Fifth Stage
Orthopedics
Dr. Haider – Lecture 2
1
Principles of Fracture Treatment
–
Part 1
Treatment of fractures
•
ATLS ( Advanced trauma life support )
•
Splint the fracture
•
Associated injuries
- Vascular injuries
- Nerve injuries
•
Decide for definitive treatment
AO PRINCIPLES
1. Anatomic reduction
Fracture reduction and fixation to restore functional anatomical relationships.
2. Stable fixation
Stability by rigid fixation or splintage, as the personality of the fracture and the injury
requires
3. Preservation of blood supply
Preservation of the blood supply to soft tissue and bone by careful handling and
gentle reduction techniques.
4. Early mobilization
Early and safe mobilization of the part and patient.
OUTLINE:
•
Closed Fracture
•
Reduce
•
Closed Reduction
•
Traction
•
Open Reduction
•
Hold
•
Sustained Traction
•
Cast Splintage
•
Functional Bracing
•
Internal Fixation
•
External Fixation
•
Exercise
2
Reduce
•
Aim for adequate apposition and normal alignment of the bone fragments
•
The greater contact surface area between fragments, the more likely is healing to
occur.
Reduction:
•
Operative
•
Closed reduction
•
Mechanical Traction
•
Non-operative
•
Open reduction
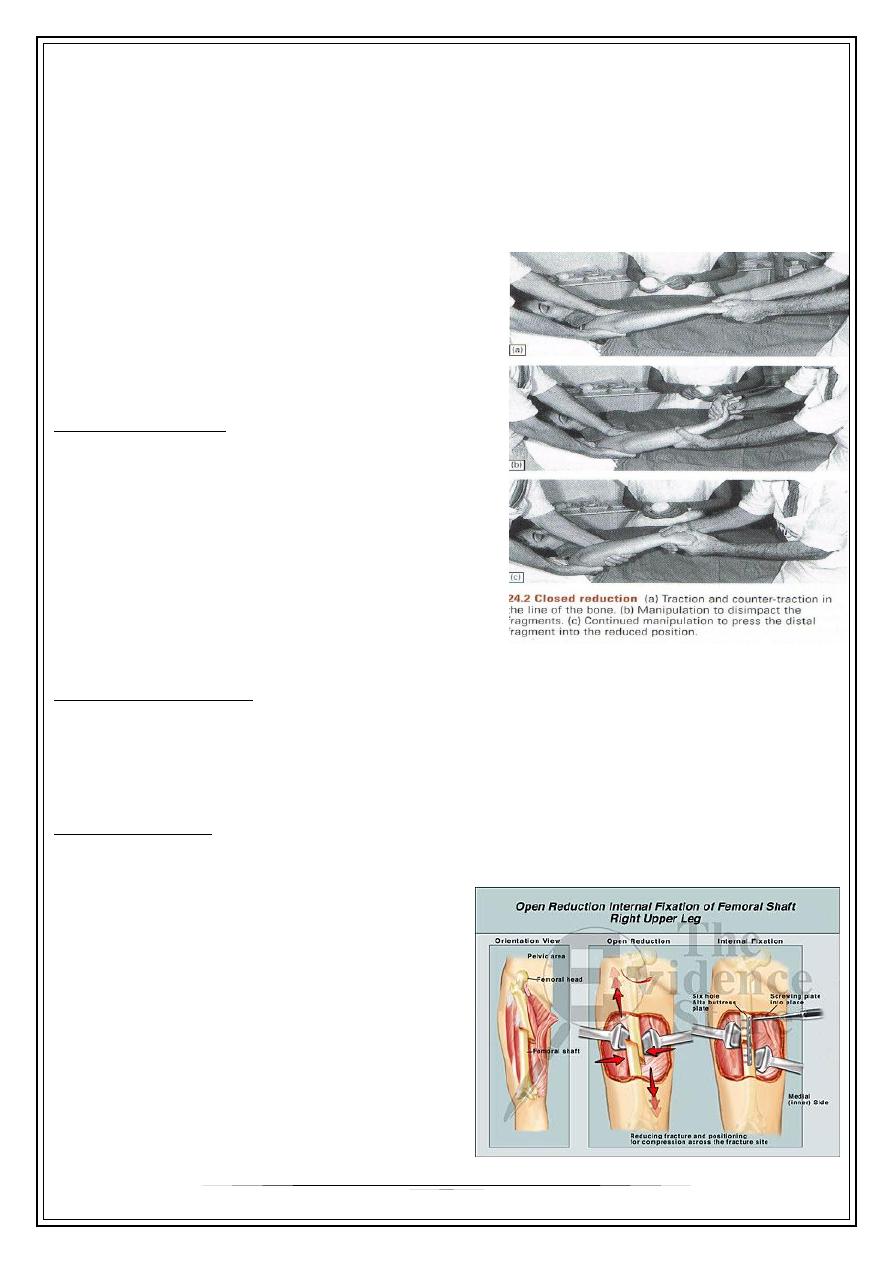
Closed Reduction
•
Suitable for
–
Minimally displaced fractures
–
Most fractures in children
–
Fractures that are likely to be stable
after reduction
–
Most effective when the periosteum
and muscles on one side of fracture remain intact
Mechanical Traction
•
Some fractures (example fracture of femoral shaft) are difficult to reduce by
manipulation because of powerful muscle pull
•
However, they can be reduced by sustained mechanical traction.
