1
Orthopedic Surgery
5
th
Stage
Metacarpal & Phalangeal Fractures
Metacarpal fracture
:
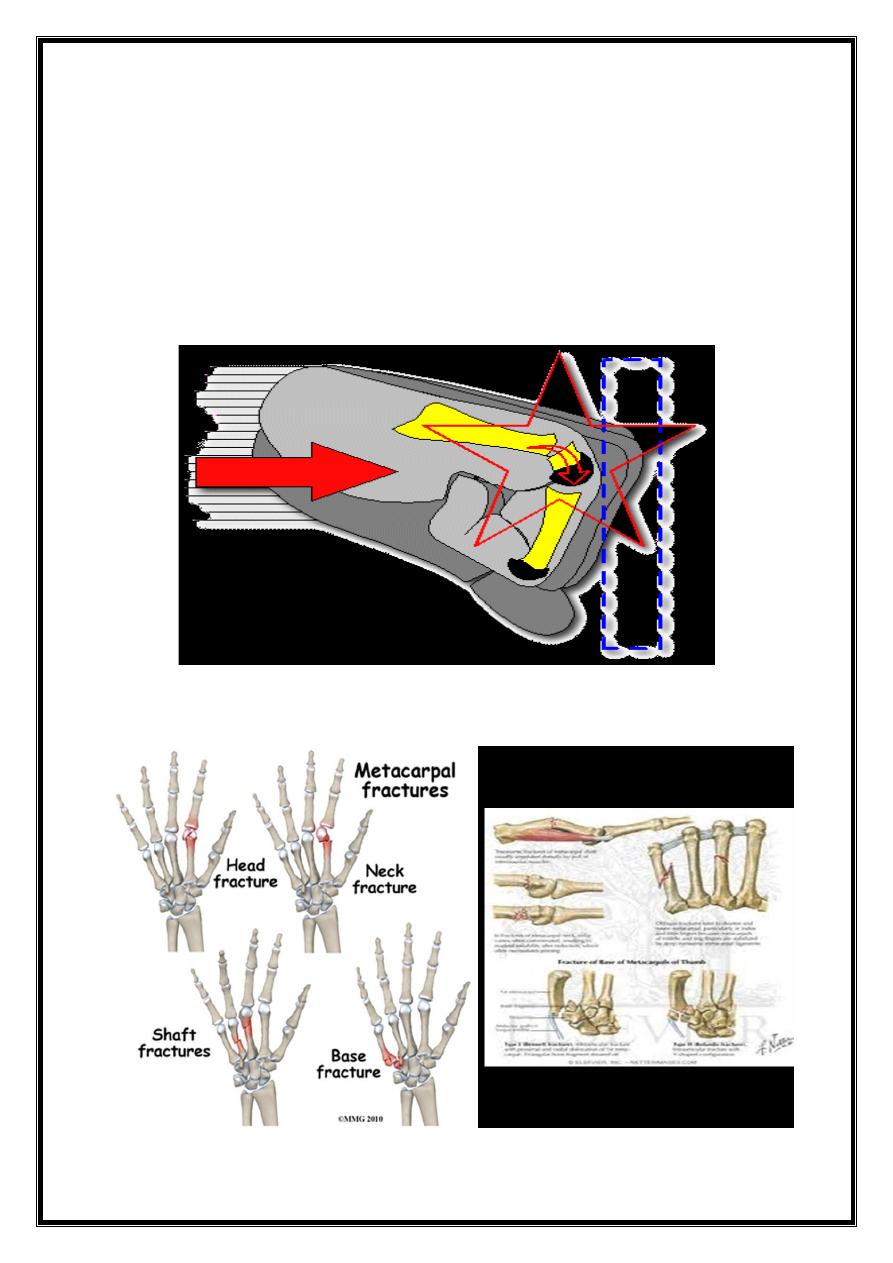
Caused by blow, fall, or longitudinal force (boxers punch).
Site: base, shaft, neck.
2
Deformity:
1. Angular: {transverse#} not very marked, doesn’t interfere much
with function.
2. Rotational: {spiral #} serious, malrotation will result in overlap of
fingers when patient closes the fist.
Metacarpal shaft fracture
Transverse: caused by direct blow.
Spiral: caused by twisting or punching force.

3
Treatment :
Transverse #:
1. slight displacement; just crepe bandage.
2. Considerable displacement: closed reduction & plaster slab for 3 weeks.
If reduction is unstable, then open reduction & internal fixation by plate
& screws, or percutaneous k –wire across the fracture line.
Spiral #:
liable to rotate so treated by open reduction& internal fixation
.
