1
بسم هللا الرحمن الرحيم
Lecture 9,10 Neurophysioloy Dr. Noor Jawad
2
nd
stage 2020
…………………………………………………………………….
Cerebral Blood Flow, Cerebrospinal Fluid, and
Brain Metabolism
Objective
1. What is the effect of Carbon Dioxide and Hydrogen Ions on
Cerebral Blood Flow?
2. Autoregulation of Cerebral Blood Flow When the Arterial
Pressure Changes?
Cerebral Blood Flow
Normal Rate of Cerebral Blood Flow
Normal blood flow through the brain of the adult person averages
50 to 65 milliliters per 100 grams of brain tissue per minute. For
the entire brain, this amounts to 750 to 900 ml/min, or 15 per cent
of the resting cardiac output.
Regulation of Cerebral Blood Flow
As in most other vascular areas of the body, cerebral blood flow is
highly related to metabolism of the tissue. At least three metabolic
factors have potent effects in controlling cerebral blood flow: (1)
2
carbon dioxide concentration, (2) hydrogen ion concentration, and
(3) oxygen concentration.
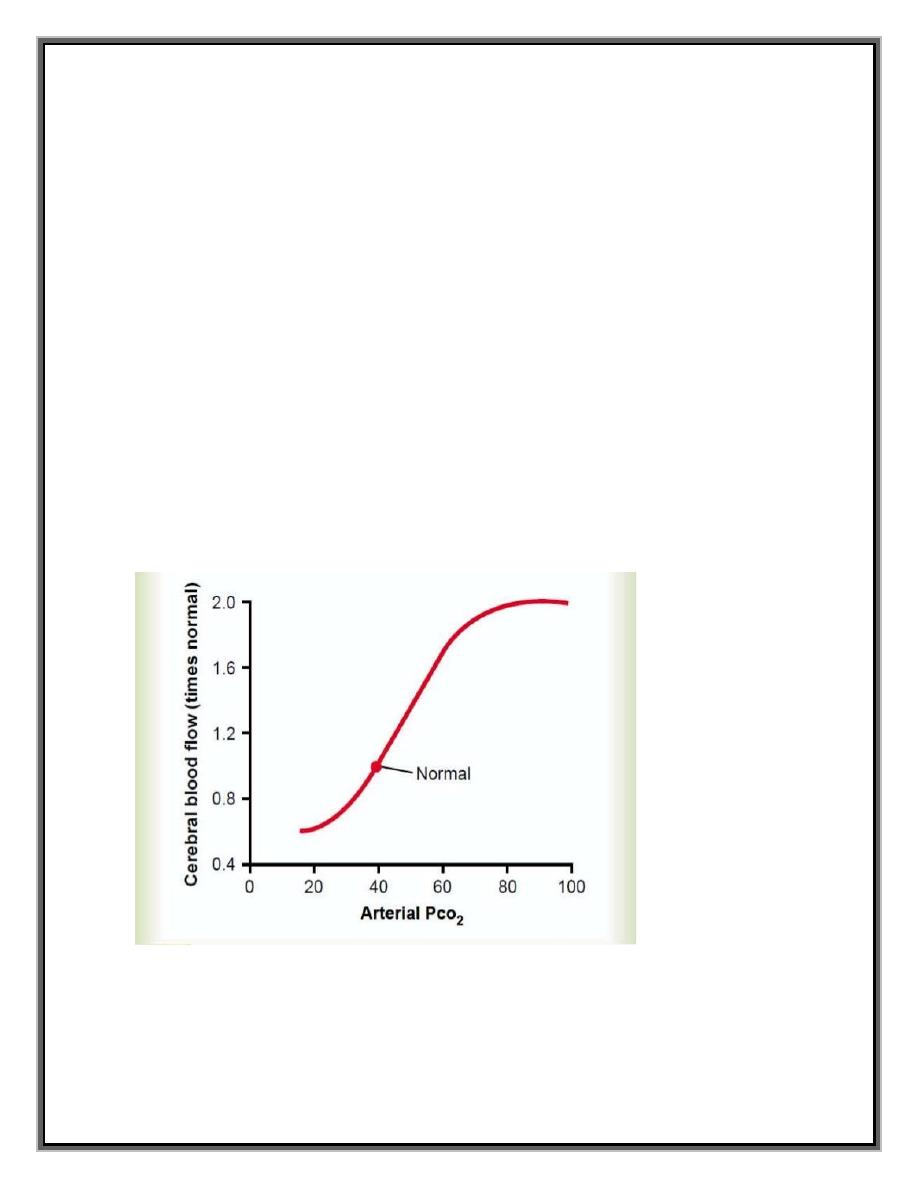
Increase of Cerebral Blood Flow in Response to Excess Carbon
Dioxide or Excess Hydrogen Ion Concentration.
