fractures of the acetabulum & injuries to the
sacrum and coccyx
Fractures of the acetabulum
Fracture of the acetabulum occur when the head of the femur is
driven into the pelvis. This is caused either by a blow on the side (as
in a fall from height) or by a blow on the front of the knee as in
dashboard injury.
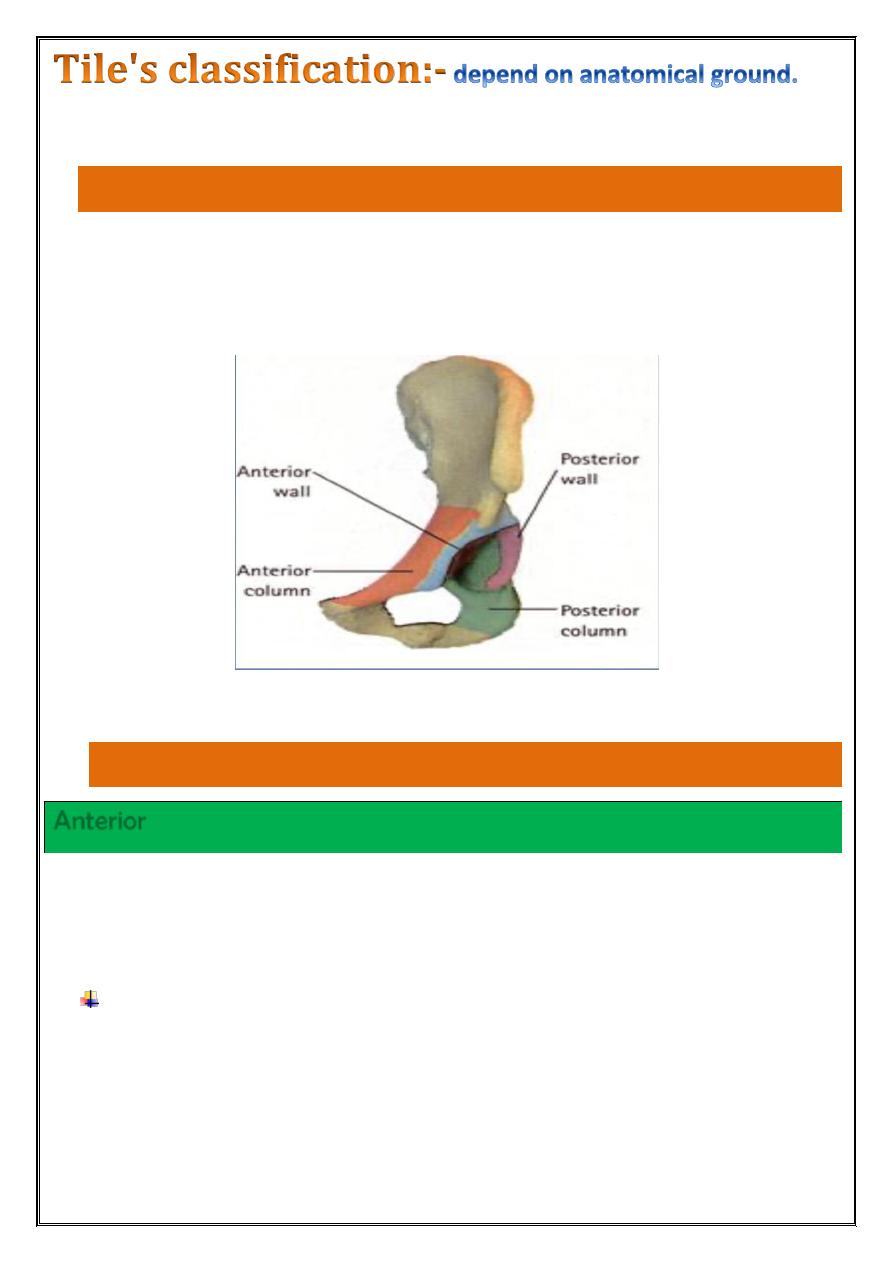
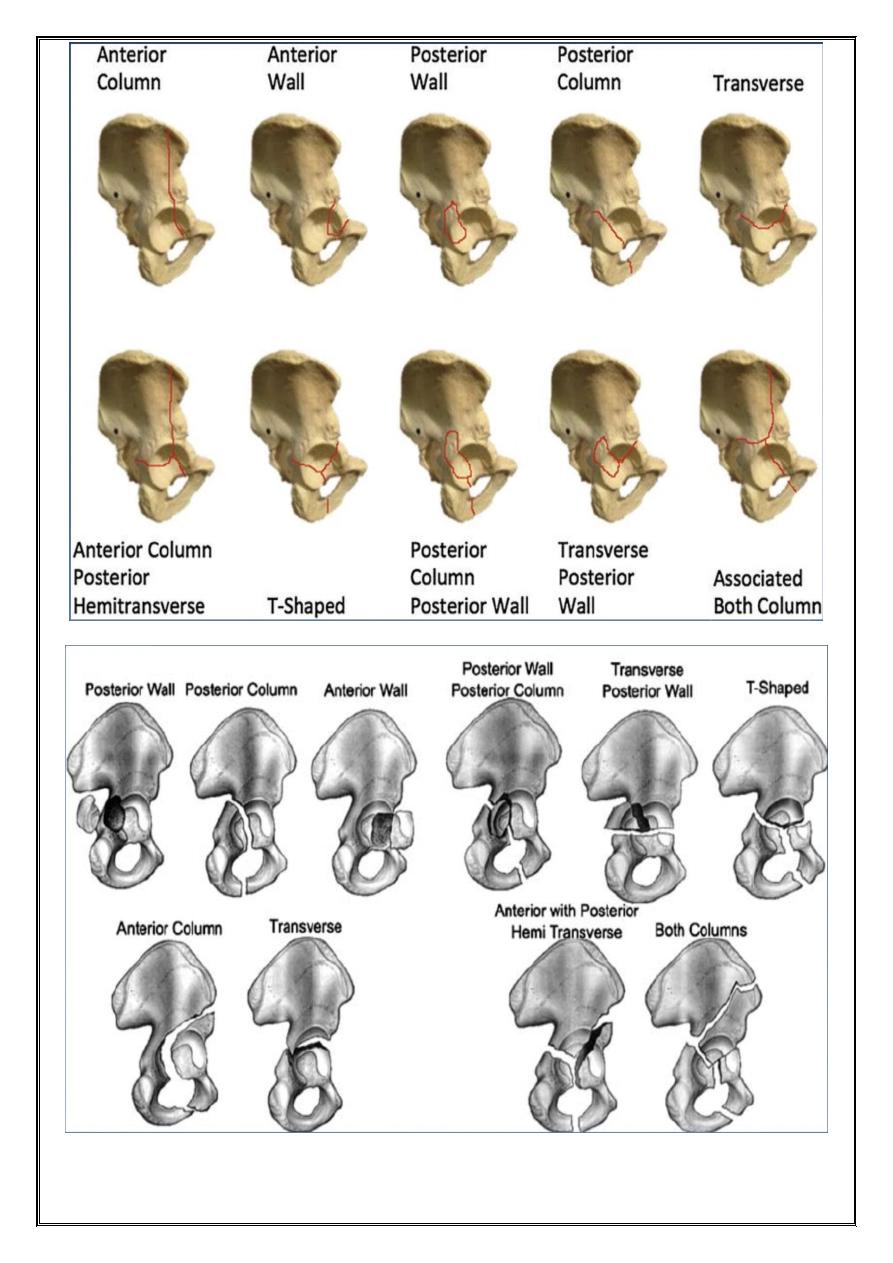
Acetabular wall(rim) fractures:-
fractures of the anterior or posterior part of the acetabular rim(wall)
affect the depth of the socket and may lead to hip instability unless
they are properly reduced and fixed.
Column fractures :-
Anterior
the anterior column extends from the pubic symphysis, along the
superior pubic ramus, across the acetabulum to the anterior part of
the ilium.
Anterior column fractures are uncommon, do not involve the
weight-bearing area and have a good prognosis.