4
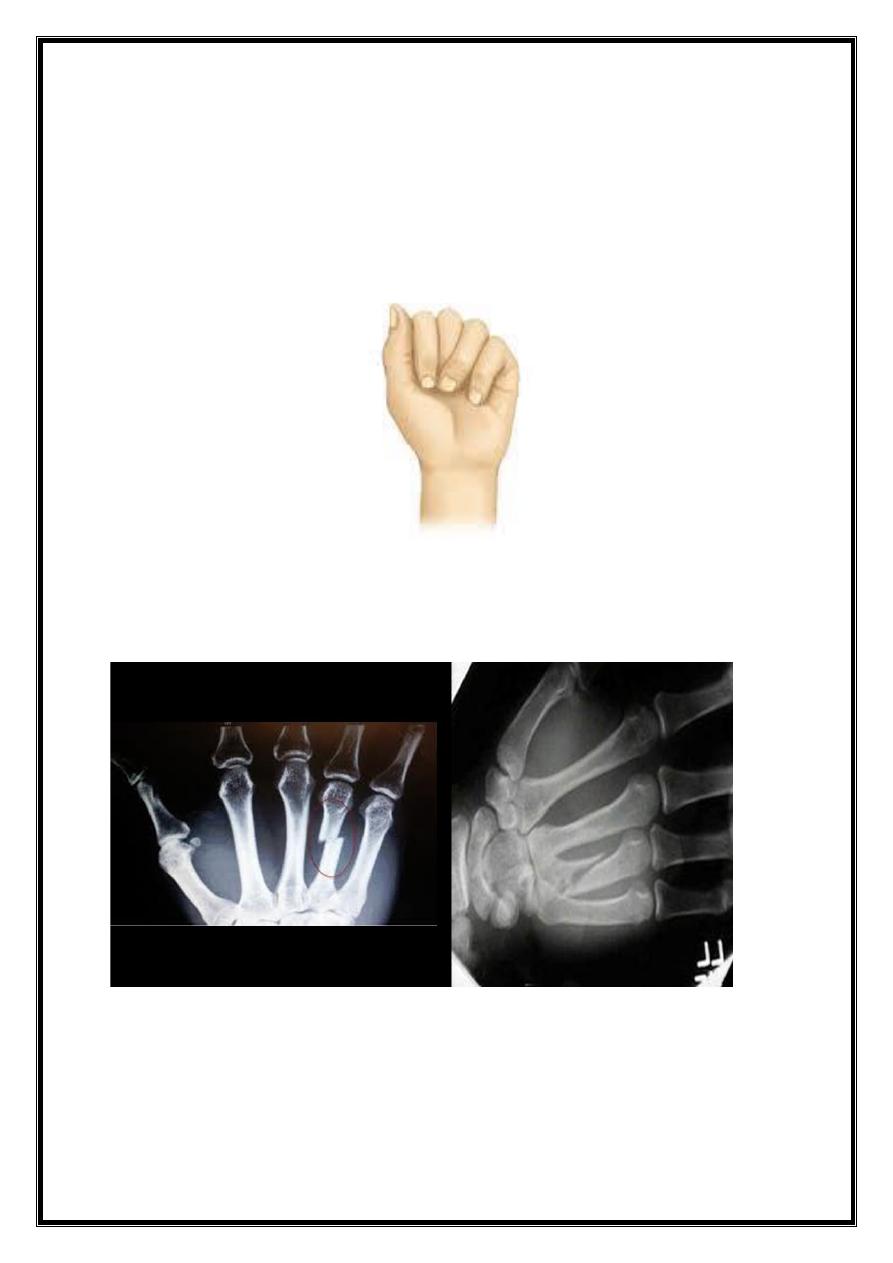
Metacarpal neck (boxer #)
Usually the fifth finger.
Usually local swelling with flattening of the knuckle.
X-ray: transverse #, impacted with volar angulation of the
distal fragment.
Treatment:
Ringe & Littile finger
Up to 40 D angulation deformity can be accepted, apply gutter plaster with
MP joint flexed & IP joints extended for 2 weeks.
Index & middle finger,
no more than 20 D angulation can be accepted.
IF reduction is needed, try closed reduction under L.A followed by
immobilization in a gutter plaster.
For unstable frcactures do open reduction &internal fixation by K-
wires .
5
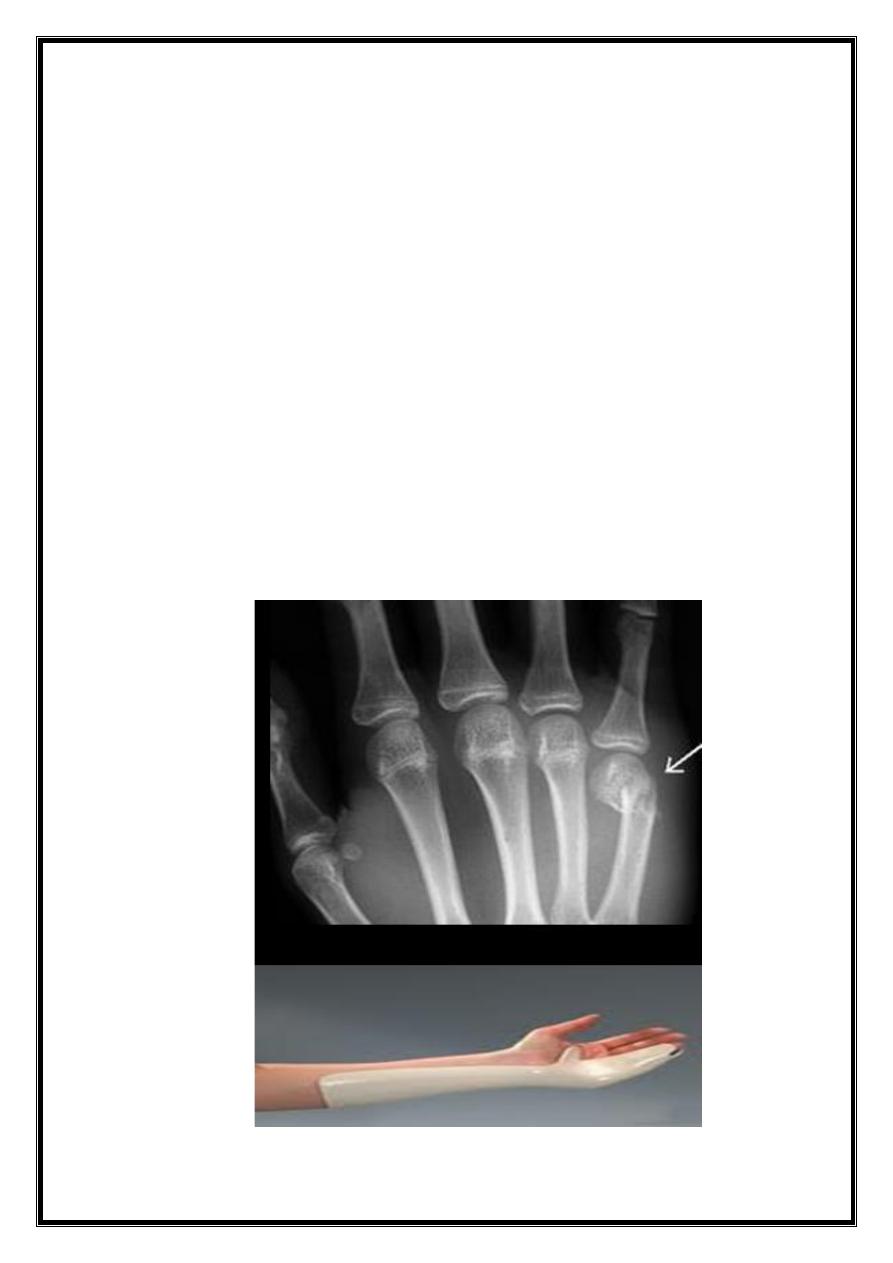