An increase in carbon dioxide concentration in the arterial blood
perfusing the brain greatly increases cerebral blood flow. This is
demonstrated in Figure below, which shows that a 70 per cent
increase in arterial PCO2 approximately doubles cerebral blood
flow.
Figure show Relationship between arterial PCO2 and cerebral
blood flow
3
Carbon dioxide is believed to increase cerebral blood flow by
combining first with water in the body fluids to form carbonic acid,
with subsequent dissociation of this acid to form hydrogen ions.
The hydrogen ions then cause vasodilation of the cerebral
vessels—the dilation being almost directly proportional to the
increase in hydrogen ion concentration up to a blood flow limit of
about twice normal.
Any other substance that increases the acidity of the brain tissue,
and therefore increases hydrogen ion concentration, will likewise
increase cerebral blood flow. Such substances include lactic acid,
pyruvic acid, and any other acidic material formed during the
course of tissue metabolism.
Importance of Cerebral Blood Flow Control by Carbon
Dioxide and Hydrogen Ions.
Increased hydrogen ion concentration greatly depresses neuronal
activity. Therefore, it is fortunate that an increase in hydrogen ion
concentration also causes an increase in blood flow, which in turn
carries hydrogen ions, carbon dioxide, and other acidforming
substances away from the brain tissues. Loss of carbon dioxide
removes carbonic acid from the tissues; this, along with removal of
other acids, reduces the hydrogen ion concentration back toward
normal.
4
Thus, this mechanism helps maintain a constant hydrogen ion
concentration in the cerebral fluids and thereby helps to maintain a
normal, constant level of neuronal activity.
Autoregulation of Cerebral Blood Flow When the Arterial
Pressure Changes.
Cerebral blood flow is “autoregulated” extremely well between
arterial pressure limits of 60 and 140 mm Hg. That is, mean arterial
pressure can be decreased acutely to as low as 60 mm Hg or
increased to as high as 140 mm Hg without significant change in
cerebral blood flow. And, in people who have hypertension,
autoregulation of cerebral blood flow occurs even when the mean
arterial pressure rises to as high as 160 to 180 mm Hg.
Role of the Sympathetic Nervous System in Controlling
Cerebral
Blood Flow.
The cerebral circulatory system has strong sympathetic innervation
that passes upward from the superior cervical sympathetic ganglia
in the neck and then into the brain along with the cerebral arteries.
This innervation supplies both the large brain arteries and the
arteries that penetrate into the substance of the brain.
5
However, transection of the sympathetic nerves or mild to
moderate stimulation of them usually causes very little change in
cerebral blood flow because the blood flow autoregulation
mechanism can override the nervous effects.
Clinical points
Cerebral “Stroke” Occurs When Cerebral Blood Vessels Are
Blocked
Almost all elderly people have blockage of some small arteries in
the brain, and as many as 10 per cent eventually have enough
blockage to cause serious disturbance of brain function, a condition
called a “stroke.”
Most strokes are caused by arteriosclerotic plaques that occur in
one or more of the feeder arteries to the brain. The plaques can
activate the clotting mechanism of the blood, causing a blood clot
to occur and block blood flow in the artery, thereby leading to
acute loss of brain function in a localized area. One of the most
common types of stroke is blockage of the middle cerebral artery
that supplies the mid portion of one brain hemisphere.
6
Cerebrospinal Fluid System
.The entire cerebral cavity enclosing the brain and spinal cord has a
capacity of about 1600 to 1700 milliliters; about 150 milliliters of
this capacity is occupied by cerebrospinal fluid and the remainder
by the brain and cord.
