Bone imaging
lecture (1)
5
TH
stage
By
Dr. Firas Abdullah
Thiqar college of medicine
Aims of our lecture:
To know the different radiological techniques used in
bone imaging, and what are their advantages and
disadvantages.
To know different bone pathologies.
To differentiate benign from malignant nature of a bony
lesion.
See some examples of bony lesions
I) Radiological techniques used in bony
imaging:
Plain X ray
Ultrasonography
CT scan
MRI
Radionuclide bone scanning
Plain X ray
• Advantages:
• Disadvantages:
The signs of bone disease on plain X ray
Decrease in bone density, which may be focal or generalized. Focal
reduction in density is usually referred to as a ‘lytic area’ or an area of
‘bone destruction’. When generalized, decrease in bone density is
best referred to as ‘osteopenia’
Increase in bone density (sclerosis), which may also be focal or
generalized.
Periosteal reaction. The periosteum is not normally visible on a
radiograph. The term ‘periosteal reaction’ refers to excess bone
produced by the periosteum, which occurs in response to such
conditions as neoplasm, inflammation or trauma.
The signs of bone disease on plain X ray
Alteration in trabecular pattern is a complex response usually
involving a reduction in the number of trabeculae with an alteration
in the remaining trabeculae, e.g. in osteoporosis and Paget’s disease
Alteration in the shape of a bone is another complex response with
many causes.
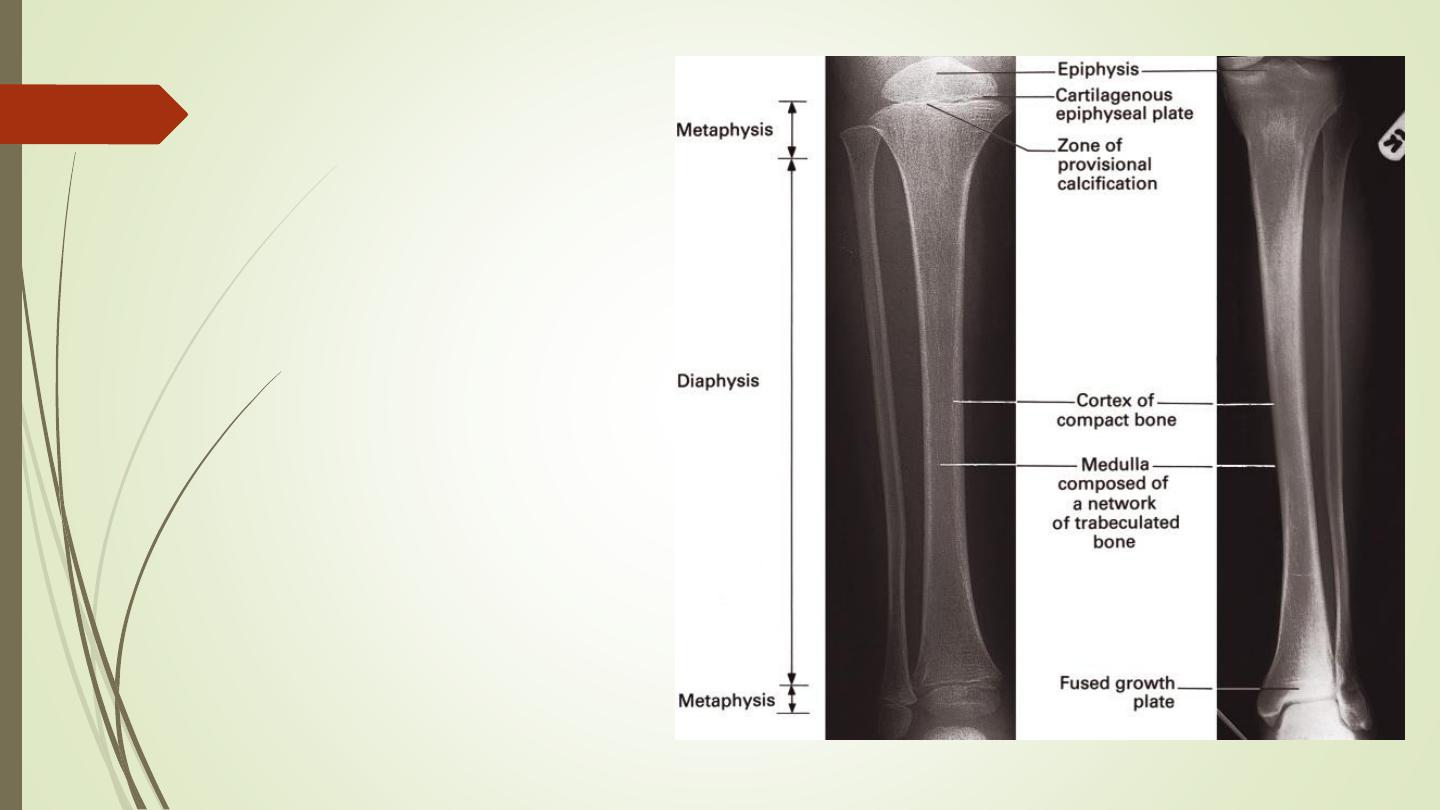
Alteration in bone age. The time of appearance of the various
epiphyseal centers and their time of fusion depends on the age of
the child.