Metacarpal base #
Except 1st metacarpal (thumb), these are stable #, treated by volar slab,
extending from the forearm to PIP joint for 3 weeks. Just ensure that rotation is
corrected.
Displaced intraarticular # of the base of 4th &5th Metacarpal: these are
mobile joints, so joint incongruity will be painful, so do closed reduction
&percutaneous k-wire or compression screw.
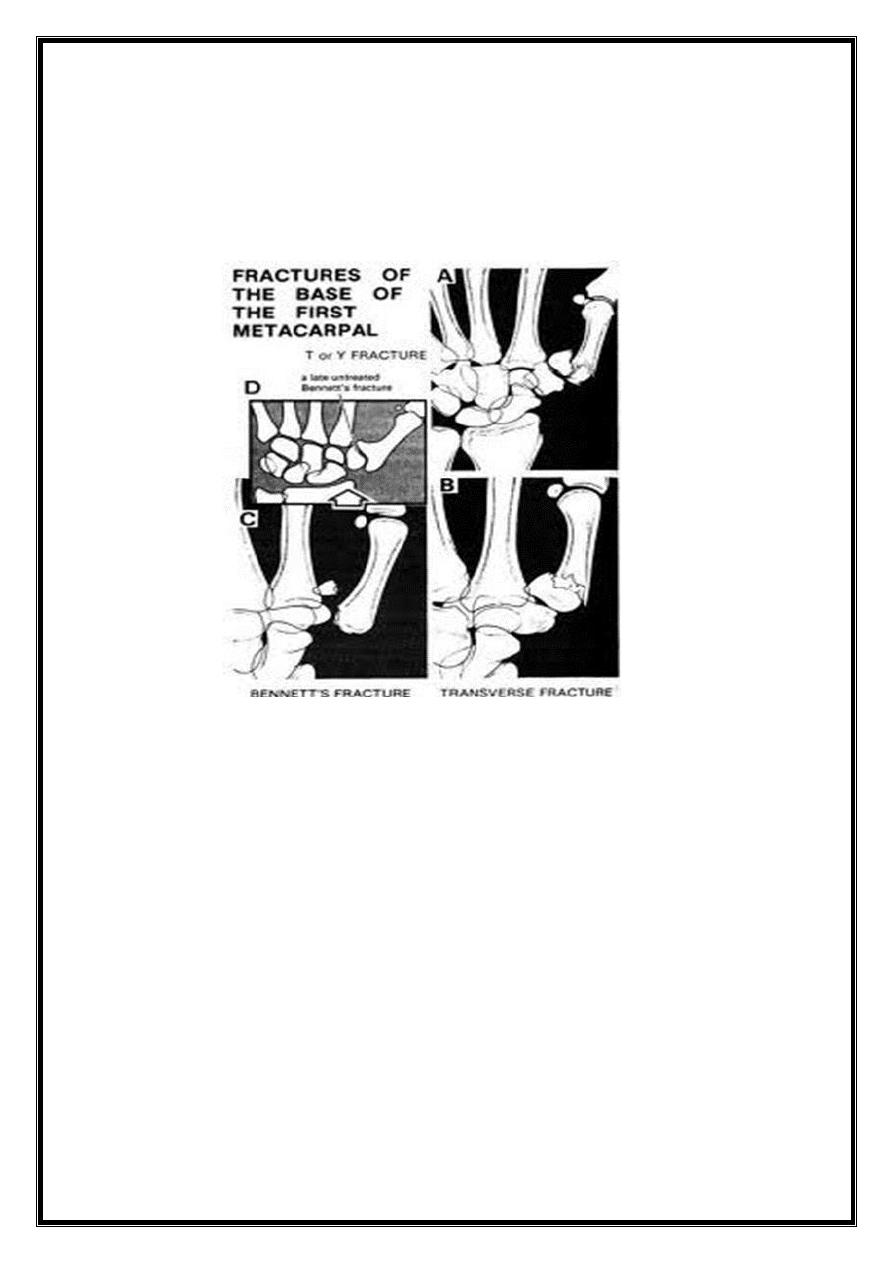
Fracture of thumb metacarpal base
1. Impacted # of the MTC base.
2. Bennet fracture dislocation of carpometacarpal joint.
3. Rolando comminuted # of the base.
6
1. Impacted fracture:
Transverse # 6 mm distal to CMC joint.
