Fifth Stage
Dermatology
Dr. Hadaf – Lecture 6
1
Objectives
•
By the end of this lecture, the student should be able to:
•
Classify the main physical factors in the environment
•
Describe the skin changes induced by these factors
•
Recognize the main preventive measures for these conditions & their best
treatment modalities.
Physical factors in the environment
•
Heat
•
Cold
•
Sun
•
Physical pressure
•
Radiation
Heat
•
Burn
•
Miliaria
•
Erythema ab igne
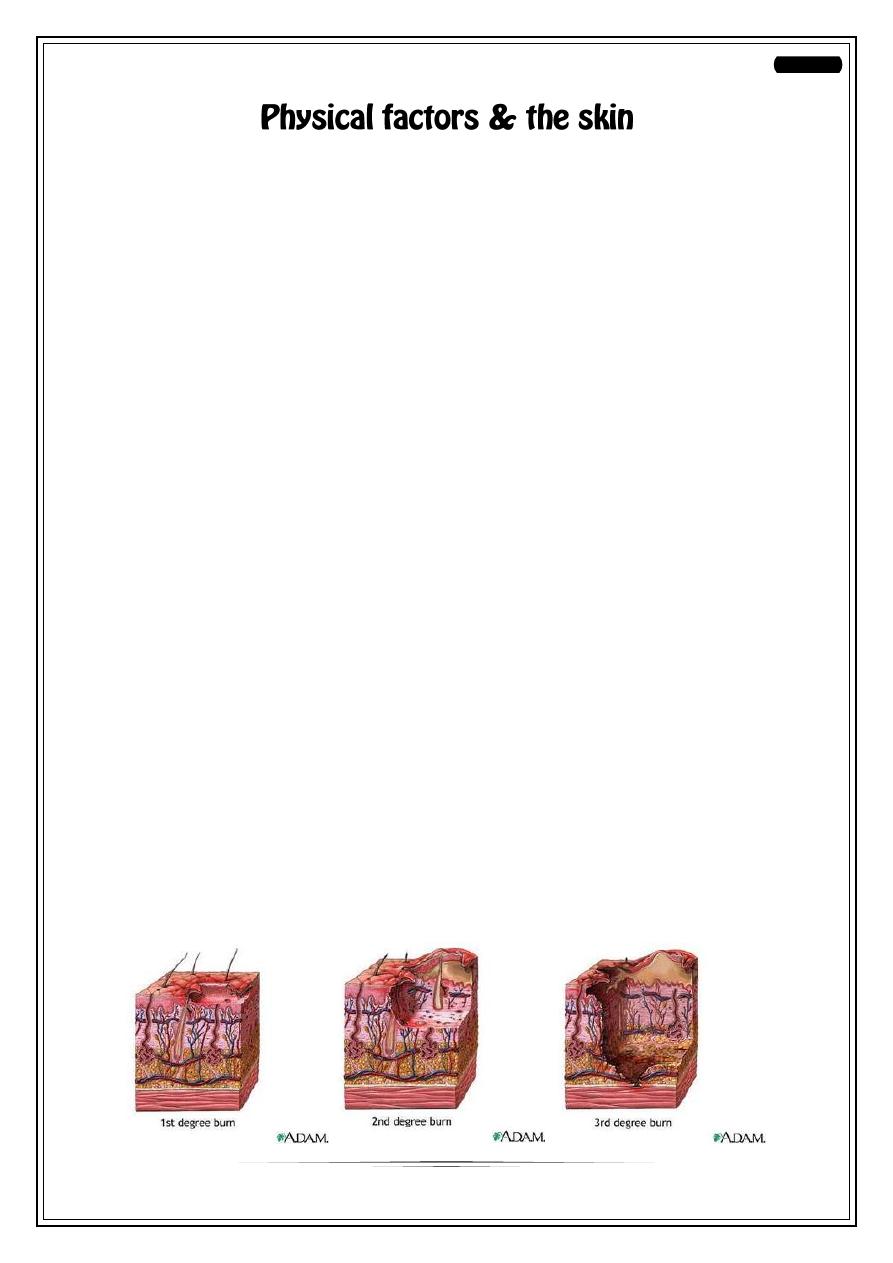
Burn
o
Thermal
o
Electrical
•
1
st
degree: only erythema + sometimes desquamation+constitutional symptoms if
a large area is involved
•
2
nd
degree:
A- superficial B- deep
superficial deep
causing vesicles & bullae causing pallor
heal without scarring delayed healing with scarring
•
3
rd
degree: full thickness loss of tissue with scarring
2
Miliaria
•
Occlusion of eccrine sweat gland leads to retention of sweat with failure of
delivery of sweat to the skin surface.