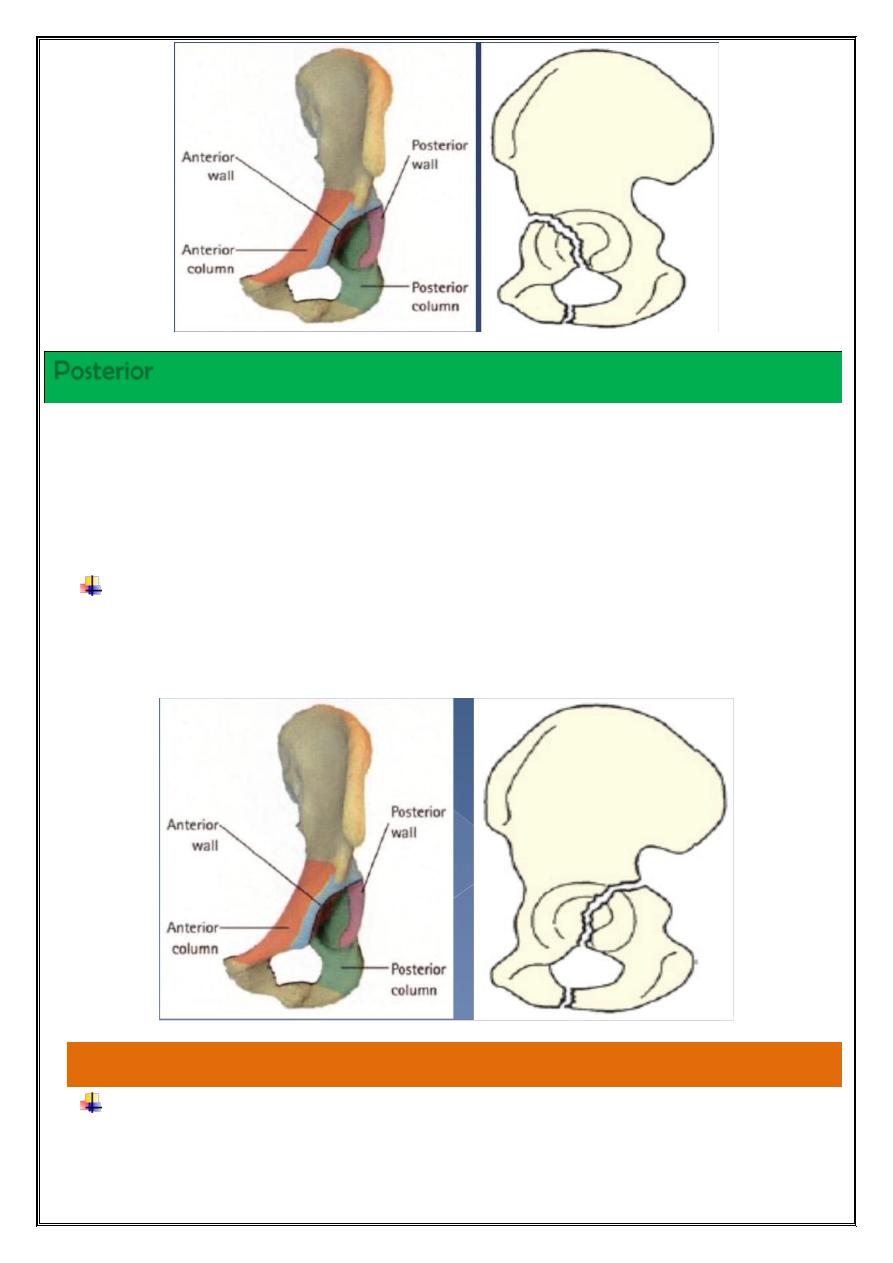
Posterior
The posterior column extends from the ischium, across the posterior
aspect of the acetabular socket to the sciatic notch and the posterior
part of the innominate bone. •Breaking the weight-bearing part of
the acetabulum.
It is usually associated with a posterior dislocation of the hip
and may injure the sciatic nerve. •Treatment is more urgent and
usually involves internal fixation to obtain a stable joint.
Transverse fracture:-
runs transversely through the acetabulum, involving both the
anterior and posterior columns, and separating the iliac portion
above from the pubic and ischial portions below.
A vertical split into the obturator foramen may coexist, resulting
in a T-fracture.
