Abdominal Trauma
INTRODUCTION7-10 % of hospital admissions
20 % of all trauma surgeries
¾ is attributable to RTA.
2/3 occur in males with a peak incidence in age 14 – 30 yrs..
Penetrating injury has a higher mortality of up to 12%and accounts for 1/3rd of all abdominal trauma.
Gunshot and stab wounds account for 90% of penetrating trauma.
Penetrating injury has a higher mortality of up to 12%and accounts for 1/3rd of all abdominal trauma.
50 % of preventable trauma death are related to inappropriate management of abdominal trauma
Abdominal injuries should be suspect in all trauma patients.
CLASSIFICATIONAbdominal Trauma
PenetratingHigh velocity (85% penetrate peritoneum)
Low velocity (95% need surgery)
Stab(1/3 do not penetrate the peritoneum, of those 50% need Sx)
Blunt trauma
High energy transfer (car accident)
Low energy transfer (fall, fight)
Blunt Injury
Spleen 25%
Liver 15%
Hollow viscus 15%
Ileum
Sigmoid
Kidney 12%
Retroperitoneal 13%
Mesentery 5%
MECHANISMS OF INJURY
• Compression
• Crushing
• Shearing
• Avulsion
Abdominal Trauma EvaluationPrimary survey
Initial assessment and resuscitation. Initial examination and resuscitation should be simultaneous.Principles of ABC should be applied ie adequate airway,breathing and treating hypovolumia.
Insert wide bore IV cannula.
Initial fluid resuscitation; rapid infusion of 2 litres of crystalloid solution followed by colloids if necessary.
Continous monitoring of BP,pulse rate , oxygen saturation.
Rule out other injuries.
Abdominal Trauma Evaluation Secondary survey
AMPLE
Mechanism
RTA:
Speed
Type of collision (frontal, lateral, sideswipe, rear, rollover)
Vehicle intrusion into passenger compartment
Types of restraints
Deployment of air bag
Patient's position in vehicle
• A.M.P.L.E. - a simple mnemonic for keyinformation
A: allergies (e.g. penicillin or aspirin)
M: medication (e.g. a beta-blocker or warfarin)
P: previous medical history (e.g. previous surgery or anaesthetic mishap)
L: last mealtime (i.e. drink versus major meal)
E: events surrounding the incident (e.g. fell 5 metres with immediate loss of consciousness)
Examine each body region meticulously
Abdominal Trauma Evaluation Secondary survey
Physical examinationBruises, abrasion over the abdomen(Seat belt mark)
Abdominal pain or tenderness
Absent bowel sounds
Auscultation
Palpation
Rebound tenderness
Guarding
Pregnancy
Pelvic instability
Abdominal Trauma Evaluation Secondary survey
Rectal examinationProstate
