central nervous system (CNS) neurons. life time risk is 5%
Epilepsy is the tendency to have unprovoked seizure. the incidence of epilepsy is
~0.3–0.5% in different populations throughout the world, and the prevalence of
epilepsy has been estimated at 5–10 persons per 1000
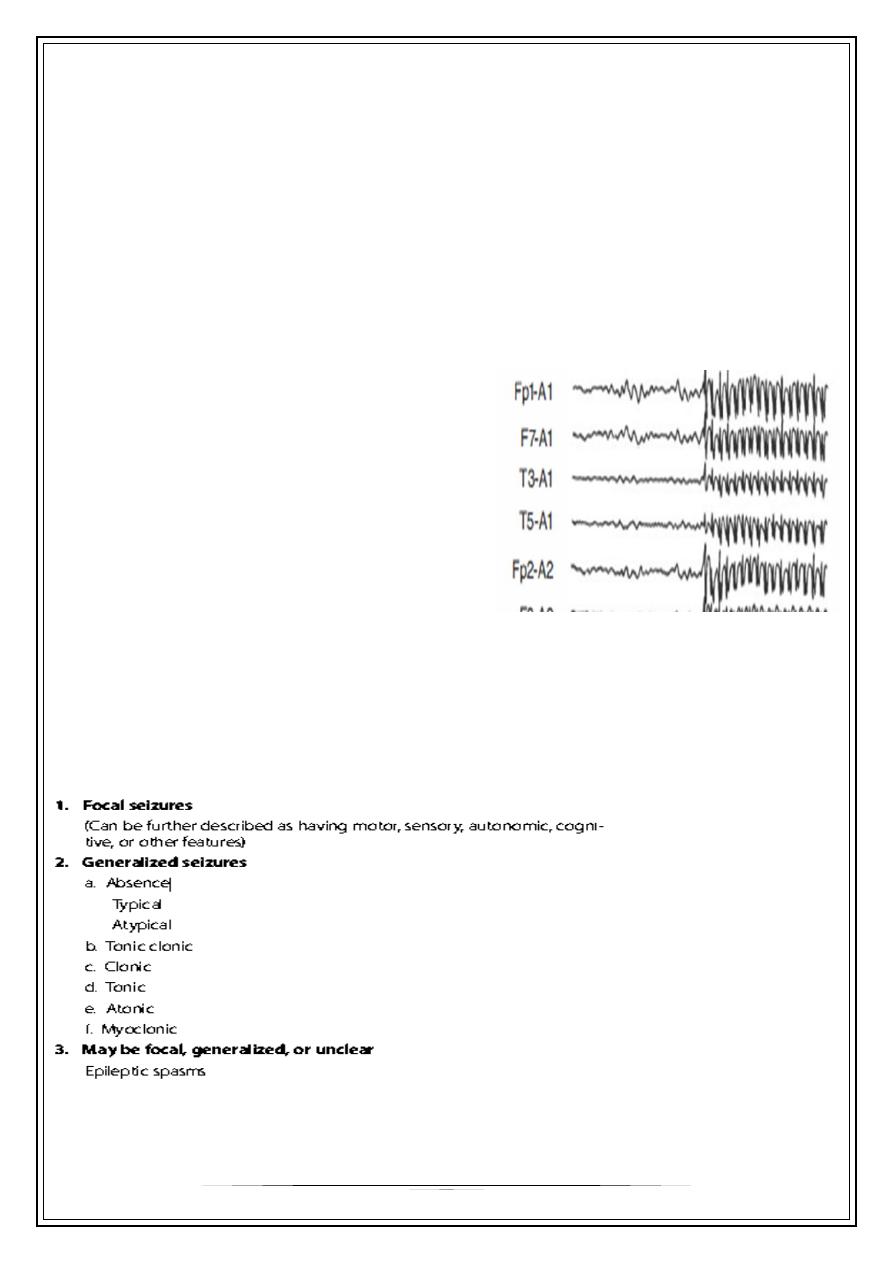
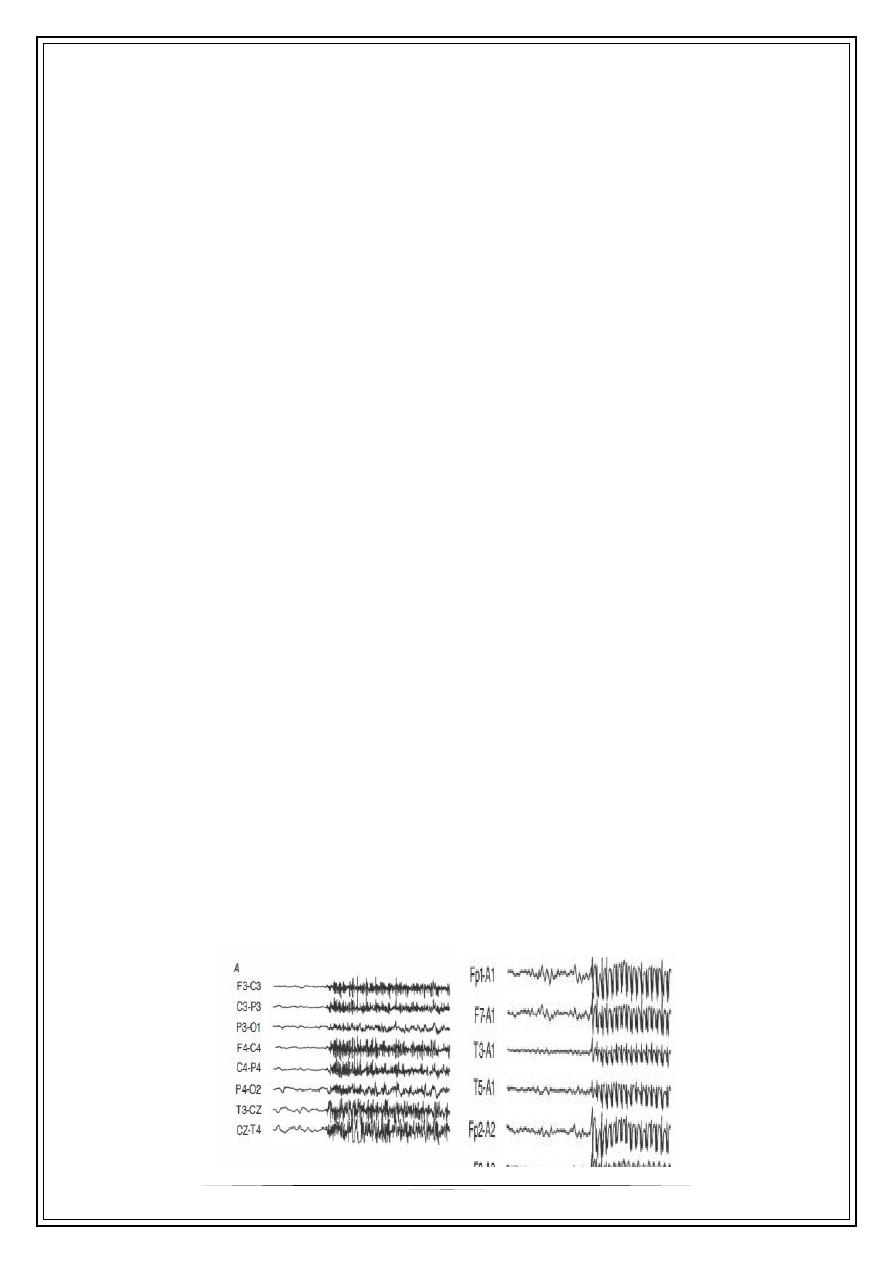
Mechanisms
During a seizure, large groups of neurons
are activated repetitively, unrestrictedly
and hyper synchronously. Inhibitory
synaptic activity between neurons fails.
Seizure results from an imbalance
between excitation and inhibition. This
produces high-voltage spike-and-wave
EEG activity, the electrophysiological
hallmark of epilepsy
Brain becomes epileptogenic either because neurons have a predisposition to be
hyper excitable, for example following abnormal neuronal migration patterns in
utero, or because the cells acquire this hyper excitable tendency. Trauma or brain
neoplasms are examples of acquired conditions that alter neuronal seizure
threshold .
Classification of epilepsy
2
Focal seizure subdivide into
1-without impairment of consciousness or awareness
2-with impairment of consciousness or awareness
3-evolving to a bilateral ,convulsive seizure
Tonic-clonic seizure
Following a vague warning, the tonic phase commences. The body becomes rigid,
for up to a minute. The patient utters a cry and falls, sometimes suffering serious
injury. The tongue is usually bitten. There may be incontinence of urine or faeces .
The clonic phase then begins, a generalized convulsion, with frothing at the mouth
and rhythmic jerking of muscles. This lasts from a few seconds to several minutes.
Seizures are usually self-limiting, followed by drowsiness, confusion or coma for
several hours .
Typical absences (petit mal)
This generalized epilepsy almost invariably begins in childhood. Each attack is
accompanied by 3 Hz spike-and-wave EEG activity
Activity cease, the patient stares and pales slightly for a few seconds. The eyelids
twitch; a few muscle jerks may occur. After an attack, normal activity is resumed.
Typical absence attacks are never due to acquired lesions such as tumors
They are a developmental abnormality of neuronal control.
Children with typical absence attacks tend to develop generalized tonic-clonic
seizures in adult life (known as primary generalized epilepsy))
Petit mal:
describes only these 3 Hz absence seizures. Clinically similar absence attacks are
also caused by partial seizures of temporal lobe origin, a source of some
confusion .
Other generalized seizure types
•
Myoclonic
o
seizures describe isolated muscle jerking.