Difficult to reduce and to hold reduced
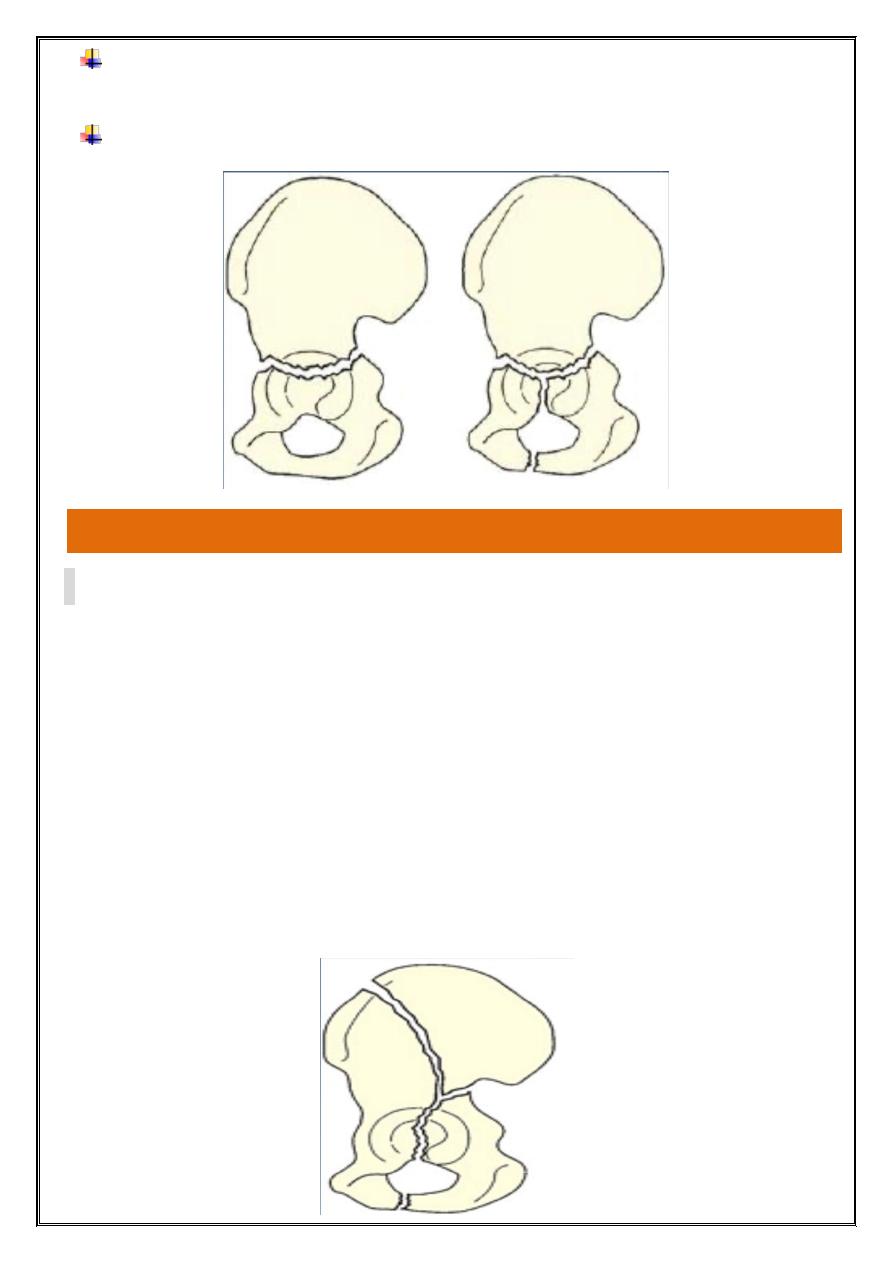
Complex fracture:-
•
are complex injuries which damage either the anterior or
the posterior columns (or both) as well as the roof or the
walls of the acetabulum.
•the injury is severe.
•The joint surface is disrupted.
•They usually need operative reduction and internal fixation.
•The end result is likely to be less than perfect, unless surgical
reduction
Clinical feature
Usually a severe injury; either a traffic accident or a fall from a
height.
Associated fracture:- whenever a fractured femur, severe knee
injury or a fractured calcaneum is diagnose, the hips also
should be x-rayed.
May be severely shocked, and the complications associated
with all pelvic fractures should be excluded.
Rectal examination is essential.
There may be bruising around the hip and the limb may lie in
internal rotation (if the hip is dislocated).
Careful neurological examination is important, testing the
function of the sciatic, femoral, obturator and pudendal
nerves.
Imaging
At least four x-ray views should be obtained in every case: a
standard anteroposterior view, the pelvic inlet view and two 45
degrees oblique views. Each view shows a different profile of the
acetabulum.
CT scans and three-dimensional re-formations are added
refinements, and are particularly helpful if surgical
reconstruction is planned.