Rectal tone
Vaginal examination
Gluteal fold
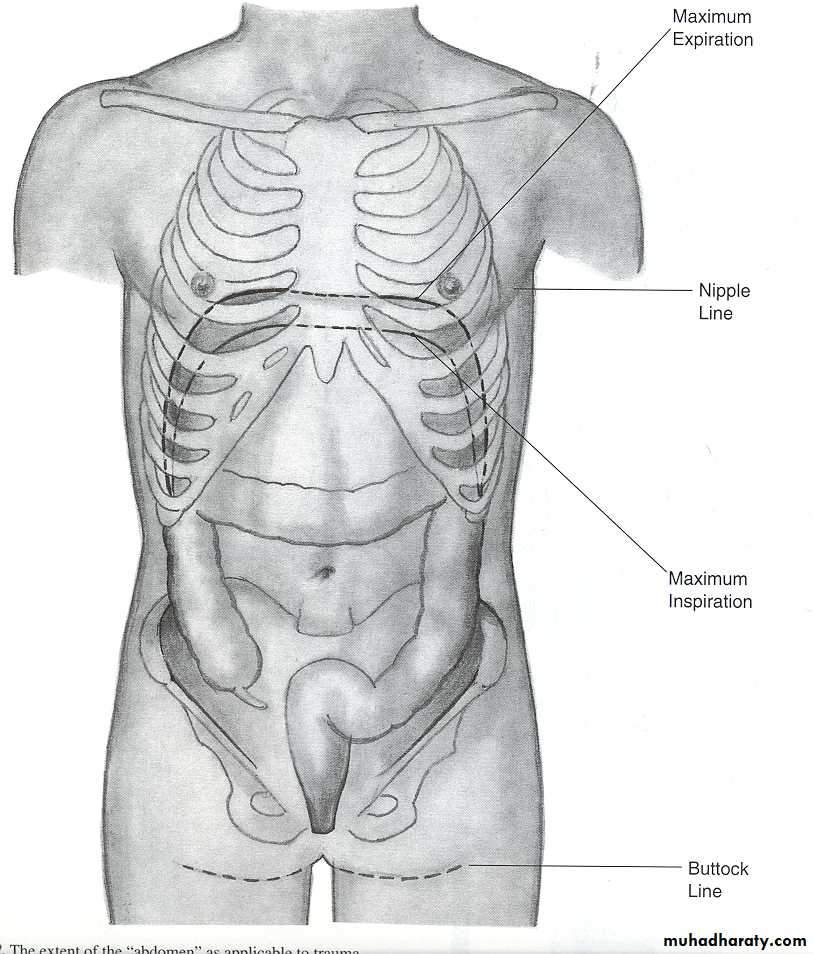
Penetrating injuries = abdominal injuries
Abdominal Trauma EvaluationTube Insertion
Urinary catheter• Monitor urinary output
• Caution
• Inability to void
• Pelvic fracture
• Blood at the meatus
• Scrotal Ecchymoses
• High riding prostate
• Gastric tube
• Relives distention• Decrease risk of unattended vomiting
• But can induce it , risk of aspiration !!!
• Caution
• Facial fracture
• basilar skull fracture
Abdominal Trauma Evaluation
Physical examination unreliable If:
Head trauma
Spinal cord injuries
Alcohol intoxication
Use of illicit drugs
Injuries to adjacent structure
Significant amount of blood present
Analgesia
Abdominal Trauma Evaluation Investigations
In haemodynamically stable patients.Full blood count ,haematocrit & BG.
Urea and electrolytes.
FAST (Focused Abdominal Sonography for Trauma)
DPL
CT abdomen and pelvis
Laproscopy
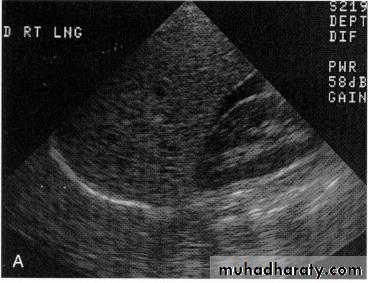
Focused Abdominal Sonography for Trauma FAST
• Detects free fluid in the peritoneal cavity. Non invasive and
rapid. 88% sensitive,99% specific and 97% accurate
• Demonstrate presence of free intraperitoneal fluid
• Evaluate solid organ hematomas• Advantages
• No risk from contrast media or radiation
• Rapid results, portability, non-invasive, ability to repeat exams.
• Disadvantages
• Cannot assess hollow visceral perforation
• Operator dependent
• Retroperitoneal structures are not visualized
FAST
Four View Technique:Morrison’s pouch (hepatorenal)
Douglas pouch (retropelvic)
Left upper quadrant (splenic view)
Epigastric (View pericardium)
Diagnostic peritoneal lavageDPL
• 98% sensitive in detecting intra abdominal bleeding.• Does not detect diaphragmatic injuries.
• Poor at detecting retroperitoneal bleed.• Invasive procedure.
• Positive criteria;RBC count >100,000/ul. WBC count > 500/ul.
Amylase > 175U/ml.
Presence of fecal matter - bile -10 mls blood .
DPL Contraindications
• Absolute :• Peritonitis ,unstable patient
• Injured diaphragm
• Extraluminal air by x-ray
• Significant intraabdominal injury by CT scan
• Intraperitoneal perforation of the bladder by cystography
• Relative :
• Previous abdominal operations (because of adhesions)
• Morbid obesity
• Gravid Uterus
• Advanced cirrhosis (because of portal hypertension and the risk of bleeding)
• Preexisting coagulopathy
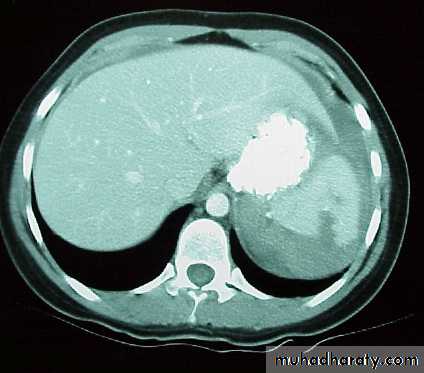
CT Scan
• Replacing DPL.