•
Eventually backed-up pressure causes rupture of sweat gland or duct at different
levels.
•
Escape of sweat into adjacent tissue produces miliaria.
•
Common in hot, humid climates.
•
Different forms of miliaria occur depending on the level of injury to the sweat
gland.
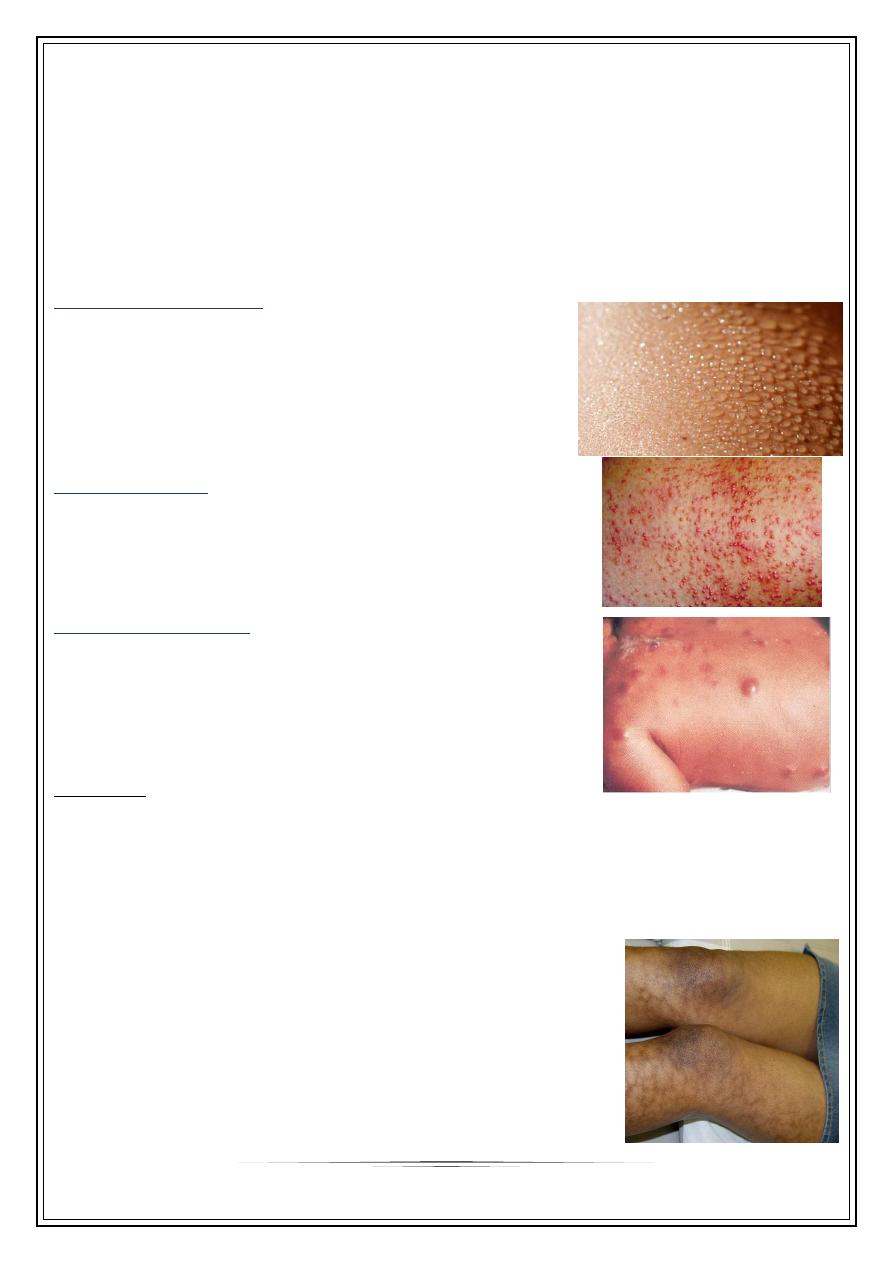
1- Miliaria crystallina
•
-Small, clear, superficial vesicles without
inflammation.