Treatment
EMERGENCY TREATMENT
The first is shock and reduce a dislocation.
Skeletal traction to the distal femur (10 kg will suffice).
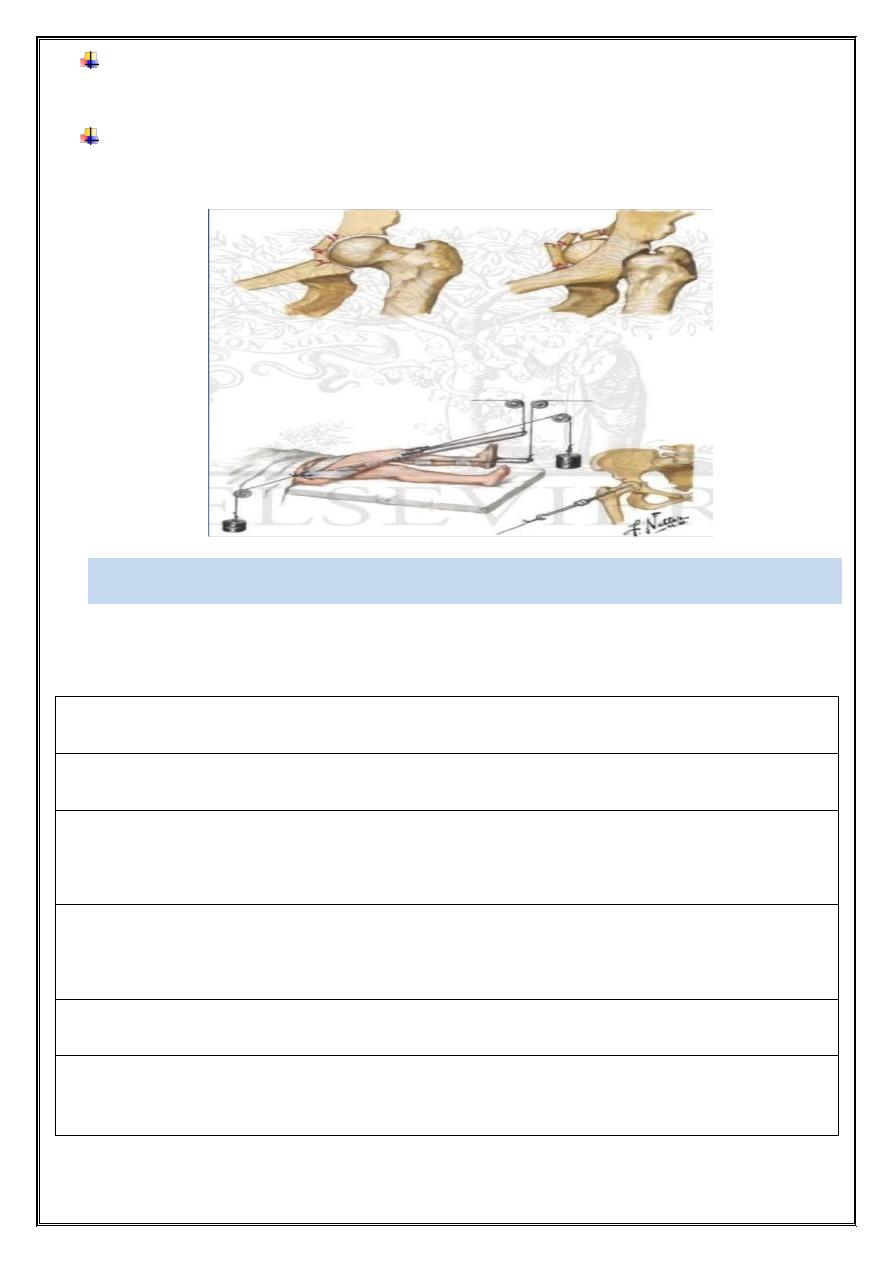
Occasionally, additional lateral traction through the greater
trochanter is needed for central hip dislocations.
Definitive treatment of the fracture is delayed until the patient is
fit and operation facilities are optimal.
NON-OPERATIVE TREATMENT
Conservative treatment : is still preferable in certain well-defined
situations:
-minimal displacement (in the weightbearing zone, less than 3 mm)
-not involve the superomedial weight bearing segment (roof) .
-a both-column fracture that retains the ball and socket congruence
of the hip.
