IN THE NAME OF ALLAH
بسم الله الرحمن الرحيم
22/4/2020
Pulmonary eosinophilia
DefinitionPulmonary eosinophilia is a group of diseases with eosinophil cells–mediated pulmonary tissue damage and characterized by the association of radiographic (usually pneumonic) abnormalities and peripheral blood eosinophilia.
Classification
Extrinsic (cause knownIntrinsic (cause unknown)
Tropical pulmonary eosinophilia
Acute eosinophilic pneumonia:
Chronic eosinophilic pneumonia:
Eosinophilic granulomatosis with polyangiitis (formerly Churg-Strauss syndrome)
Case-studies
A 65-year-old man presents with progressive shortness-of-breath. On examination he is found to have fine crackles in both lung bases and oxygen saturations of 93% on room air.
A diagnosis of idiopathic pulmonary fibrosis is suspected. Which one of the following chest x-ray findings develops first in patients with idiopathic pulmonary fibrosis?
A/ Asymmetrical upper zone 'ground-glass' changes
B/ Small, peripheral opacities in the lower zones
C/ Perihilar horizontal septal lines
D/ Honeycombing
E/ Loss of left heart border
On examination, he is comfortable at rest with oxygen saturations 95% on air. There is no evidence of lymphadenopathy, clubbing or cyanosis. He has fine crackles at both lung bases that do not alter on coughing.
Which of the following investigation findings would support a diagnosis of idiopathic pulmonary fibrosis?
A/ Reticular changes on CT imaging that is worse at the bases
B/ Obstructive picture on spirometry
C/ Extensive ground glass opacities on CT imaging
D/ Increased transfer factor on spirometry
E/ A lymphocytosis on bronchoalveolar lavage
A 68-year-old male patient presents with a 6-month history of shortness of breath that is worse on exertion with reduced exercise tolerance & no associated wheeze, or haemoptysis but does have a dry cough.
He has hypertension and takes amlodipine 5mg once a day. He has never smoked or worked with asbestos
DISEASES OF THE PLEURA, DIAPHRAGM AND CHEST WALL
OBJECTIVES
To know theepidemiology ,
etiology,
pathogenesis ,
clinical presentation
investigation ,
diagnosis ,
treatment
,complication ,
prognosis
Pleural effusion
Appearance of fluidand features
Type of fluid
Predominant cells in fluid
Other diagnostic features
Pleura fluid
Cause Appearance
Tuberculosis Serous, usually amber-coloured
Serous, often blood-stained Malignant disease
Cardiac failure
Pulmonary infarction
Rheumatoid disease
SLE
Acute pancreatitis
Obstruction of thoracic duct Milky
Clinical assessment
Symptoms (pain on inspiration and coughing)
signs of pleurisy (a pleural rub) often precede the development of an effusion.
The onset may be insidious.
Breathlessness severity depends on the size and rate of accumulation.
Investigations
Imaging
The erect PA chest film .
200 mL of fluid is required ,
ultrasound or CT smaller effusions.
Pleural fluid localised below the lower lobe ('subpulmonary effusion').
Fluid localised within an oblique fissure.
Ultrasonography is more accurate than plain chest radiography.
To distinguish pleural fluid from pleural thickening.
CT better than either plain radiography or ultrasound,.
Light's criteria for distinguishing pleural transudate from exudate
Pleural fluid is an exudate if one or more of the following criteria are met:
Pleural fluid protein:serum protein ratio > 0.5
Pleural fluid LDH:serum LDH ratio > 0.6
Pleural fluid LDH > two-thirds of the upper limit of normal serum LDH .
Pleural aspiration and biopsy
Empyema
This is a collection of pus in the pleural space.The pus may be thin or so thick.
Microscopically, neutrophil leucocytes are present in large numbers.
An empyema may involve the whole pleural space or only part of it ('loculated' or 'encysted' empyema) and is usually unilateral.
Aetiology
A secondary to infection in a neighbouring structure.
'Para-pneumonic' effusion become secondarily infected.
infection of a haemothorax .
Empyema remains a significant cause of morbidity and mortality.
Aspiration of fluid
Ultrasound or CT is used to identify the optimal site using a wide-bore needle.
features suggesting empyema
1-fluid is thick and turbid pus.
2-Biochemistery
fluid glucose low
LDH very high
fluid pH low
However, pH measurement should be avoided if pus is thick.
3- Baceriology pus is culture.
The pleural biopsy for histology and culture.
ManagementTreatment of non-tuberculous empyema
When the patient is acutely ill and the pus ia drained
a wide-bore intercostal tube .
The tube should be put on suction .
Antibiotic
directed against the organism causing the empyema should be given for 2-4 weeks.
Empirical antibiotic treatment (e.g. intravenous co-amoxiclav or cefuroxime with metronidazole).
surgical intervention :If the intercostal tube is not providing adequate drainage.