TRT: <20-30 D angulation, apply thumb Spica for 2-3 weeks.
> 30 D, closed reduction & thumb spica.
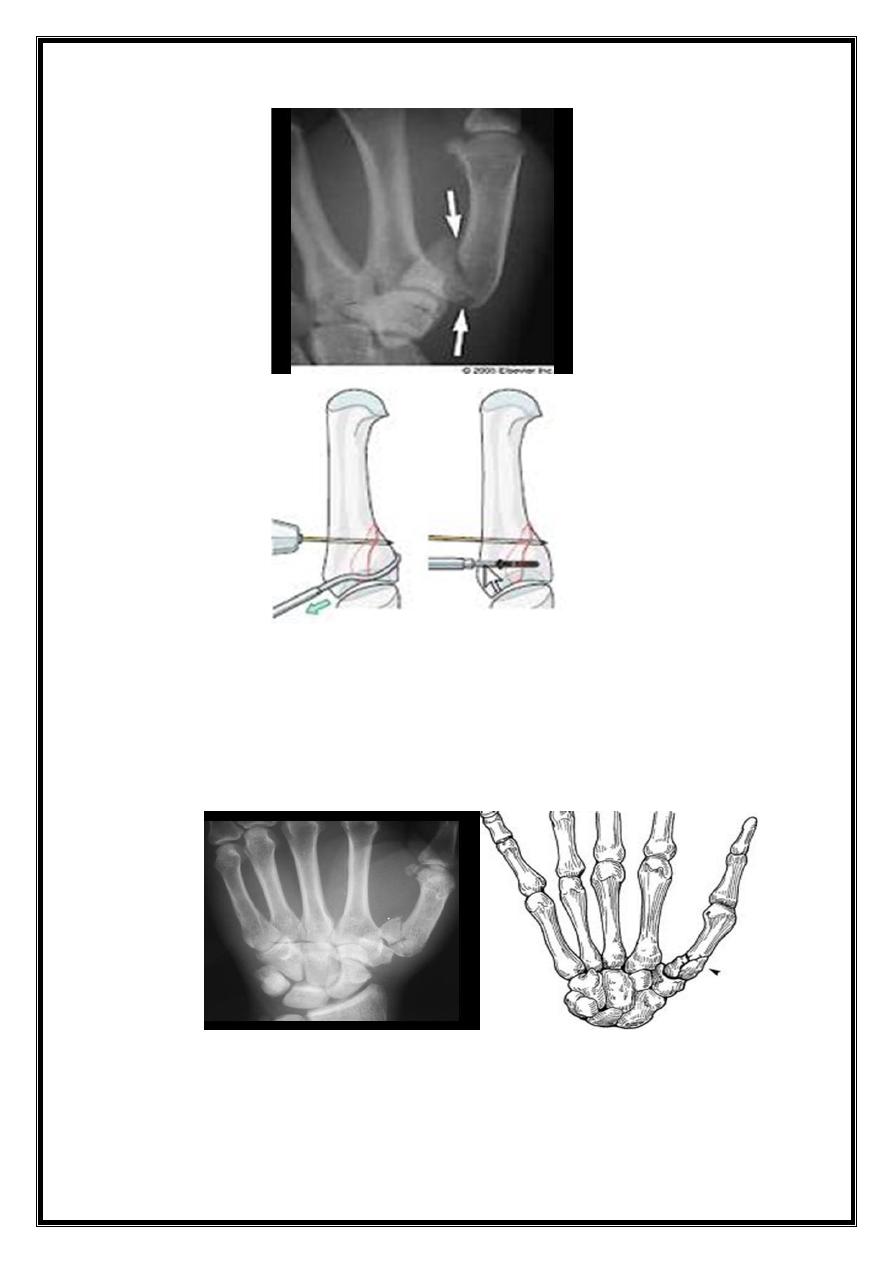
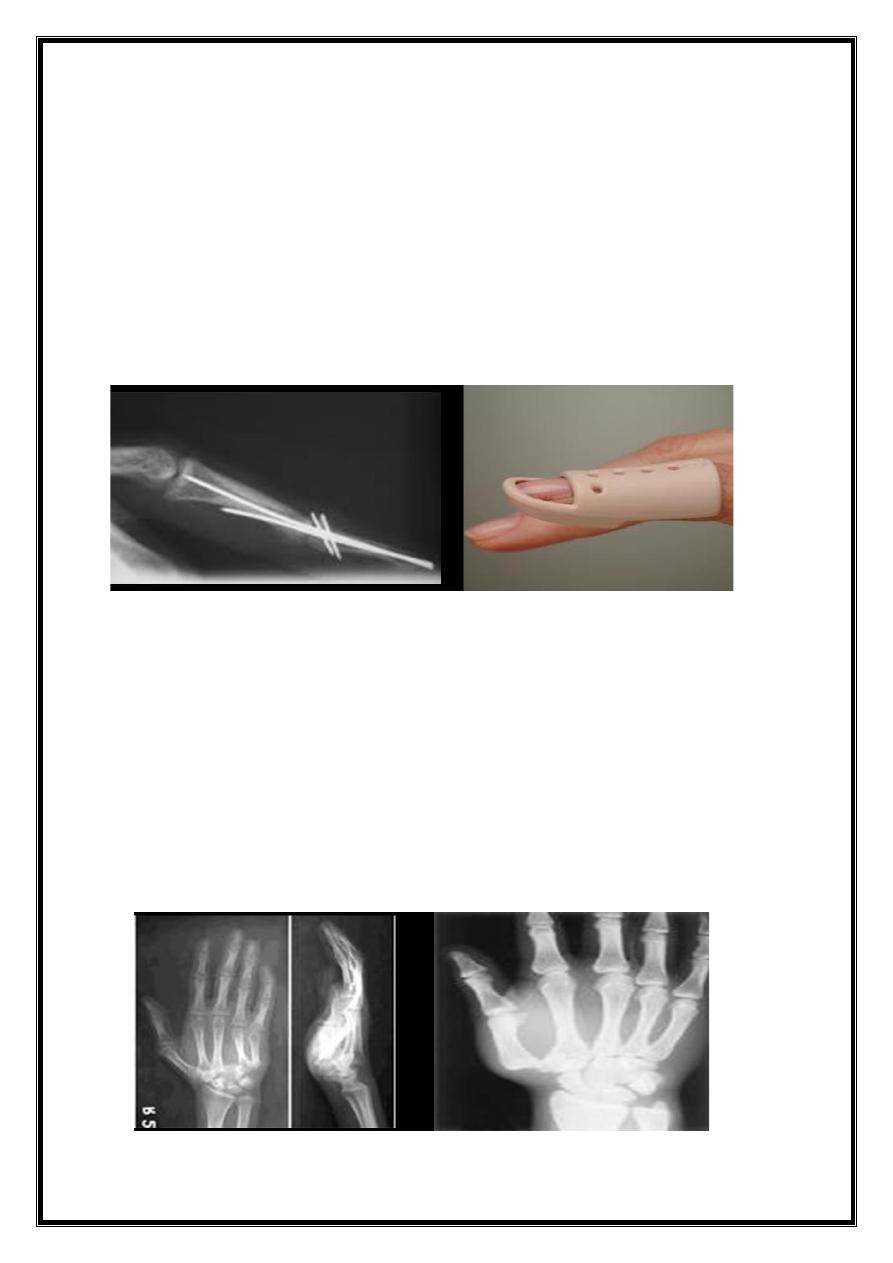
2. Bennet fracture
Oblique fracture, extend into carpometacarpal (intraarticular) & unstable.
Treatment:
Try closed reduction &POP cast.
If failed,do closed reduction & percutaneous K wire fixation, or