•
-Appears in bedridden pts and bundled children.
•
-Lesions are asymptomatic and rupture at the
slightest trauma.
•
-Self-limited; no treatment is required.
2-Miliarai rubra
•
Discrete, extremely pruritic, erythematous
papulovesicles with sensation of prickling, burning, or
tingling.
•
-Site of injury is prickle cell layer.
3-Miliaria profundal
•
Occlusion is in the papillary dermis
•
Only seen in tropics
•
Rare in our country
•
Deep seated flesh colored papules
•
asymptomatic
Treatment
•
Mild cases respond to cooling of skin
•
Place patient in a cool environment
•
Use dusting powder as talcum
•
Cooling baths of menthol & corn starch
•
Emollients & steroid ointment to dissolve keratin plugs & restore sweating
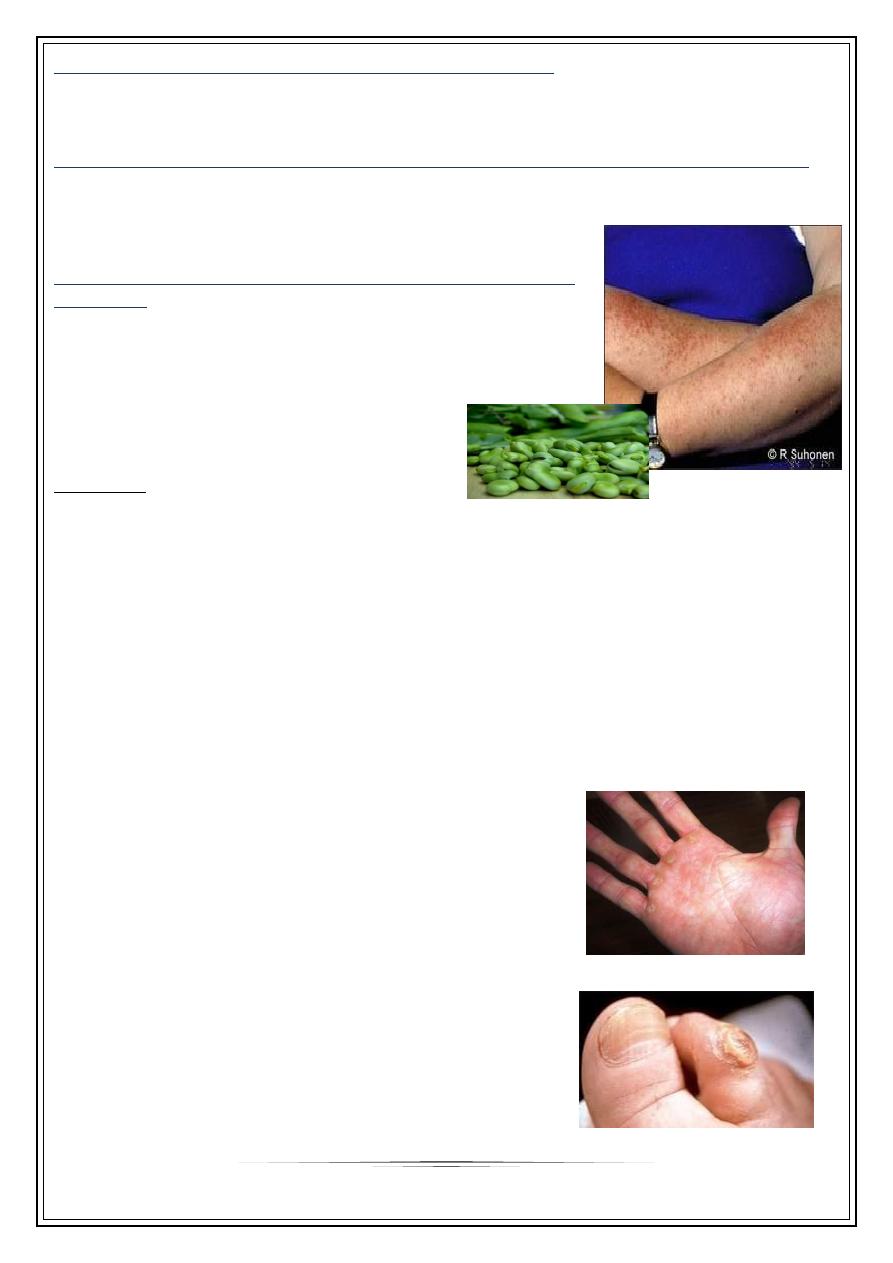
Erythema ab igne
•
Persistent erythema or the coarsely reticulated residual
pigmentation resulting from it, due to long exposure to
excessive heat without burn.
