Physical factors & the skin
Dr. Hadaf AljunaiyehProfessor of dermatology
College of medicine/ thi qar university
objectives
By the end of this lecture, the student should be able to:Classify the main physical factors in the environment
Describe the skin changes induced by these factors
Recognize the main preventive measures for these conditions
& their best treatment modalities.
Physical factors in the environment
HeatCold
Sun
Physical pressure
Radiation
heat
The main dermatoses induced by heat are:1- Burn
2- Miliaria
3- Erythema ab igne
burn
ThermalElectrical
burn
Classified into 3 degrees:First, second & third
1st degree:
only erythema + sometimes desquamation + if a large is involved, then constitutional symptoms2nd degree:
A- superficial type B- deep typesuperficial deep
causing vesicles & bullae causing pallor
heal without scarring delayed healing with scarring
3rd degree: full thickness loss of tissue with scarring
miliaria
Occlusion of eccrine sweat gland leads to sweat retention & failure ofdelivery of sweat to skin surface.
Eventually backed-up pressure causes rupture of sweat gland or duct
at different levels & the escape of sweat into adjacent tissue producing miliaria.
Common in hot, humid climates.
Different forms of miliaria occur depending on the level of injury to the sweat gland.
1- Miliaria crystallina
1-Small, clear, superficial vesicles without inflammation.2-In bedridden patients and bundled children.
3-Lesions are asymptomatic & rupture
at the slightest trauma.
4-Self-limited; requires no Rx
5- sweat duct is blocked at the
stratum corneum level
2-Miliarai rubra ( prickly heat)
Discrete, extremely pruritic,erythematous papulovesicles with
sensation of prickling, burning,
or tingling.
Site of injury is prickle cell layer
Commonest type mostly in
Summer & jobs with excessive heat
3-Miliaria profunda
Occlusion is in the papillary dermisOnly seen in tropics
Rare in our country
Deep seated flesh colored papules
Asymptomatic
treatment
Mild cases respond to cooling of skinPlace patient in a cool environment
Use dusting powder as talcum
Cooling baths of menthol & corn starch
Emollients & steroid ointment to dissolve keratin
Plugs & restore sweating
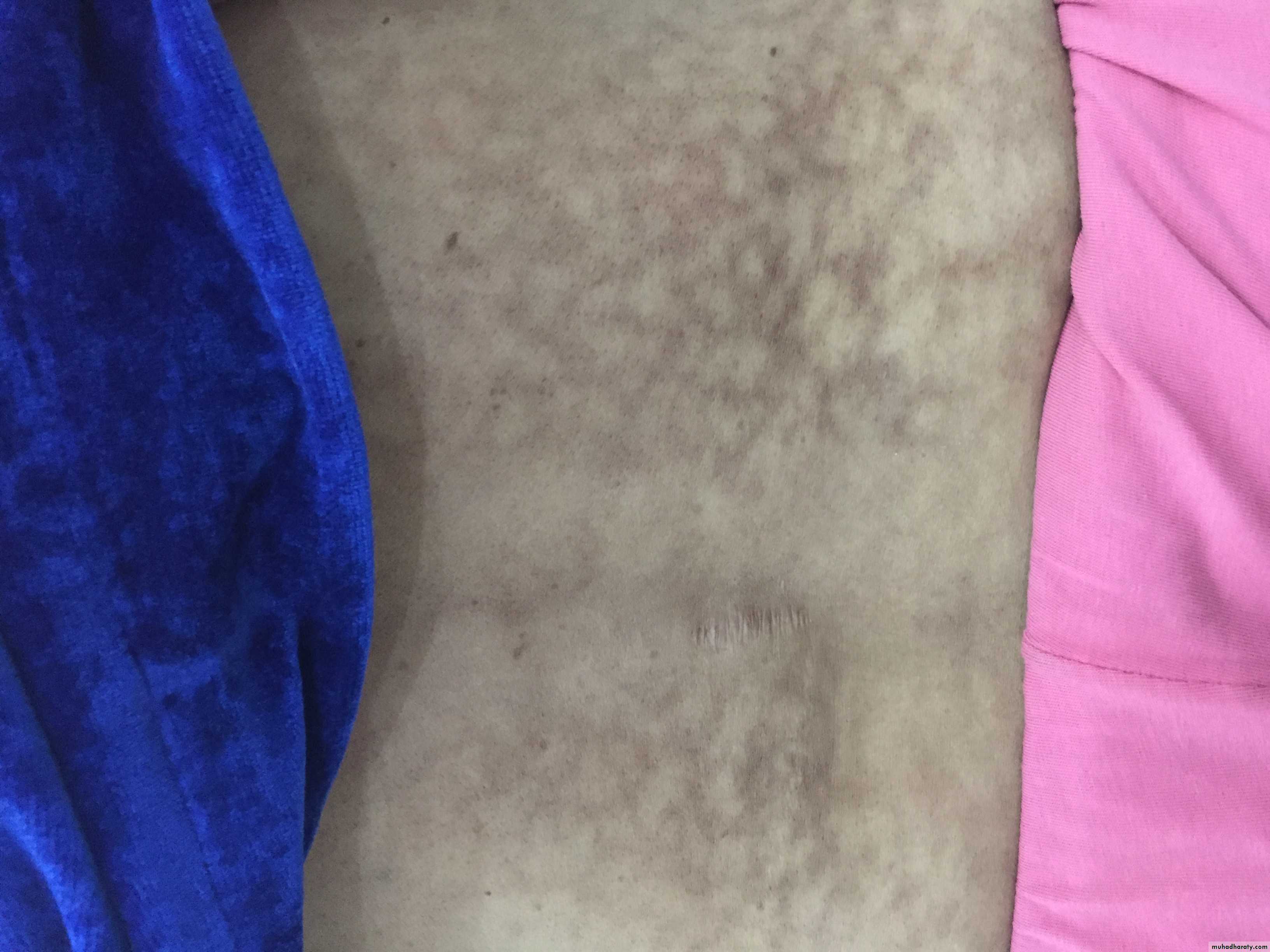
Erythema ab igne
1- Persistent erythema or the coarsely reticulatedresidual pigmentation resulting from it, due to long
exposure to excessive heat without burn.