-fractures in elderly patients, where closed reduction seems
feasible.
-patients with ‘medical’ contraindications, local sepsis)
-Comminution, unless adequate facilities and expertise are
available.
Non-operative treatment is more suitable for patients aged over
50 years than for adolescents and young adults.
If there are medical contraindications to operative treatment,
closed reduction under general anaesthesia is attempted.
In all patients treated conservatively, longitudinal traction, if
necessary supplemented by lateral traction, is maintained for 6–8
weeks; this will unload the articular cartilage and will help to
prevent further displacement of the fracture.
During this period, hip movement and exercises are encouraged.
The patient is then allowed up, using crutches with minimal
weight-bearing for a further 6 weeks.
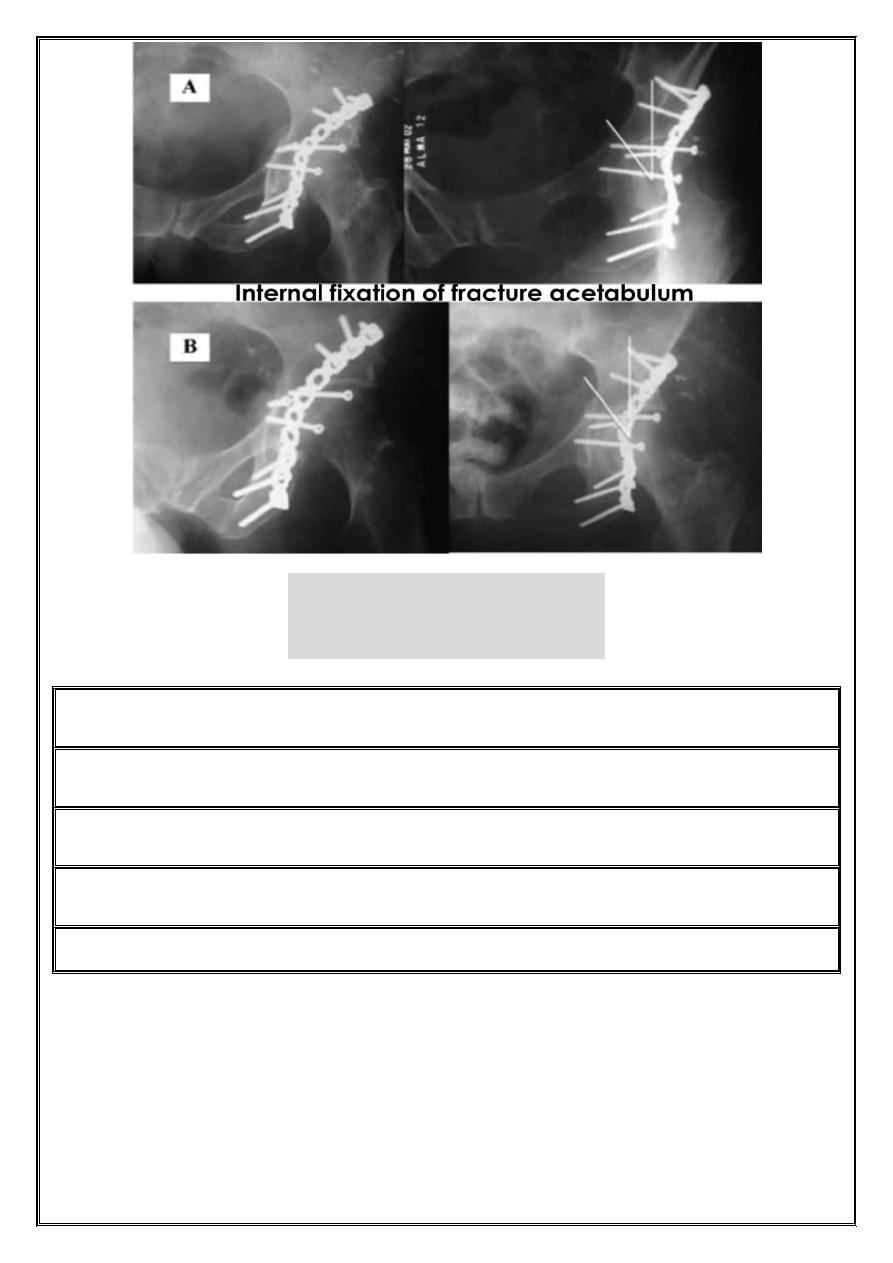
OPERATIVE TREATMENT
• indicated for all unstable hips.