•
First transient, then permanent
•
Legs of women
•
May cause epithelial atypia, rarely Bowen’s disease or
squamous cell carcinoma.
3
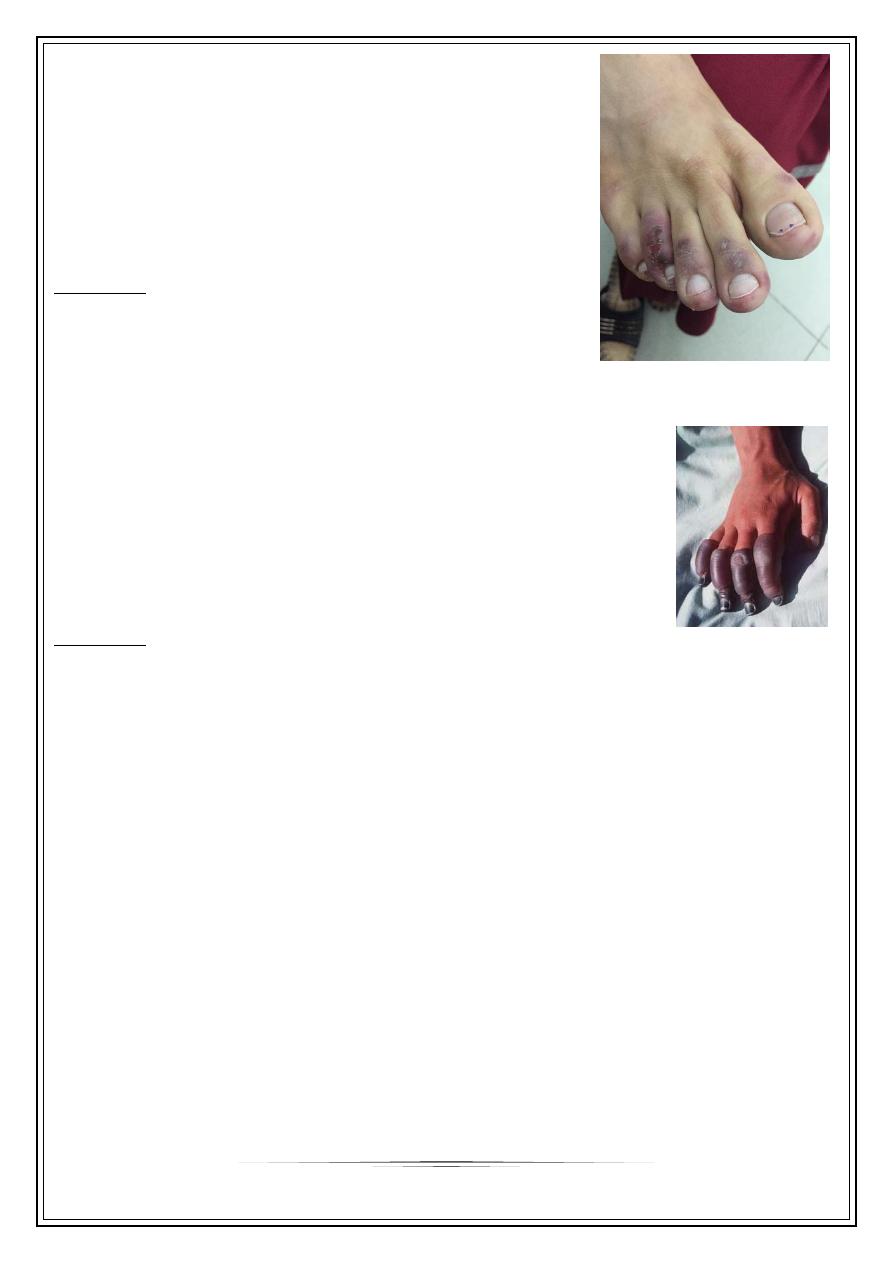
Cold injuries
Perniosis(=chill blains)
•
Cold hypersensitivity
•
Erythema & swelling (purple pink) of exposed parts
•
Mainly fingers, toes, nose & ears
•
Can lead to blistering or ulceration
•
Pain, itching & burning
•
Cool to touch, onset enhanced by dampness
Treatment
•
Protection & prophylaxis of cold
•
Quit smoking
•
Topical steroids & systemic antihistamines
•
Nifidipine 20 mg t.d.s., vasodilators (nicotinamide, dipyridamole)
•
Spontaneous resolution occur in 1-3 weeks
Frost bite
•
Cold toxicity due to exposure to extremely low temperatures
•
Freezing of tissue
•
Affected part is pale, waxy, painless
•
Different degrees of tissue damage from erythema to deep
gangrene similar to burn
•
Degree of damage depends on temperature & duration
Treatment
•
Rapid rewarming in hot water bath
•
Analgesia: counteract thawing pain
•
Supportive measures:
• Bed rest
• High protein/calorie diet
• Wound care
• Avoidance of trauma
Solar injury
The sunlight spectrum is divided into
•
Visible light 400 to 760 nm, has little biologic activity, except for stimulating the
retina
•
Infrared radiation beyond 760 nm, experienced as radiant heat.
Below 400 nm is the ultraviolet spectrum, divided into three bands:
-UVA, 320 to 400 nm
-UVB, 290 to 320 nm
-UVC, 200 to 290 nm
Virtually no UVC reaches the earth’s surface, because it is absorbed by the ozone layer.