open reduction & internal fixation by compression screw.
7
3. Rolando fracture:
Comminuted intra-articular # of the base of 1st metacarpal
Treatment:
closed reduction &k-wire fixation
external fixation for more sever comminution.
8
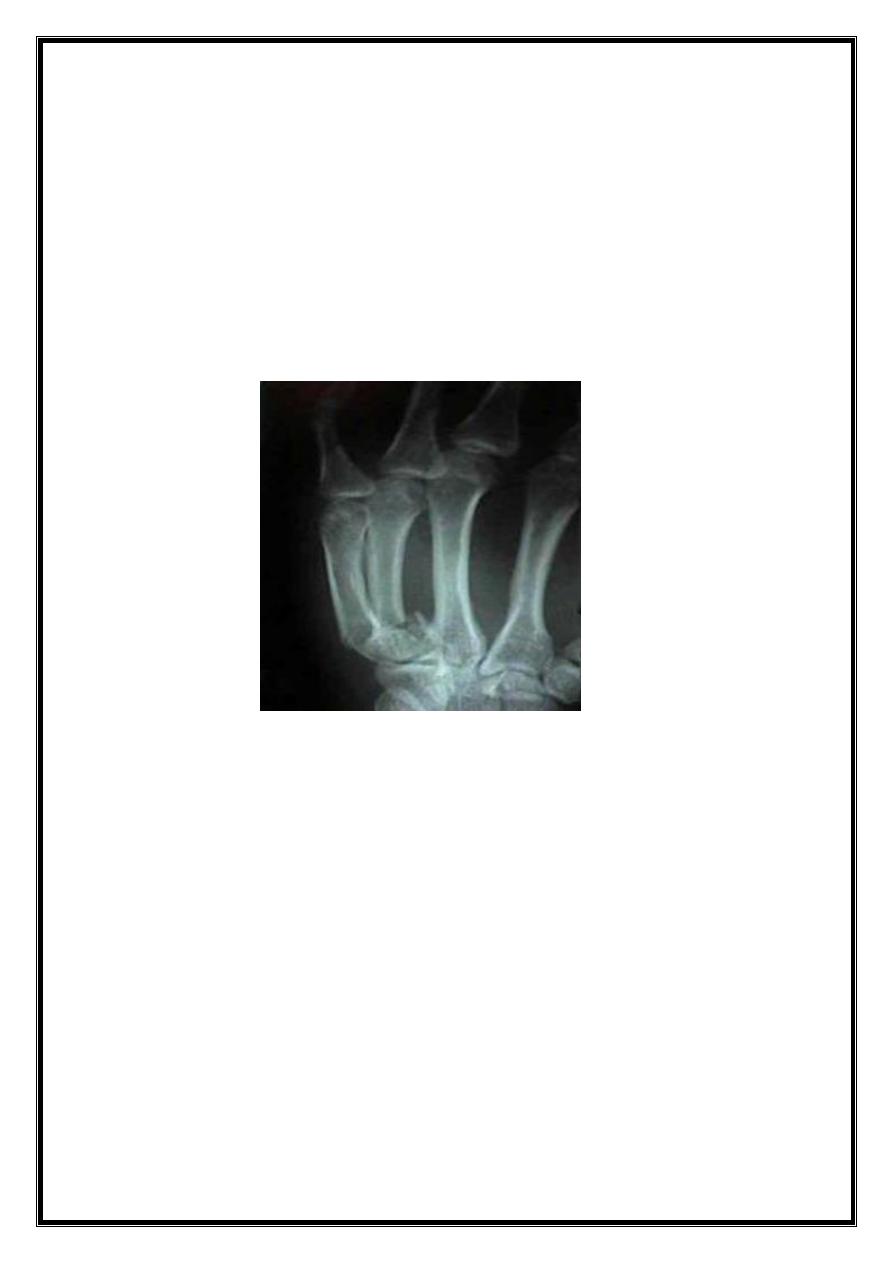
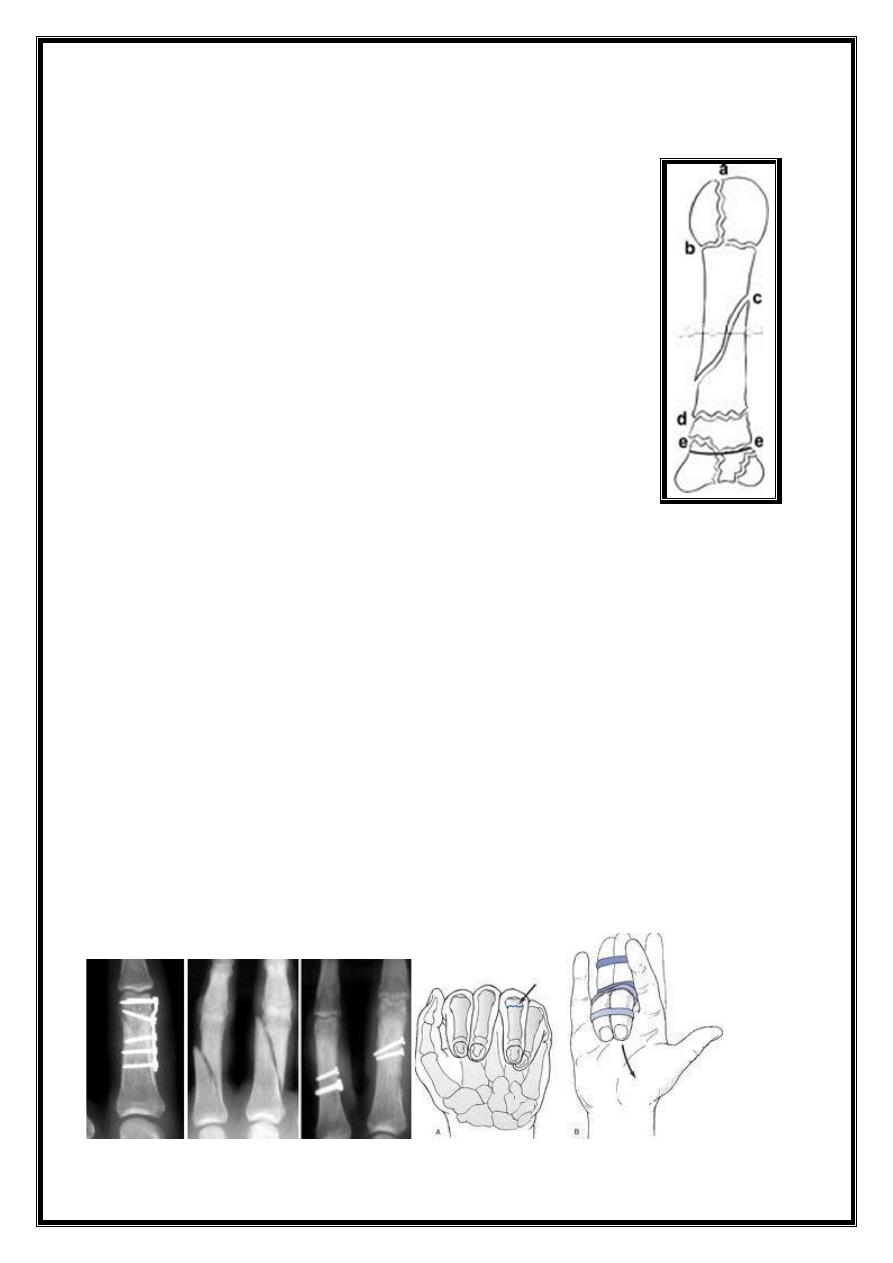
Fracture phalanges
Cause:
Direct trauma.
Fracture proximal & middle phalanges:
Transverse #: usually angulated.
Spiral #: rotation deformity.
Comminuted #: (tendon damage & skin loss).
Avulsion #: of small fragment of bone.
Intra-articular fracture:
Treatment:
Undisplaced #: functional splintage by strapping the
fractured finger to its neighbor (buddy strapping).
Displaced #: reduced; correct rotation & angulation. Apply
dorsal splint with MP joint in 80 D flexion & IP joint in
extension for 3 weeks.
