Disorders of Calcium metabolism
About 98% of body calcium is found in the body skeletonThe extraosseous fraction of Calcium effect :
Neuromuscluar excitibility .
hypocalcaemia lead to tetany .
- Cardiac muscle function .
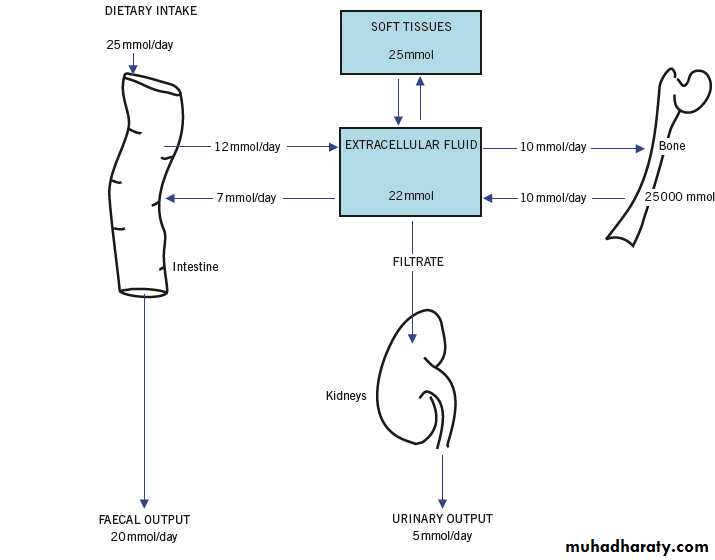
The total body calcium depends upon the calcium absorbed from dietary intake and that lost from the body.
.
( The approximate daily turnover of total body calcium.)
* Factors affecting calcium intake
About 25 mmol (1gm) of calcium is ingested per day ,
There is net absorptoin of ( 6-12 mmol) , the active metabolite of vitamin D (1,25 (OH)2 D3 ) is needed for calcium absorption .
Factors affecting calcium loss
Calcium is lost in urine and faeces .
- Urinary calcium excreation depend on GFR and renal tubular function ,
- PTH and (1,25 (OH)2 D3 ) increase urinary calcium reabsorption .
Faecal Calcium may form insoluble, poorly absorbed complex with oxalate , phosphate or fatty acid
so steatorrhoea may leads to calcium malabsorption .
CONCEPT OF PLASMA CALCIUM ANDALBUMIN CORRECTION (ADJUSTED)
The plasma Calcium conc. in healthy subjects around (2.15-2.55) mmol/L and present in two forms :-Calcium bound to proteins,: mainly albumin this accounts for a little less than half the total calcium concentration as measured by
routine analytical methods and is the physiologically inactive form.
-Free ionized calcium (Ca2+), : which comprises most of the rest.
This is the physiologically active fraction.Changes in plasma protein concentration, particularly of albumin, alter the most commonly measured concentration, that of plasma total calcium, but not that of the free ionized fraction.
.
- Changes in plasma hydrogen ion concentration ([H+]) affect the binding of calcium to plasma proteins because H+ competes with Ca2+ for binding sites.
- The plasma total calcium concentration is unaltered by changes in [H+] ion .
If [H+] falls, as in an alkalosis, tetany may occur, despite a normal plasma total calcium concentration.
- Conversely, an acidosis decreases binding and so increases the proportion of plasma calcium in the free ionized form , also, by
increasing calcium solubility, it increases the rate of release of calcium from bones into the extracellular fluid (ECF).
- The increased load reaching the kidney increases the renal calcium loss.
Prolonged acidosis may cause osteomalacia
Control of plasma calcium
an adequate supply of:Calcium
Vitamin D
Normal functioning of the:
IntestineParathyroid glands
Kidneys
Parathyroid hormone
(PTH) is a single-chain polypeptide , the biological actions include:
- Stimulation of osteoclastic bone resorption , so releasing both free ionized calcium and phosphate into (ECF) →increases the plasma conc. of both calcium and phosphate .
.
- PTH decreased renal tubular reabsorption of phsphate , causing phosphaturia and increased reabsorption of calcium → increase plasma calcium and decrease plasma phosphate .
So ↓ free ionized Calcium → ↑PTH secretion → stimulate 1-α-hydroxylase activity → stimulate 1,25(OH)2D3 synthesis ,
until calcium return to normal .
Hypomagnesaemia → ↓ PTH secretion
Metabolism and action on vitamin D
Vitamin D is derived from :
Ergocalciferol ( D2) from diet .