4
Sun burn
•
Normal reaction of skin to sunlight in excess of erythema dose
•
Erythema, edema, sometimes blistering on sun exposed skin
•
Desquamation follows within a week
•
If severe may be accompanied by fever, chills, nausea & hypotension
•
Treatment by analgesics, cool compresses, topical steroids
Treatment
•
Cool compresses
•
Analgesics+ soothing agents
Photosensitivity
Abnormal reaction to normal amount of sunlight
Can be either:
1- chemical photosensitivity: phototoxic & photo allergic photosensitizers
2- metabolic disorders
3- light exacerbated disorders
4- idiopathic phtosensitivity
1- Chemical photosensitivity
•
Photosensitizers are substances that may induce an abnormal reaction in skin
exposed to sunlight or its equivalent.
•
Substances may be delivered externally or internally.
•
Increased sunburn response without prior allergic sensitization is called
phototoxicity. Phototoxicity may occur from both externally applied
phytophotodermatitis or internally administered chemicals phototoxic drug
reaction.
•
Photo allergy: needs prior exposure to the substance (sensitization)
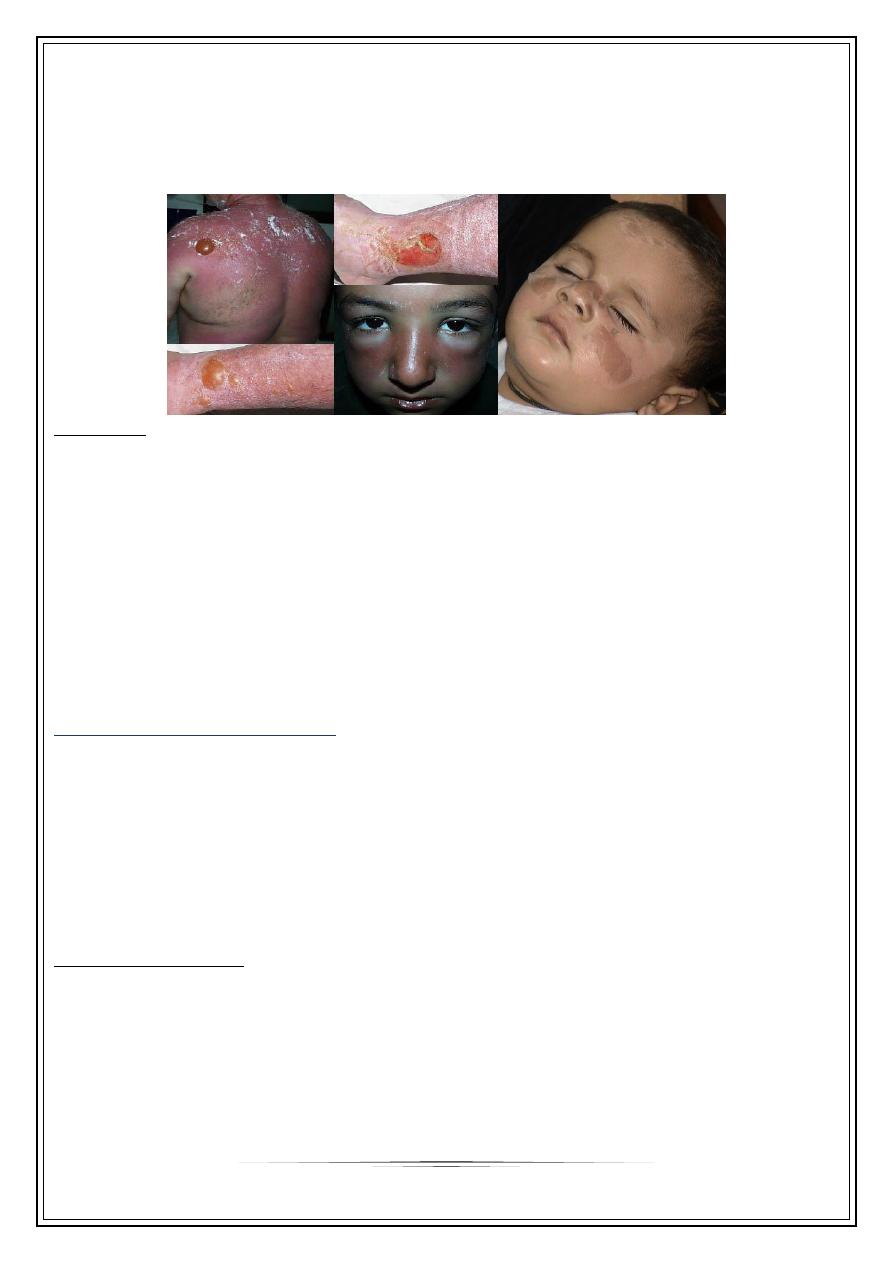
Phytophotodermatitis
•
Contact between certain plants containing a substance called furocumarine with
moist skin & then exposed to long wave UV (UVA)
•
A dermatitis develops followed by intense pigmentation that can last wk.s or m.s
•
More in women & children dealing with citrus fruits, & on exposed skin (face &
hands)
5
2- Metabolic photosensitivity pellagra & porphyria