Indication for internal fixation:
1. Closed reduction cannot be achieved.
2. Unstable #.
3. Intra-articular #.
9
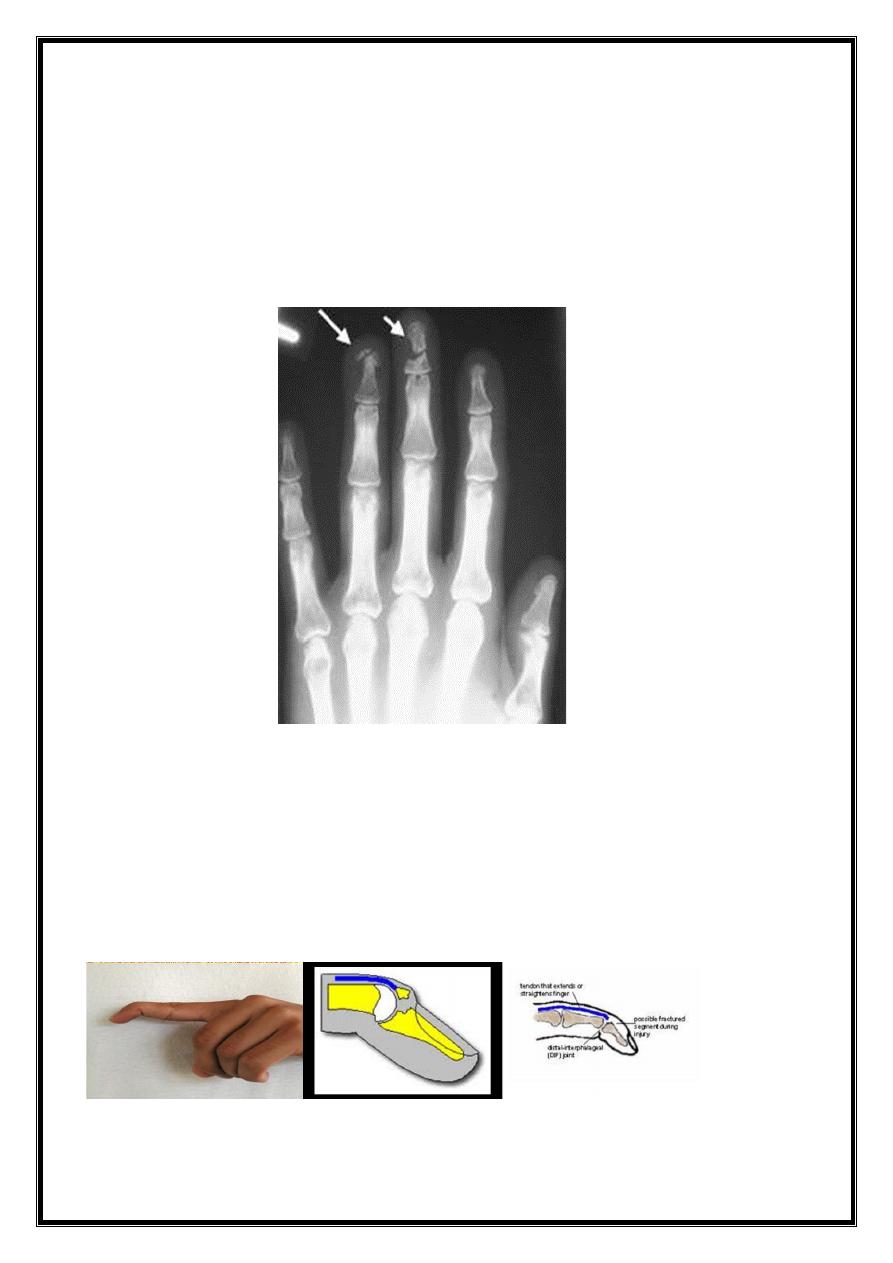
Fracture distal phalanx:
# of the tuft: fingertip struck by hammer, or caught by a door,
the bone shattered.
Treatment: disregard the #, control swelling & regain
movement. Painful hematoma beneath finger nail should be
drained.
Mallet finger injury (baseball finger):
Cause:
1. rupture of extensor tendon at or near its insertion at terminal
phalanx.
2. avulsion #of the base of terminal phalanx.
C/F: Terminal phalanx drops & patient unable to straighten it
.
10
Treatment:
Tendinous avulsion:
splint DIP joint in hyperextension,
using a special splint, constantly for 8 weeks, then only
at night for 4 weeks.
Bony avulsion:
also splint DIP joint in hyperextension
for 6 weeks. For large bony avulsion associated with
subluxation of DIP joint, fixation of the fragment with K
wire or a small screw.