• 98% sensitive in detecting intraperitoneal bleeding.
• Contrast enhanced CT Scan gives useful anatomical and fuctional information on organs.
• Can identify organ injuries and be used to determine which injuries can be managed conservatively in stable patients.
• Useful in grading solid organ injuries(liver and spleen)..
Laparoscopy
• Increasingly used in assessing trauma.• Useful in determining peritoneal penetration and identifying diaphragmatic injuries.
• Also can be used for treating certain injuries.
Abominal Trauma TreatmentOutlines
A Abdominal traumabaaado
Gun shotGun shot
Stab woundBlunt abdominal trauma
Mandatory laparotomy
Evisceration ,positive DPL, Haemodynamic instabilty,peritonitis
Stable ; FAST,CTScan,DPL
Unstable haemodynamically
LAPAROTOMY
Others X-Ray Abdominal Trauma Evaluation
• Urethrography , cystography
• 5. ? IVP for hematuria
• IV contrast
• Keep good urinary output
• Better CT scan
• 6. Spine fracture
• Chance Fracture
Small Intestine InjuriesEpidemiology
15% of all laparotomyHigh index of suspicion required
Serial examination
DPL diagnostic in 95 %
Increasing success with CT and laparoscopy
Delay in diagnosis increase M & M
Spleen Injuries
20% of splenic injuries occur inadvertently during other abdominal operationsIn some patients spontaneous rupture can occur following trivial trauma
Spleen is invariably abnormal due to, for example, malaria or infectious mononucleosis
Spleen InjuriesClinical features
Clinical features depend on:
Degree of hypovolaemia
Presence of associated injuries
Clinical features range from left upper quadrant pain to shock and peritonitis
30 to 60% of patients have other assocaited intraperitoneal injuries
Spleen InjuriesDiagnosis
Blunt trauma chest and or abdominal traumaHemodynamic instability
LUQ pain-left lower ribs fractures
Left shoulder pain (positive kehr’s sign)
CT scan will save 70 % of spleens
Observation X 72 hr
Healing over 6 weeks
OPSI (overwhelming post Splenectomy infection)
< 1% of splenectomies , increased in children
Spleen InjuriesInvestigation
FAST U\S abdomen .D.P.L.x-ray plain ,enlargement of splenic shadow
CT abdomen
Grading
Grade 1 – Minor subcapsular tear or haematoma
Grade 2 – Parenchymal injury not extending to the hilum
Grade 3 – Major parenchymal injury involving vessels and hilum
Grade 4 – Shattered spleen
• Spleen InjuriesTreatment
If cardiovascularly unstable requires resuscitation and early surgery
If cardiovascularly stable consider either ultrasound or CT scan
Spleen InjuriesTreatment
Surgical optionsSurgical management can involve either splenectomy or splenic repair
Main benefit of retaining the spleen is the prevention of OPSI
If splenic conservation attempted need to preserve more than 20% of tissue
Spleen InjuriesTreatment
Indication for non operative -:Presentation >12 hour
Haemody namically stable.
No sign of abdominal injury
U\S, C.T follow up.
Close monotering.
Spleen InjuriesTreatment
Conservative management
Overall 20-40% of patients are suitable for conservative management
Children can often be managed conservatively as they have
Increased proportion of low grade injuries
Fewer multiple injuries
Should be monitored in high dependency unit
Require cardiovascular and haematological monitoring
Spleen InjuriesTreatment
If successful patients should remain on:Bed rest for 72 hours
Limited physical activity for 6 weeks
No contact sports for 6 months
Surgery needed if clinically hypovolaemic of they have a falling haematocrit
Approximately 30% of patients fail conservative management
Usually occurs within the first 72 hours of injury
Failed conservative management often results in splenectomy
What’s New in Abdominal Trauma
DiagnosticCt, U/S
Laparoscopy its impact is coming
Therapeutic
Nonoperative management
Spleen & liver
Non operative for liver gunshot
“Damage control” laparotomy
“Abdominal compartment syndrome”