Treatment of tuberculous empyema
Antituberculosis chemotherapy
the pus in the pleural space aspirated through a wide-bore needle.
surgery is occasionally required.
Pneumothorax
The presence of air in the pleural space.Types
SpontaneousPrimary
SecondaryTraumatic
Primary• No evidence of overt lung disease.
Air escapes from the lung
into the pleural space through rupture of a small pleural bleb,
or the pulmonary end of a pleural adhesion
Secondary
• Underlying lung disease,COPD
Tuberculosis;
Asthma,
Lung abscess,
Pulmonary infarcts,
Bronchogenic carcinoma,
All forms of fibrotic
Traumatic
Iatrogenic (e.g. following thoracic surgery or biopsy) or chest wall injurySpontaneous pneumothorax
Clinical featuresThe primary spontaneous peaks in males aged 15-30 years.
Secondary spontaneous pneumothorax occurs mainly in males > 55 years.
The most common symptoms:
1- sudden-onset unilateral pleuritic chest pain.
2- breathlessness.
3-Sever breathlessness in those with underlying chest disease, and may not resolve spontaneously.
Examination
• may be normal in patients with a small pneumothorax.
• A decreased or absent breath sounds in larger pneumothorax .
3 - The combination of absent breath sounds and resonant percussion note.
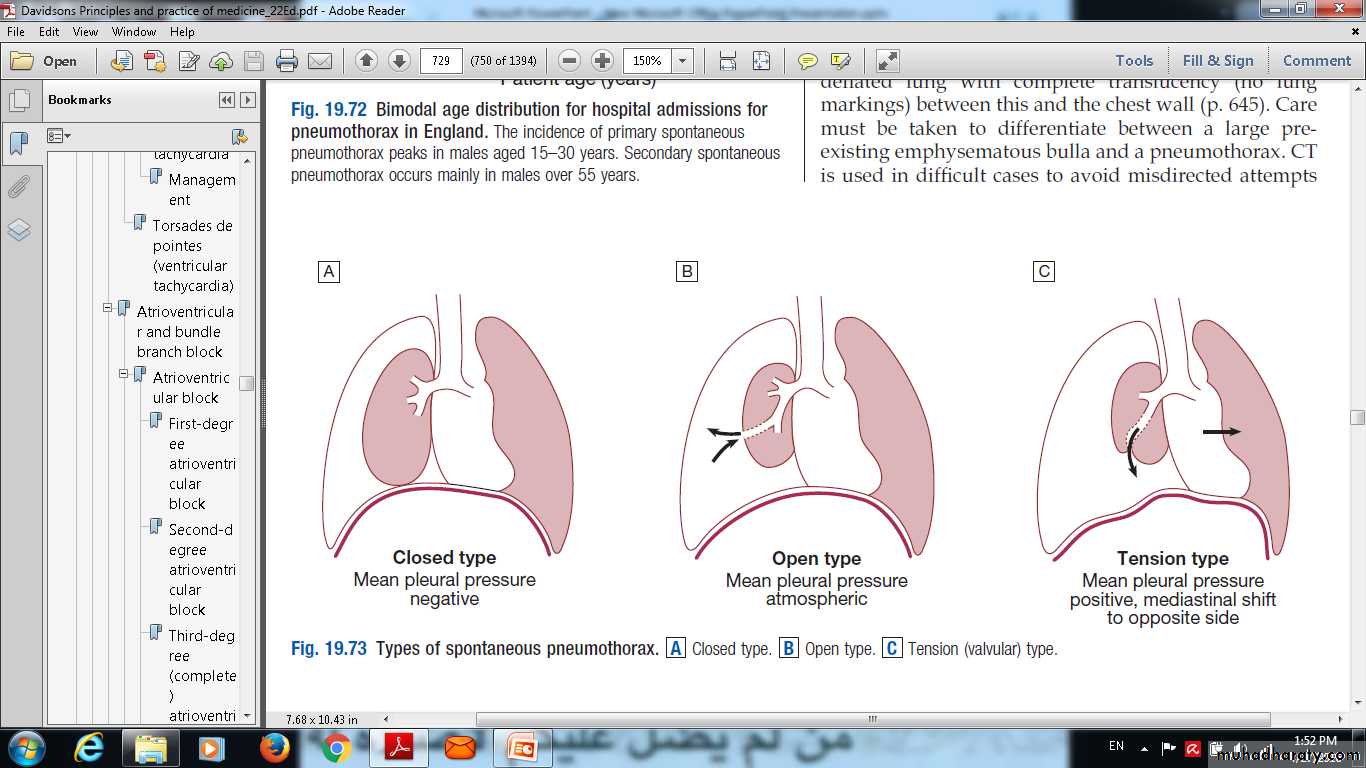
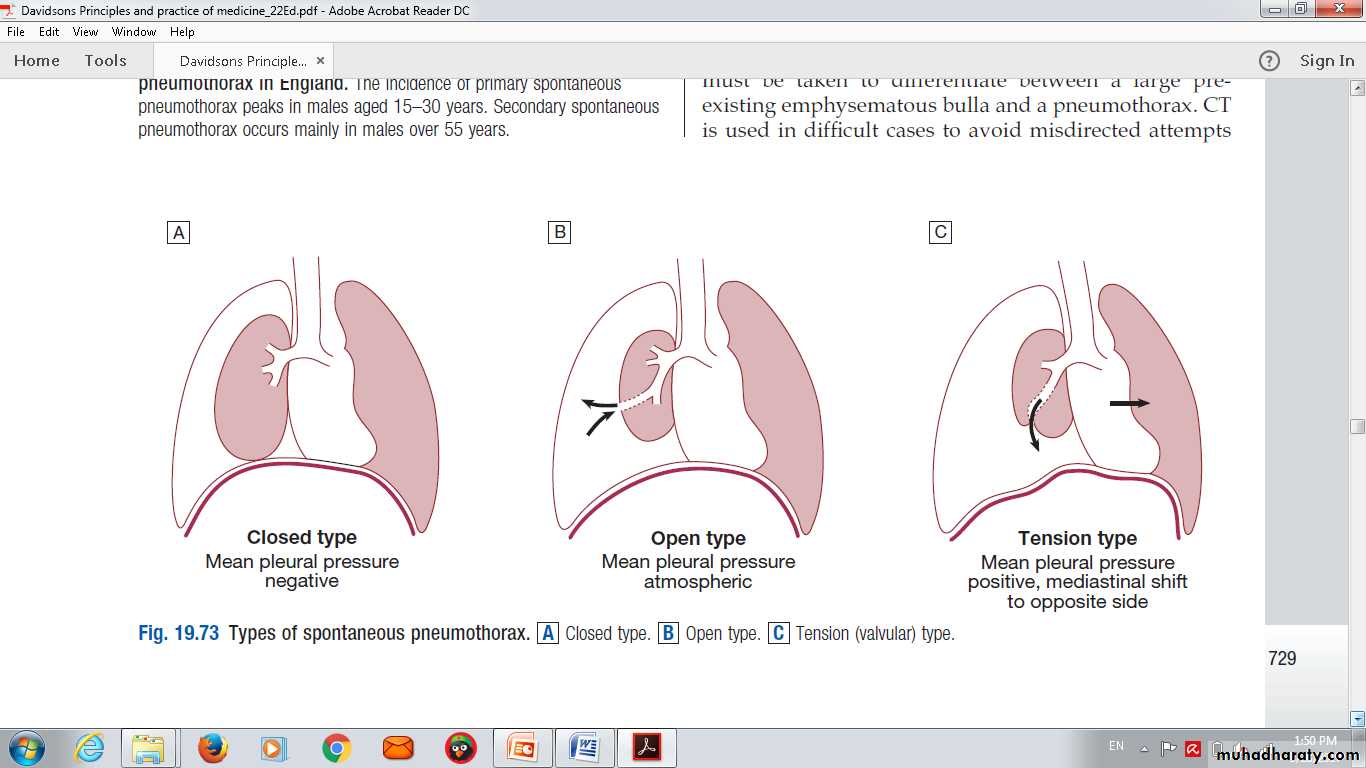
Types of spontaneous pneumothorax.
1-Closed type.
2-Open type. 3-Tension (valvular) type.
Types of spontaneous pneumothorax. A Closed type. B Open type. C Tension (valvular) type
Clinical features
The sudden-onset unilateralpleuritic chest pain .breathlessness.
severe breathlessness in those with underlying chest disease .
Small pneumothorax,
may be normal physical examination.
Larger pneumothorax
results in decreased or absent breath
sounds
Tension pneumothorax
rapidly progressive breathlessness.
tachycardia.
hypotension.
cyanosis and tracheal displacement.
treatment& Investigation
Chest Xray.CT chest.
Treatment
Small asymptomatic in healthy need observation .
Larger need aspiration.
Tension ,elderly,sever lyng diseases need intercostal chest tube.
Investigations
The chest X-ray.CT is useful in distinguishing bullae from pleural air.