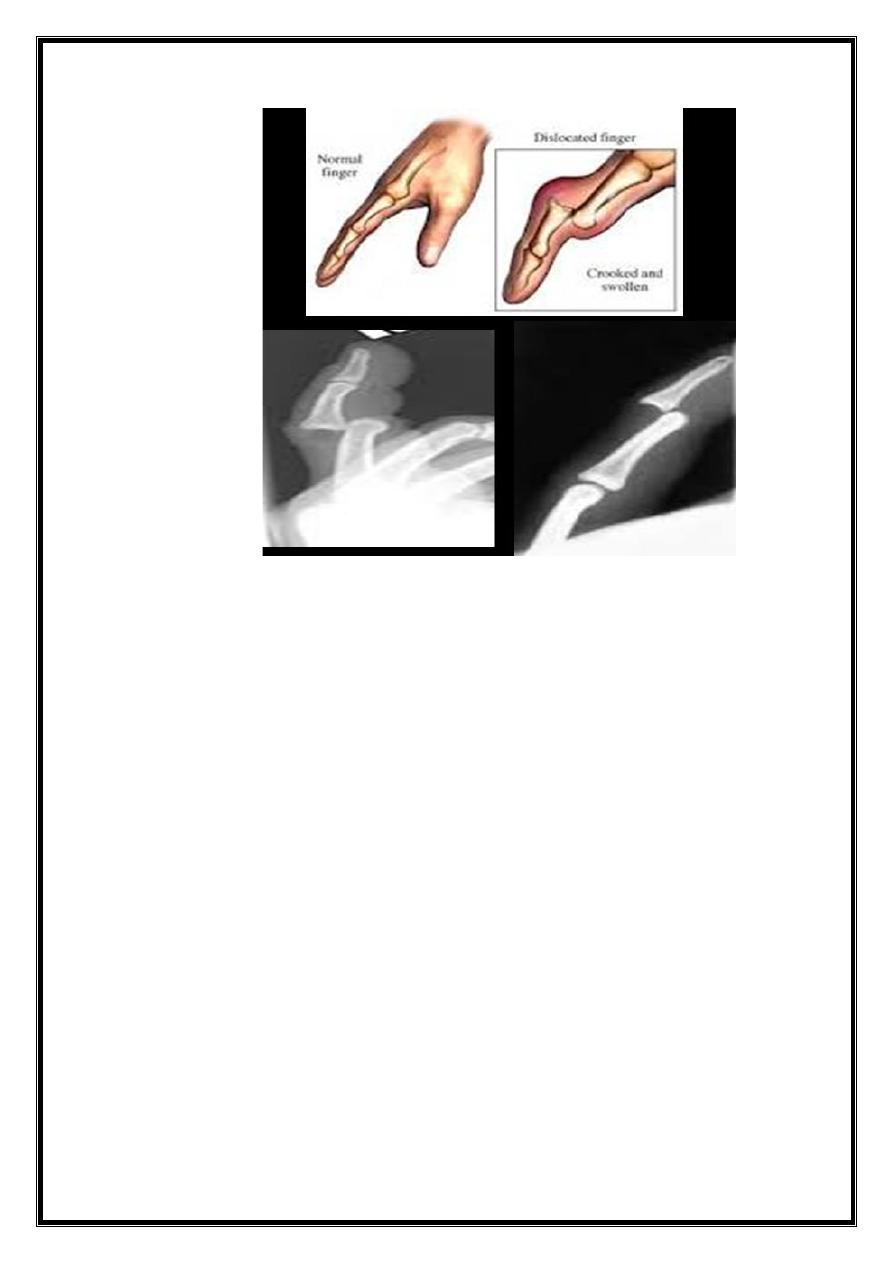
Dislocations in the Hand
Carpo-metacarpal dislocation
Mostly in the thumb, it resembles Bennetts fracture
dislocation.
Treatment: closed reduction is easy, but unstable, so; fix
by k wire which is kept for 5 weeks but protective splint
should worn for 8 weeks (risk of instability).

11
Metacarpo-phalageal dislocation
Usually the thumb, sometimes the 5th finger.
The finger is suddenly forced into hyper extension.
TRT: trial of closed reduction (usually difficult to reduce). If
failed, then open reduction through dorsal approach.
Interphalangeal dislocation
Distal interphalangeal dislocation is rare.
Proximal interphalangeal dislocation is more common
Mechanism: hyperextension force.
TRT:
closed reduction (easily done), strapping the finger to
its neighbor for few days.
If there is # fragment which is big &associated with
dislocation, open reduction of the fragment &
fixation by small screw or k-wire.
12
Open hand injuries
Very common.
Types:
1. Tidy or clean cuts
2. Laceration
3. Crushing or injection injuries
4. Burns &finger bulb defects
Clinical assessment:
Mechanism: instrument; Sharp or blunt?? Clean or dirty??
Severity?
Position of the fingers: (flexed or extended??) at injury.
Timing:
Age: of the patient
Occupation:
Dominancy: right or left handed
13
Clinical examination
Skin: assess the degree of skin damage small wounds, be
alert!!, possibility of misdiagnosis
Circulation: careful evaluation of the state of hand
circulation, Perform (Allen test).
Nerve examination: assess function of the peripheral
nerves.
Tendon: assess the function of extensor tendons & long
flexor tendons.
Bones: any fractures
X-ray: AP, lateral & oblique view.
Primary treatment:
Preoperative care:
Treatment of pain & shock
Wound rinsed with plenty of normal saline
Antibiotics
Anti-tetanus &Anti gas gangrene prophylaxis
Wound dressed &hand splinted
Wound exploration:
Under G.A, skin debrided but here skin is very precious,
original wound is enlarged (must not cross skin creases)
Dead muscle excised, wound irrigated with saline
Further assessment of extent of injury.
Tissue repair:
# reduced & fixed by k-wire or external fixation.
Joint ligament & capsule: repaired
Artery& vein: repaired if the hand or finger is ischemic
Nerves: repaired (operating microscope)
Extensor tendon: repaired
Flexor tendon: repair is more challenging.
Closure: unless wound contaminated, skin is closed by
direct suture without tension or, if there is skin loss, by
skin grafting or local flaps.