•The hip may be dislocated centrally, anteriorly or posteriorly.
•The fracture (or fractures) is fixed with lag screws or special
buttressing plates.
•Prophylactic antibiotics are used.
•Postoperatively hip movements are started as soon as possible.
•Some prophylaxis against heterotopic ossification is often used,
usually indomethacin.
•The patient is allowed up, partial weightbearing with crutches, after
7 days.
•Exercises continued for 3–6 months; it may take a year or longer for
full function to return.
Complications
o Iliofemoral venous thrombosis
o Sciatic nerve injury
o Hereterotopic bone formation
o Avascular necrosis
o Loss of joint movement and secondary osteoarthritis
INJURIES TO THE SACRUM AND COCCYX
•blow from behind.
•Fall in to tail.
•Women seem to be affected more .
•Bruising.
•Tenderness.
•Sensation may be lost over sacral n.
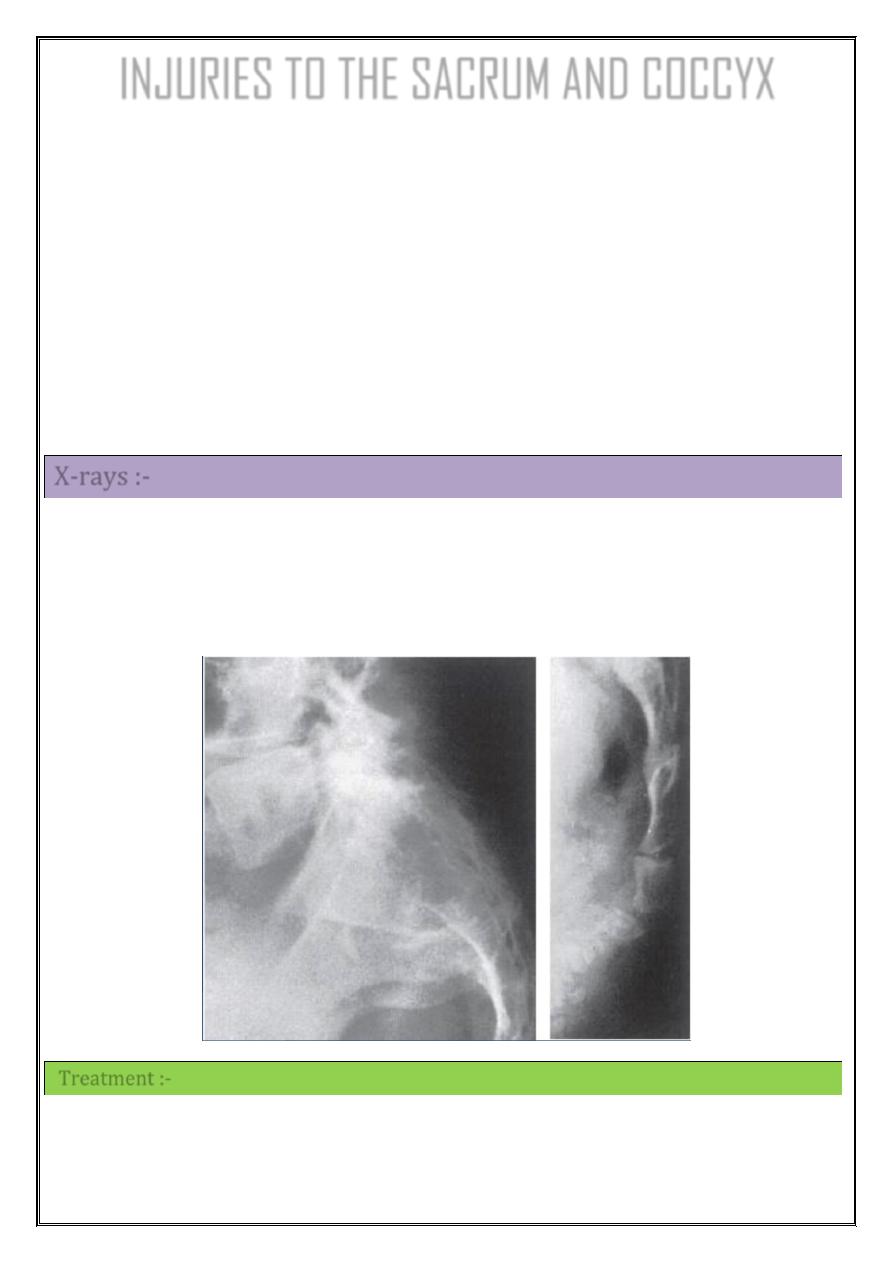
X-rays :-
1- transverse fracture of the sacrum.