Contents of CSF
The CSF is derived from blood plasma and is largely similar to it,
except that CSF is nearly protein-free compared with plasma and
has some different electrolyte levels. Owing to the way it is
produced, CSF has a higher chloride level than plasma, and an
equivalent sodium level.
CSF
contains
approximately 0.3%
plasma proteins, or
approximately 15 to 40 mg/dL, depending on sampling site. CSF is
normally free of red blood cells, and at most contains only a
few white blood cells. Any white blood cell count higher than this
constitutes pleocytosis.
Three Main Functions of CSF
CSF protects brain and spinal cord from trauma.
CSF supplies nutrients to nervous system tissue.
CSF removes waste products from cerebral metabolism.
7
Cushioning Function of the Cerebrospinal Fluid
A major function of the cerebrospinal fluid is to cushion the brain
within its solid vault. The brain and the cerebrospinal fluid have
about the same specific gravity (only about 4 per cent different), so
that the brain simply floats in the fluid. Therefore, a blow to the
head, if it is not too intense, moves the entire brain simultaneously
with the skull, causing no one portion of the brain to be
momentarily contorted by the blow.
Formation, Flow, and Absorption of Cerebrospinal Fluid
Cerebrospinal fluid is formed at a rate of about 500 milliliters each
day, which is three to four times as much as the total volume of
fluid in the entire cerebrospinal fluid system.
About two thirds or more of this fluid originates as secretion from
the choroid plexuses in the four ventricles, mainly in the two
lateral ventricles. Additional small amounts of fluid are secreted
by the ependymal surfaces of all the ventricles and by the
arachnoidal membranes.
The fluid secreted in the lateral ventricles passes first into the third
ventricle; then, after addition of minute amounts of fluid from the
third ventricle, it flows downward along the aqueduct of Sylvius
into the fourth ventricle, where still another minute amount of fluid
is added.
8
Finally, the fluid passes out of the fourth ventricle through three
small openings, two lateral foramina of Luschka and a midline
foramen of Magendie, entering the cisterna magna, a fluid space
that lies behind the medulla and beneath the cerebellum.
Secretion by the Choroid Plexus.
Secretion of fluid into the ventricles by the choroid plexus depends
mainly on active transport of sodium ions through the epithelial
cells lining the outside of the plexus .
The sodium ions in turn pull along large amounts of chloride ions
as well because the positive charge of the sodium ion attracts the
chloride ion’s negative charge. The two of these together increase
the quantity of osmotically active sodium chloride in the
cerebrospinal fluid, which then causes almost immediate osmosis
of water through the membrane, thus providing the fluid of the
secretion.
Cerebrospinal Fluid Pressure
The normal pressure in the cerebrospinal fluid system when one is
lying in a horizontal position averages 130 millimeters of water
(10 mm Hg), although this may be as low as 65 millimeters of
water or as high as 195 millimeters of water even in the normal
healthy person.
9
Regulation
of
Cerebrospinal
Fluid
Pressure
by
the
Arachnoidal Villi.
The normal rate of cerebrospinal fluid formation remains very
nearly constant, so that changes in fluid formation are seldom a
factor in pressure control. Conversely, the arachnoidal villi
function like “valves” that allow cerebrospinal fluid and its
contents to flow readily into the blood of the venous sinuses while
not allowing blood to flow backward in the opposite direction.
Then, if the cerebrospinal fluid pressure rises still higher, the
valves open more widely, so that under normal conditions, the
cerebrospinal fluid pressure almost never rises more than a few
millimeters of mercury higher than the pressure in the cerebral
venous sinuses.
Conversely, in disease states, the villi sometimes become blocked
by large particulate matter, by fibrosis, or by excesses of blood
cells that have leaked into the cerebrospinal fluid in brain diseases.
Such blockage can cause high cerebrospinal fluid pressure, .
Blood–Cerebrospinal Fluid and Blood-Brain Barriers
It has already been pointed out that the concentrations of several
important constituents of cerebrospinal fluid are not the same as in
extracellular fluid elsewhere in the body.
10
Furthermore, many large molecular substances hardly pass at all
from the blood into the cerebrospinal fluid or into the interstitial
fluids of the brain, even though these same substances pass readily
into the usual interstitial fluids of the body. Therefore, it is said
that barriers, called the blood–cerebrospinal fluid barrier and the
blood-brain barrier, exist between the blood and the cerebrospinal
fluid and brain fluid, respectively.