Open Reduction
•
Operative reduction under direct vision
•
Indications:
–
When closed reduction fails
–
When there is a large articular
fragment that needs accurate
positioning
–
When an operation is needed for
associated injuries
–
When a fracture needs an
internal fixation
3
Hold
•
Non Operative
•
Sustained traction
•
Cast Splintage
•
Functional Bracing
•
Operative
•
Internal Fixation
•
External Fixation
WHY TO HOLD?
•
To prevent displacement
•
To alleviate pain by some restriction of movement
•
To promote soft-tissue healing
•
To allow free movement of the unaffected parts
Sustained Traction
•
Traction is applied to limb distal to the fracture
•
To exert continuous pull along the long axis of the bone
•
Disadvantage and complications
–
Patient kept on bed for long time
–
Pressure ulcer
–
General weakness
–
Pulmonary infection
–
Contracture
–
Pin tract infection
–
Thromboembolic event
•
Methods
–
Traction by gravity
–
Balanced traction
–
Fixed traction
4
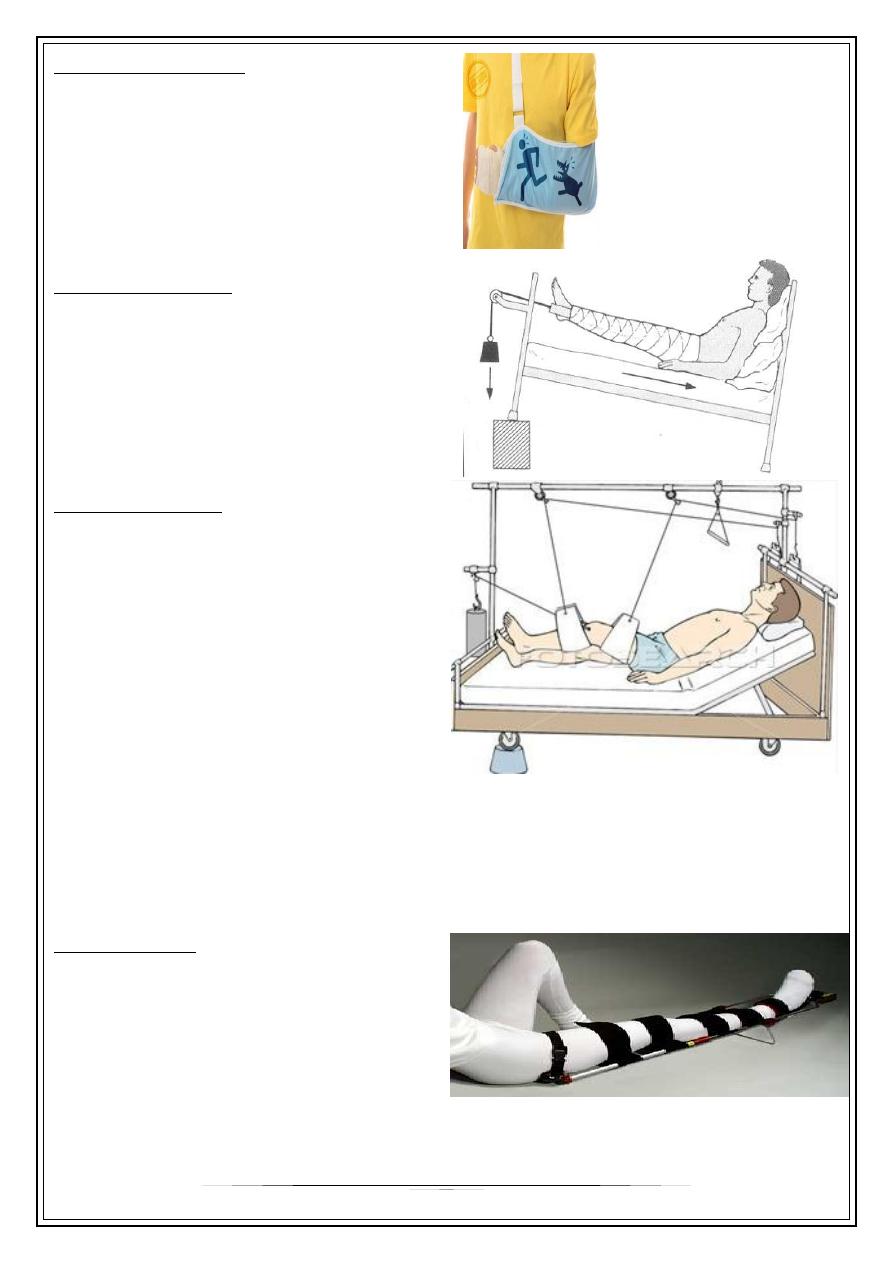
Traction By Gravity
Example:
Fracture of humerus
-
Weight of arm to supply traction
-
Forearm is supported in a wrist sling
Balanced Traction
•
Traction is applied to the limb by
way of adhesive strapping, kept in
place by bandages skin
traction
•
Sustain a pull no more than 4-5 kg
Skeletal Traction
•
Traction applied via stiff wire or pin
inserted through the bone distal to
the fracture skeletal traction
•
Can apply several times as
much force
↓↓↓
•
Complications:
•
Pin tract infection
•
Damage to epiphyseal growth plate
•