Cholecalciferol ( D3) formed in the skin by action of U/V light on 7-dehydrocholesterol . It is inactive untill metabolized in the liver by 25-hydroxylase enzyme to (24,25 DHCC) , then in the kidney in proximal renal tubules a second hydroxylation by the enzyme 1-α-hydroxylase to form active metabolite 1,25 –(OH)2D3 this stimulated by :
Low plasma phosphate.
Increase plasma PTH
And vice versa
Disorder of calcium metabolism
Hypercalcaemia :Clinical effects of hypercalcaemia :
A)- Renal effects :
-Renal damage :
one of the most serious clinical consequences of prolong hypercalcaemia → precipitate in the kidney .
- Polyuria :
Hypercalcaemia may cause reversible inhibition of tubular response to ADH .-Renal Calculi .
-Hypokalaemia : Calcium may directly inhibit potassium reabsorption from renal lumen .
.
B) Calcium stimulate gastrin secreation :
-Chronic hypercalcaemia → peptic ulceration .
C) CNS effects : anorexia , nausea, vomiting .
Depress neuromuscular excitability in both voluntary and involuntary muscle → muscular hypotonia .D) Bone and goint pain .
E) E C G changes .
Investigation of hypercalcaemia
Two groups of causes should be diffrentiated for raise plasma calcium1)- Hypercalcaemia due to ( high PTH and hypophosphataemia) .
2)- Hypercalaemia due to other causes associated with ( low PTH and hyperphosphataemia ) .
The following procedures may be useful to find the cause of hypercalcaemia :
- Establish the plasma albumin concentration .
- Check the specimen without venous stasis (without tourniquet) to eliminate art factual haemoconcentration .
Drug history such as (vitamin D) is important .
If plasma phosphate is low suggests the diagnosis of primary hyperparathyroidism .
`
- It is essential that primary hyperparathyroidism and malignant hyper- calaemia are distinguished .
A raised plasma PTH is usually seen in primary hyperthyroidism
while suppressed level are found in malignant states , ( CBP , ESR and radiological tests may be helpful ).
* Check growth hormone , T3 , T4 if endocrine causes .
* Serum protein electrophoresis : if multiple Myeloma is suspected .
* Urinary calcium determination (CaE) is useful to exclude hypocaliuric hypercalcaemia .
* Plasma ALP activity : if it is very high , it suggest either malignancy or bone disease such as Paget disease of the bone, while it is unlikely to be high due to uncomplicated primary hyperparathyroidism .
Hypocalcaemia
Clinical effects of a reduced plasma concentration ( Hypocalcaemia ) including even those with a normal total calcium conc. of alkalosis are :-Neuromuscular effect :
Increase neuromuscular activity → Tetany .
Paraesthesiae , hypotension , laryngospasm.
- Cardiovascular :
Cardiac arrhythmias and ECG changes (prolong Q-T interval) .-Psychiatric symptoms :
Depression
- Other :
Prolong hypocalcemia , even when mild interfers with the metabolism of the lens in the eye and may cause cataract .
Investigation of hypocalcaemia
As in case of hypercalcaemia two groups of causes should be diffrentiated for hypocalcaemia1)- Hypocalcaemia due to ( primary PTH deficiency and associated with hyperphosphataemia) .
2)- Hypocalcaemia due to other causes and associated with ( high PTH and usually hypophosphataemia ) .
- Determine first if the fall in total calcium concentration is due to a (low protein- bound fraction)
Drug history or chemical that may cause hypocalcaemia .
If the plasma phosphate is high ? If the plasma urea and creatinine conc. is high this suggest renal impairment
- Check plasma (25,OH)vitamin D levels , if the level are low , look for the causes of under nutrition and malabsorption states .
.
- Is the plasma phosphate conc. low ? If so calcium deficiency with normal secretion of PTH as a feedback response is likely , At this point a plasma PTH may useful.
- Is the plasma ALP activity is high → this may suggest prolong secondary hyperparathyroidism due to calcium deficiency .
- If indicated bone radiographs → signs of rickets or osteomalacia
- Raised plasma phosphate in face of hypocalcaemia and low PTH conc. suggest hypoparathyroidism .
Check the magnesium level since sever hypomagnesamia can cause hypocalcaemia by reducing the action of PTH .
A raised urinary calcium conc. may help diagnosis of the rare autosomal dominant hypercalciuric hypocalcaemia .