Barriers exist both at the choroid plexus and at the tissue capillary
membranes in essentially all areas of the brain parenchyma except
in some areas of the hypothalamus, pineal gland, where
substances diffuse with greater ease into the tissue spaces. The
ease of diffusion in these areas is important because they have
sensory receptors that respond to specific changes in the body
fluids, such as changes in osmolality and in glucose concentration,
as well as receptors for peptide hormones that regulate thirst, such
as angiotensin II.
The blood-brain barrier also has specific carrier molecules that
facilitate transport of hormones, such as leptin, from the blood into
the hypothalamus where they bind to specific receptors that control
other functions such as appetite and sympathetic nervous system
activity.
11
In general, the blood–cerebrospinal fluid and blood brain barriers
are highly permeable to water, carbon dioxide, oxygen, and most
lipid-soluble substances such as alcohol and anesthetics; slightly
permeable to electrolytes such as sodium, chloride, and potassium;
and almost totally impermeable to plasma proteins and most non–
lipid-soluble large organic molecules.
Brain Metabolism
Like other tissues, the brain requires oxygen and food nutrients to
supply its metabolic needs.
Total Brain Metabolic Rate and Metabolic Rate of Neurons.
Under resting but awake conditions, the metabolism of the brain
accounts for about 15 per cent of the total metabolism in the body,
even though the mass of the brain is only 2 per cent of the total
body mass. Therefore, under resting conditions, brain metabolism
per unit mass of tissue is about 7.5 times the average metabolism
in non–nervous system tissues.
Most of this excess metabolism of the brain occurs in the neurons,
not in the glial supportive tissues. The major need for metabolism
in the neurons is to pump ions through their membranes, mainly to
transport sodium and calcium ions to the outside of the neuronal
membrane and potassium ions to the interior.
12
Each time a neuron conducts an action potential, these ions move
through the membranes, increasing the need for additional
membrane transport to restore proper ionic concentration
differences across the neuron membranes. Therefore, during
excessive brain activity, neuronal metabolism can increase as
much as 100 to 150 per cent.
Special Requirement of the Brain for Oxygen—Lack of
Significant Anaerobic Metabolism.
Most tissues of the body can live without oxygen for several
minutes and some for as long as 30 minutes. During this time, the
tissue cells obtain their energy through processes of anaerobic
metabolism, which means release of energy by partially breaking
down glucose and glycogen but without combining these with
oxygen.
This delivers energy only at the expense of consuming tremendous
amounts of glucose and glycogen. However, it does keep the
tissues alive.
The brain is not capable of much anaerobic metabolism. One of the
reasons for this is the high metabolic rate of the neurons, so that
most neuronal activity depends on second-by-second delivery of
oxygen from the blood.
13
Putting these factors together, one can understand why sudden
cessation of blood flow to the brain or sudden total lack of oxygen
in the blood can cause unconsciousness within 5 to 10 seconds.
Under Normal Conditions Most Brain Energy Is Supplied by
Glucose.
Under normal conditions, almost all the energy used by the brain
cells is supplied by glucose derived from the blood. As is true for
oxygen, most of this is derived minute by minute and second by
second from the capillary blood, with a total of only about a 2-
minute supply of glucose normally stored as glycogen in the
neurons at any given time.
A special feature of glucose delivery to the neurons is that its
transport into the neurons through the cell membrane is not
dependent on insulin, even though insulin is required for glucose
transport into most other body cells.
Therefore, in patients who have serious diabetes with essentially
zero secretion of insulin, glucose still diffuses readily into the
neurons—which is most fortunate in preventing loss of mental
function in diabetic patients.
14
Yet, when a diabetic patient is overtreated with insulin, the blood
glucose concentration can fall extremely low because the excess
insulin causes almost all the glucose in the blood to be transported
rapidly into the vast numbers of insulin-sensitive non-neural cells
throughout the body, especially into muscle and liver cells.
When this happens, not enough glucose is left in the blood to
supply the neurons properly, and mental function does then
become seriously deranged, leading sometimes to coma and even
more often to mental imbalances and psychotic disturbances— all
caused by overtreatment with insulin.
Thank you
References : Guyton and Hall textbook of medical physiology,
thirteen edition