•
Tonic
o
seizures describe intense stiffening of the body not followed by convulsive
jerking .
•
Atonic
o
seizures cause sudden loss of tone, with falling and loss of consciousness .
3
Focal seizures
focal seizure (simple or complex, implies that an area of brain (e.g. a temporal
lobe) has generated abnormal electrical activity. The seizure frequently has
clinical features that provide evidence of its site.
An aura describes the effects of initial focal electrical events, such as an unusual
smell, tingling in a limb or a strange inner feeling often recognized as a warning of
an impending seizure .
Jacksonian, or focal motor seizures
These simple focal seizures originate in the motor cortex.
Jerking movements typically begin at the angle of the mouth or in the hand, spreading
to involve the limbs on the side opposite the epileptic focus. Clinical evidence of this
spread of activity is called the march.
TEMPORAL LOBE SEIZURES
•
Medial temporal
•
Aura (70–90%): epigastric sensation, déjà vu, emotions, indescribable feelings
•
Arrest of activity (30–50%)
•
Simple automatisms at onset; complex later, usually ipsilateral to the region
where the seizure began
•
Later, contralateral tonic motor activity secondary to spread of seizure activity—
usually to the arm
•
Confusion
•
Consciousness may be preserved
•
Lengthy (1–3 minutes)
Aetiological and precipitating factors in epilepsy
1-Genetic predisposition
2-Developmental, e.g. hamartomas, neuronal migration abnormalities
3-Trauma and surgery
4-Pyrexia
5-Intracranial mass lesions, e.g. tumour, neurocysticercosis
6-Vascular, e.g. cerebral infarction, arteriovenous malformation
7-Drugs and drug withdrawa
4
8-lEncephalitis and inflammatory conditions
9-Metabolic abnormalities, e.g. porphyria, hypocalcaemia
10-Neural degenerative disorder
Provoked seizures, e.g. photosensitivity, sleep deprivation1
Brain tumours (and abscesses]
I.e. Mass
Lesions in the cortex cause epilepsy - either partial or secondary generalized
seizures. If epilepsy develops in adult life, the chance of finding an unsuspected
tumour is around 3% .
Vascular
Seizures sometimes follow cerebral infarction, especially in the elderly - there is a
peak in incidence late in life. A brain arteriovenous malformation may present with
seizures and occasionally a subarachnoid
Diagnosis
Accurate diagnosis is the cornerstone of treatment. The diagnostic evaluation has
three objectives: (1) to determine if the patient has epilepsy; (2) to classify the
seizures and type of epilepsy accurately and determine if the clinical data fit a
particular epilepsy syndrome; and (3) to identify, if possible, a specific underlying
cause
Electroencephalography
The EEG may help to establish a diagnosis and characterise the type of epilepsy
(i.e. primary generalised or partial with or without secondary generalisation).
Inter-ictal records are abnormal in only about 50% of patients so the EEG is not a
sensitive test for the presence or absence of epilepsy. However, 'epileptiform
changes' (sharp waves or spikes) are fairly specific (falsely positive in 1/1000 .)

5
Epileptic nature of attacks?
Ambulatory EEG
Videotelemetry
Type of epilepsy?
Standard EEG
Sleep EEG
EEG with special electrodes (foramen ovale, subdural
CT and/or MR imaging
Indications for brain imaging in epilepsy:
Epilepsy starts after the age of 16 years
Seizures have focal features clinically
EEG shows a focal seizure source
Control of seizures is difficult or deteriorates
The trend is towards sophisticated imaging of all new cases of epilepsy when
resources permit. In practice, CT is a reasonable screening test for tumours in adults but
MR is used routinely if available .
Other
1-urea and electrolytes
2-liver function test
3-serum glucose
4-serum calcium.magnesium
5-chest x-ray
6-CBC,ESR , C-reactive protein
7-Serology for HIV ,collagen disease
8-CSF examination
6
Treatment
Emergency measures
When faced with a seizure it is best simply to ensure that the patient comes to as
little harm as possible, and that the airway is maintained both during a prolonged
seizure and in postictal coma. Wooden mouth gags, tongue forceps and physical
restraint cause injury
Most seizures last only minutes and end spontaneously. A prolonged seizure -
longer than 3 minutes - or repeated seizures outside hospital are best treated with
rectal diazepam (10 mg), or intravenous diazepam. If there is any suspicion of
hypoglycaemia, take blood for glucose and give i.v. glucose. Serial epilepsy
describes repeated seizures with brief periods of recovery. These may lead to
status epilepticus. Sudden death in a seizure
Focal status
also occurs. In absence status, for example, status is non-convulsive - the patient
is in a continuous, distant, stuporose state.
Epilepsia partialis continua:
is continuous seizure activity in one part of the body, such as a finger or a limb,
without loss of consciousness. This is often due to a cortical neoplasm or, in the
elderly, a cortical infarct .
Thank you,,,