2- Fractured coccyx.
3- normal appearance if the joint sprain.
Treatment :-
•reduction by a finger in the rectum.
•The reduction is stable.
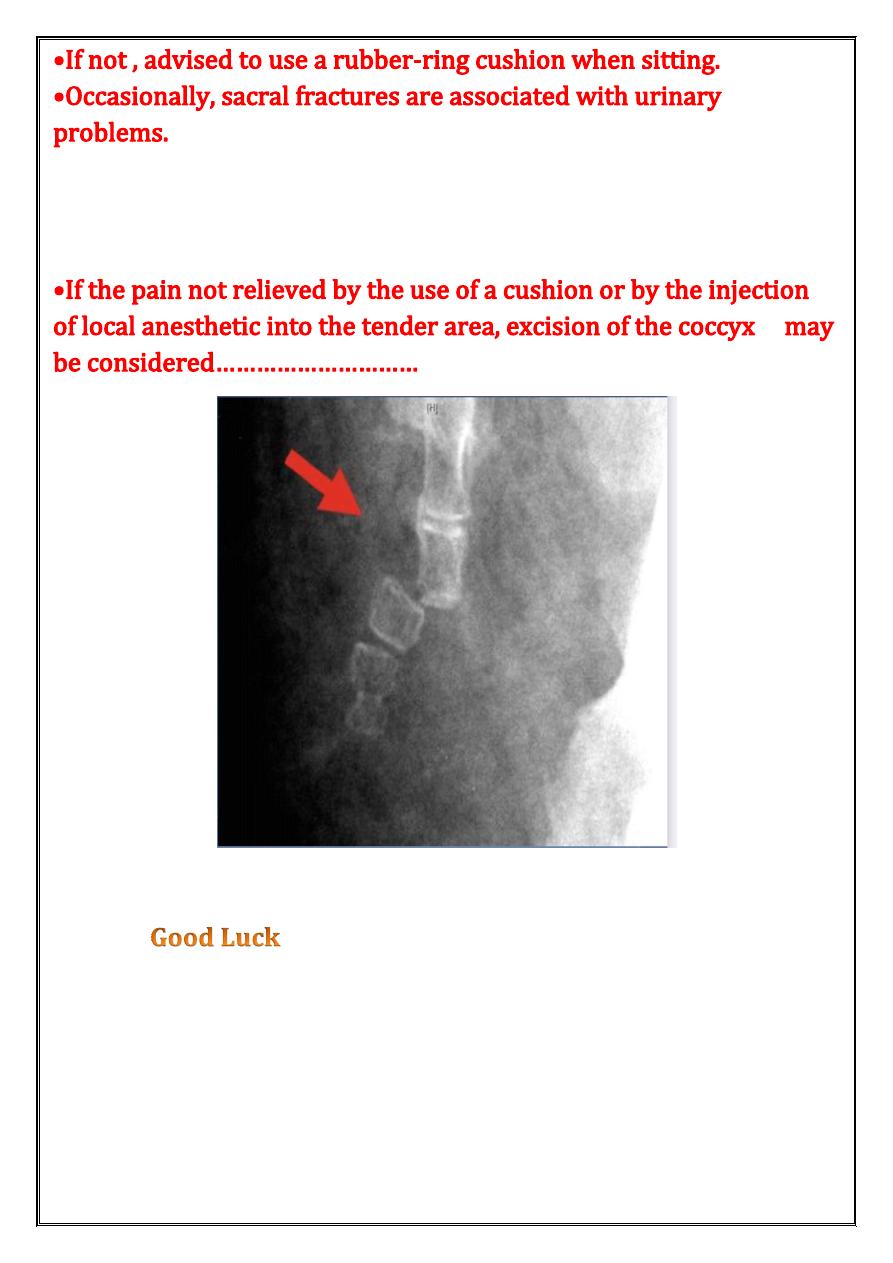
•Laminectomy.
•Persistent pain on sitting is common after coccygeal injuries.