fracture of the bone
•
Injury to the vessels or nerves
Fixed Traction
•
Useful for when patient has to be
transported
•
Thomas’s splint
5
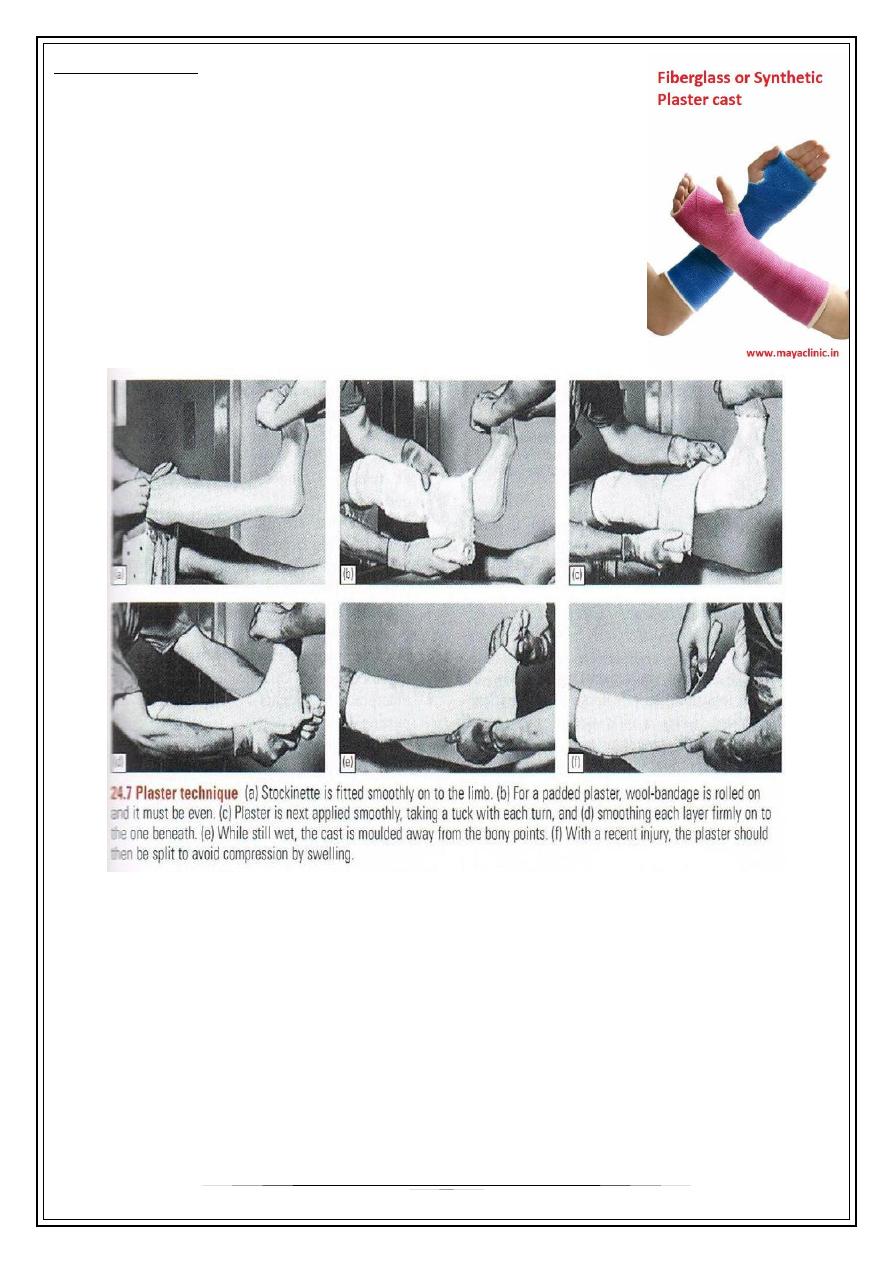
Cast Splintage
•
TYPES:
–
Plaster of Paris
–
Fibreglass
•
Especially for distal limb # and for most children #
•
Disadvantage: joint encased in plaster cannot move and
liable to stiffen
Complications of cast
•
Tight cast : too tight/limb swells
•
Pressure sores : press upon the skin over a bony prominence (the patella, the
heel)
•
Skin abrasion or laceration during removal of the plaster
6
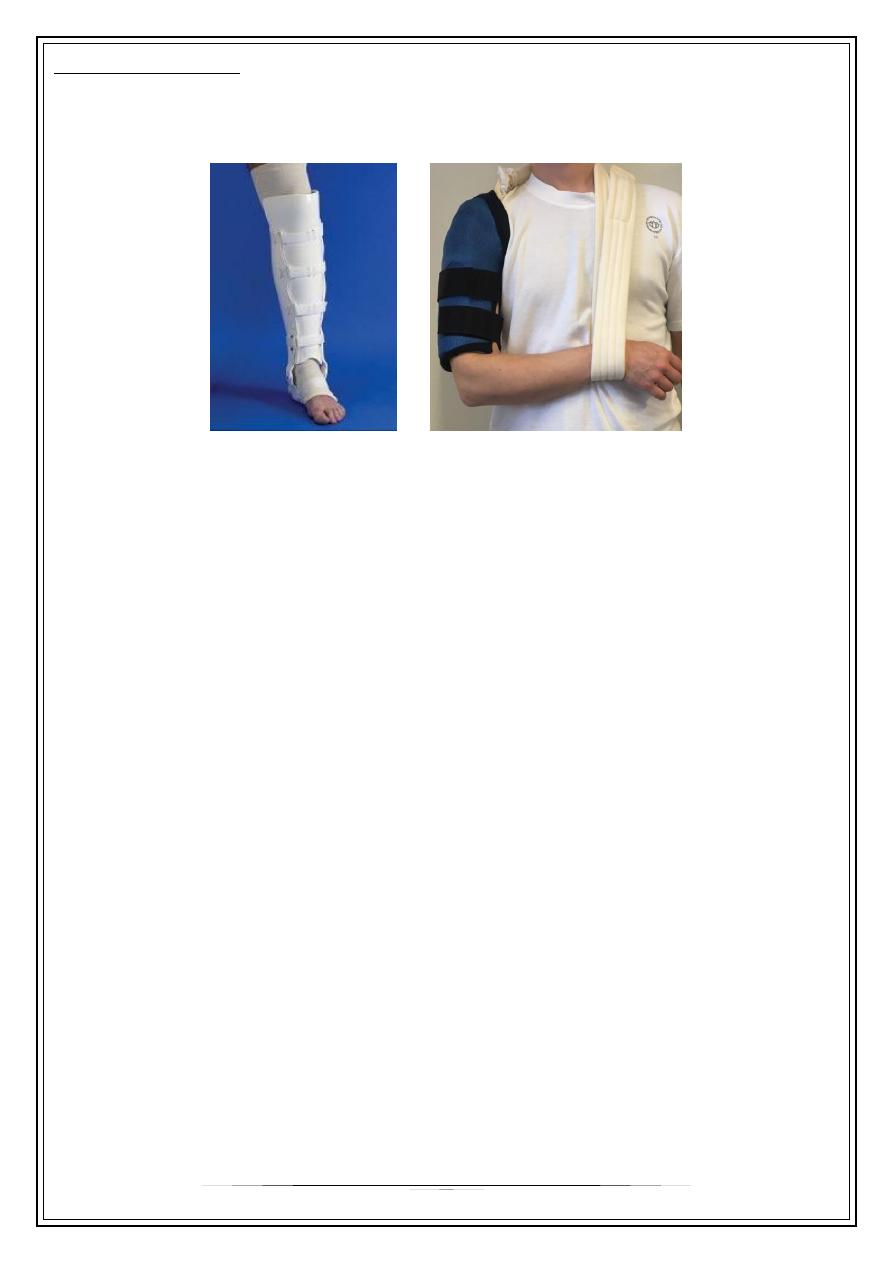
Functional Bracing
•
Brace supportive device that allows continued function of the part
•
Indication fractures of shaft of humerus or tibia
To be continued,,,