Pellagra: Niacin deficiency: 4 D’s disease
Porphyria: Defect in heam synthesis
3- Light exacerbated disorders (Diseases aggravated by sun light exposure)
•
1-genetic: xeroderma pigmentosum
•
2- acquired: SLE, Darier’s, vitiligo, acne, small % of psoriasis, dermatomyositis,
lichen planus actinicus, & chloasma.
4- idiopathic photosensitivity PLE (polymorphic light
eruption)
•
Different morphologies in different people
•
Constant morphology in the same patient
•
More in young adults, more in females
•
Mostly erythematous papular rash on exposed skin
•
Starts in spring & improves in summer
Treatment
•
Prophylaxis:
•
-Avoid sun exposure between 10 am and 2 pm.
•
-Barrier protection with hats and clothing.
•
-Sunscreen agents include UV-absorbing chemicals (chemical sunscreens:,
and UV-scattering or blocking agents (physical sunscreens).
1- Avoidance: sunscreens with SPF more than 30 with physical & chemical properties
2- Topical steroids: usually potent
3- Systemic antihistamines: to control itching
4-Systemic steroids: in severe cases
5- Antimalarial: as chloroquine
6- Light therapy as PUVA or UVB to induce hardening of the skin
7- Immunosuppressant only in recalcitrant cases: azathioprine & cyclosporin
Mechanical trauma
CALLUS
: circumscribed hyperkeratosis induced by
pressure, diffuse with no central core.
CLAVUS (corn):
circumscribed conical thickenning
with base on surface & apex down pressing on subjacent
structures, of 2 types: Soft corns & hard corn
6
Thank you,,,