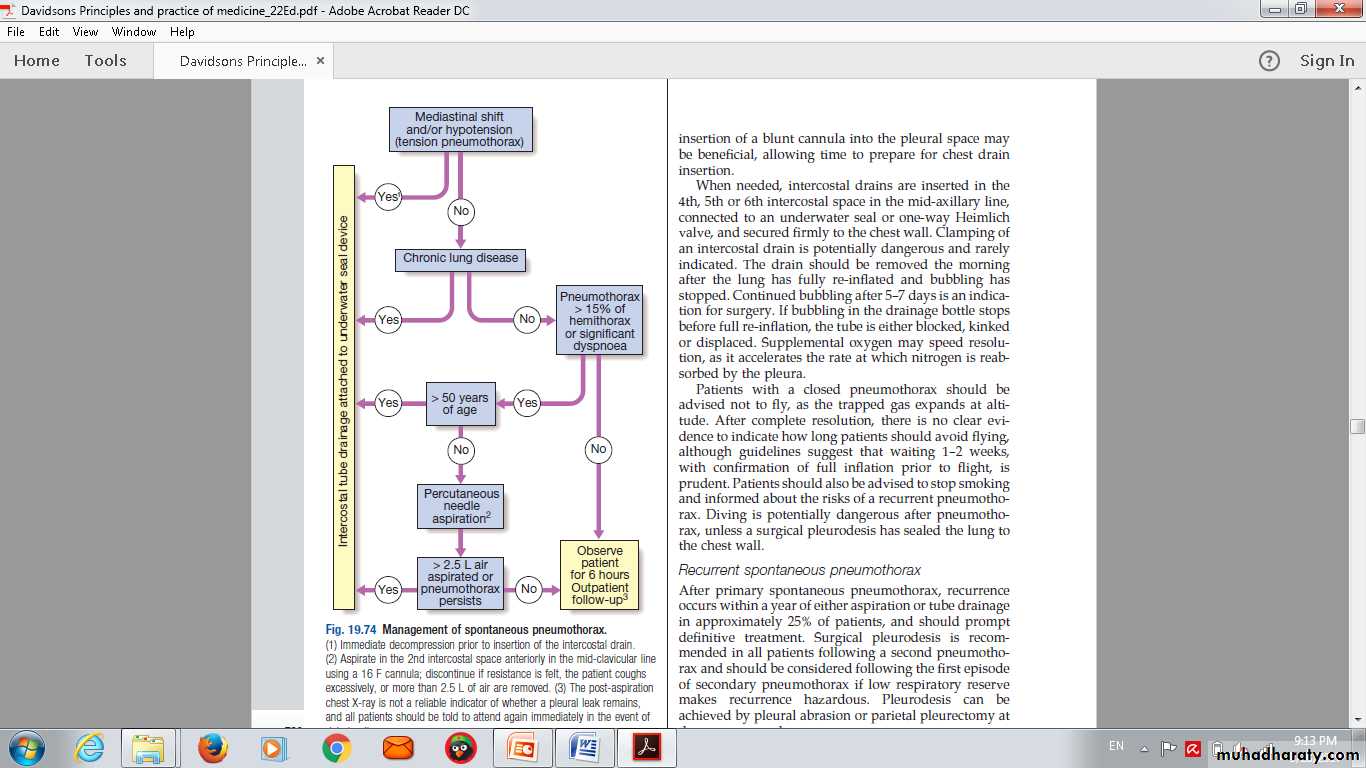
Management
Primary pneumothorax
the lung edge is less than 2 cm from the chest wall.
the patient is not breathless.
normally resolves without intervention.
A moderate or large spontaneous primary pneumothorax : In young patients
percutaneous needle aspiration of air
secondary pneumothorax may cause respiratory distress.
In patients with significant underlying chronic lung disease
the success rate of aspiration is much lower,
intercostal tube drainage
H0SPITAL ADMISSION particularly in those over 50 years old and those with respiratory compromise.
Management of spontaneous pneumothorax.
(1) Immediate decompression prior to insertion of the intercostal drain.(2) Aspirate in the 2nd intercostal space
discontinue if
• resistance is felt,
• the patient coughs excessively,
• more than 2.5 L of air are removed.
• advised
• Supplemental oxygen
avoid flying, .
to stop smoking
(3) The post-aspiration
chest X-ray is not a reliable indicator of whether a pleural leak remains,
and all patients should be told to attend again immediately in the event of deterioration.
DISEASES OF THE DIAPHRAGM ANDCHEST WALL
Disorders of the diaphragmCongenital disorders
Diaphragmatic hernias
Eventration of the diaphragm
Acquired disorders
Elevation of a hemidiaphragm cause by
• Phrenic nerve paralysis
• • Eventration of the diaphragm
• • Decrease in volume of onelung (e.g. lobectomy,unilateral pulmonaryfibrosis)
• • Severe pleuritic pain
• • Pulmonary infarction
• • Subphrenic abscess
• • Large volume of gas in the stomach or colon
• • Large tumours or cysts of the liver
Chest wall deformity
KyphosisKyphoscoliosis
Pectus excavatum funnel
Pectus carinatum pigeon
Malignant diseases of pleura
MesotheliomaAs pleural effusion
THANK U
Q
QUIZE