2- First transient, then permanent
3- Mostly on the legs of women
May cause epithelial atypia, rarely Bowen’s disease or squamous cell carcinoma.
Cold injury
perniosis(=chill blains)
Cold hypersensitivity
Erythema & swelling (purple pink) of
exposed parts mainly fingers, toes, nose & ears
Can lead to blistering or ulceration
Pain, itching & burning
Cool to touch, onset enhanced by dampness
IMG_9356.JPG
IMG_9356.JPGtreatment
Protection & prophylaxis of cold Quit smoking
Topical steroids & systemic antihistamines
Nifidipine 20 mg t.d.s., vasodilators (nicotinamide, dipyridamole)
Spontaneous resolution occur in 1-3 weeks
Frost bite.
Cold toxicity due to exposure to extremelylow temperatures with freezing of tissue
Affected part is pale, waxy, painless
Different degrees of tissue damage from erythema to
deep gangrene similar to burn
Degree of damage depends on temperature & duration
treatment
Rapid rewarming in hot water bath
Analgesia: counteract thawing pain
Supportive measures:
Bed rest
High protein/calorie diet
Wound care
Avoidance of trauma
Solar injury
The sunlight spectrum is divided intoVisible light 400 to 760 nm, has little biologic activity,
except for stimulating the retina
Infrared radiation beyond 760 nm, experienced as radiant heat.
Below 400 nm is the ultraviolet spectrum, divided into three bands:
-UVA, 320 to 400 nm
-UVB, 290 to 320 nm
-UVC, 200 to 290 nm
Virtually no UVC reaches the earth’s surface, because it is absorbed by the ozone layer.
Sun burn
Normal reaction of skin to sunlight inexcess of erythema dose
Erythema, edema, sometimes blistering on sun exposed skin
Desquamation follows within a week
If severe may be accompanied by fever, chills, nausea
& hypotension
Treatment by analgesics, cool compresses, topical steroids
Erythema, edema, blistering
desquamation
Treatmentcool compresses
photosensitivity
Abnormal reaction to normal amount of sunlightCan be either:
1- chemical photosensitivity: phototoxic & photo allergic photosensitizers
2- metabolic disorders
3- light exacerbated disorders
4- idiopathic phtosensitivity
Chemical photosensitivity
Photosensitizers are substances that may induce an abnormal reaction in skin exposed to sunlight or its equivalent.
Substances may be delivered externally or internally.
Increased sunburn response without prior allergic sensitization is called phototoxicity. Phototoxicity may occur from both externally applied phytophotodermatitis or internally administered chemicals phototoxic drug reaction.
Photo allergy: needs prior exposure to the substance (sensitization)
phytophotodermatitis
Contact between certain plants containing a substance called furocumarine with moist skin & then exposed to long wave UV (UVA)A dermatitis develops followed by intense pigmentation that can last wk.s or m.s
More in women & children dealing with citrus fruits, & on exposed skin (face & hands)
phyto-photo dermatitis
2- metabolic photosensitivitypellagra & porphyria
PellagraNiacin deficiency
4 D’s disease
Metabolic photosensitivity
porphyriaDefect in heam
synthesis3- light exacerbated disorders(Diseases aggravated by sun light exposure)
1-genetic: xeroderma pigmentosum2- acquired: SLE, Darier’s, vitiligo, acne, small % of psoriasis, dermatomyositis, lichen planus actinicus, & chloasma.
4- idiopathic photosensitivityple (polymorphic light eruption)
Different morphologies in different peopleConstant morphology in the same patient
More in young adults, more in females
Mostly erythematous papular rash on exposed skin
Starts in spring & improves in summer
treatment
Prophylaxis:
-Avoid sun exposure between 10 am and 2 pm.
-Barrier protection with hats and clothing.
-Sunscreen agents include UV-absorbing chemicals (chemical sunscreens:, and UV-scattering or blocking agents (physical sunscreens).
1- Avoidance: sunscreens with SPF more than 30 with physical & chemical properties
2- Topical steroids: usually potent3- Systemic antihistamines: to control itching
4-Systemic steroids: in severe cases
5- Antimalarial: as chloroquine
6- Light therapy as PUVA or UVB to induce hardening of the skin7- Immunosuppressant only in recalcitrant cases: azathioprine & cyclosporin
Mechanical trauma
CALLUS: circumscribed hyperkeratosis induced by pressure, diffuse with no central core.CLAVUS: (corn): circumscribed conical thickening with base on surface & apex down pressing on subjacent structures, of 2 types: Soft corns & hard corn