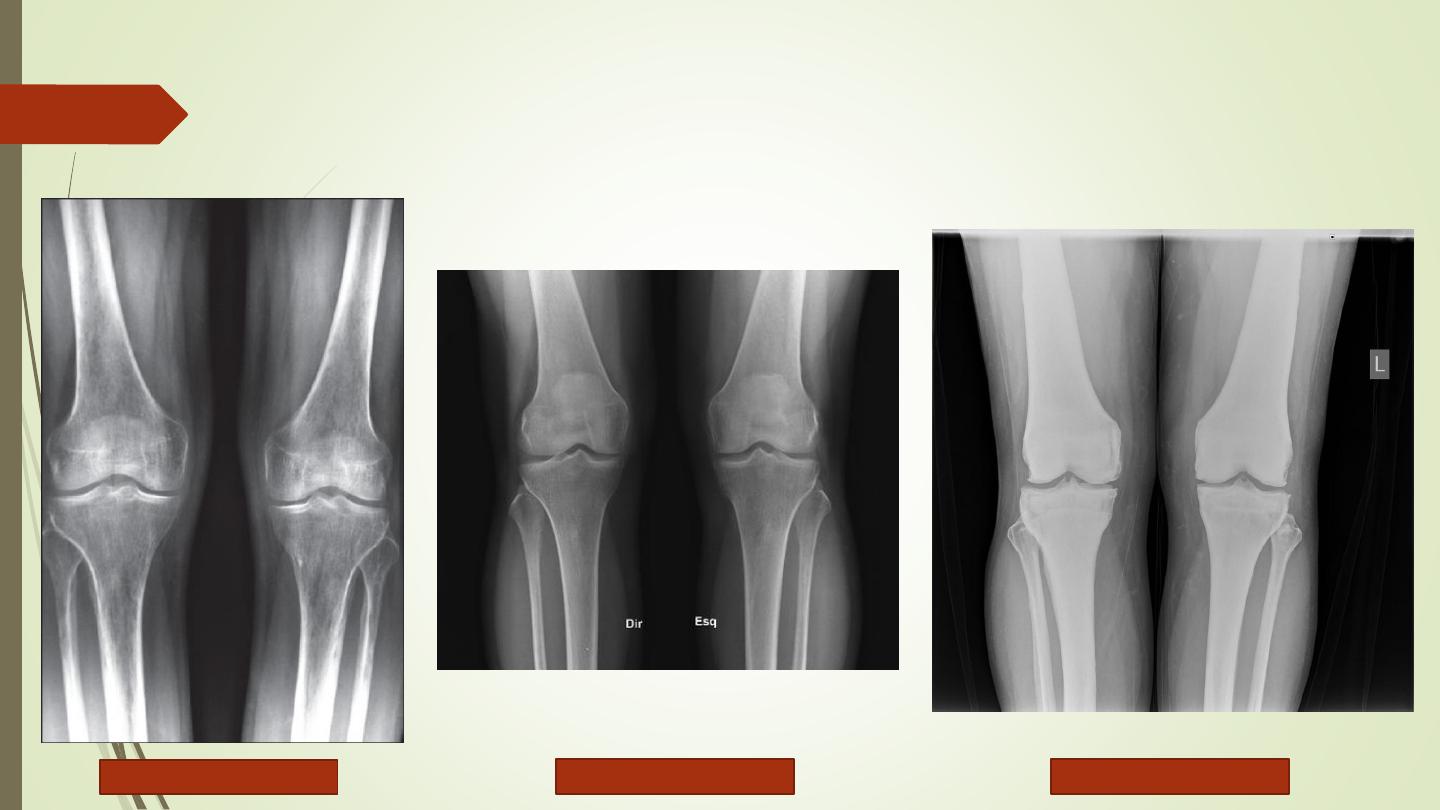
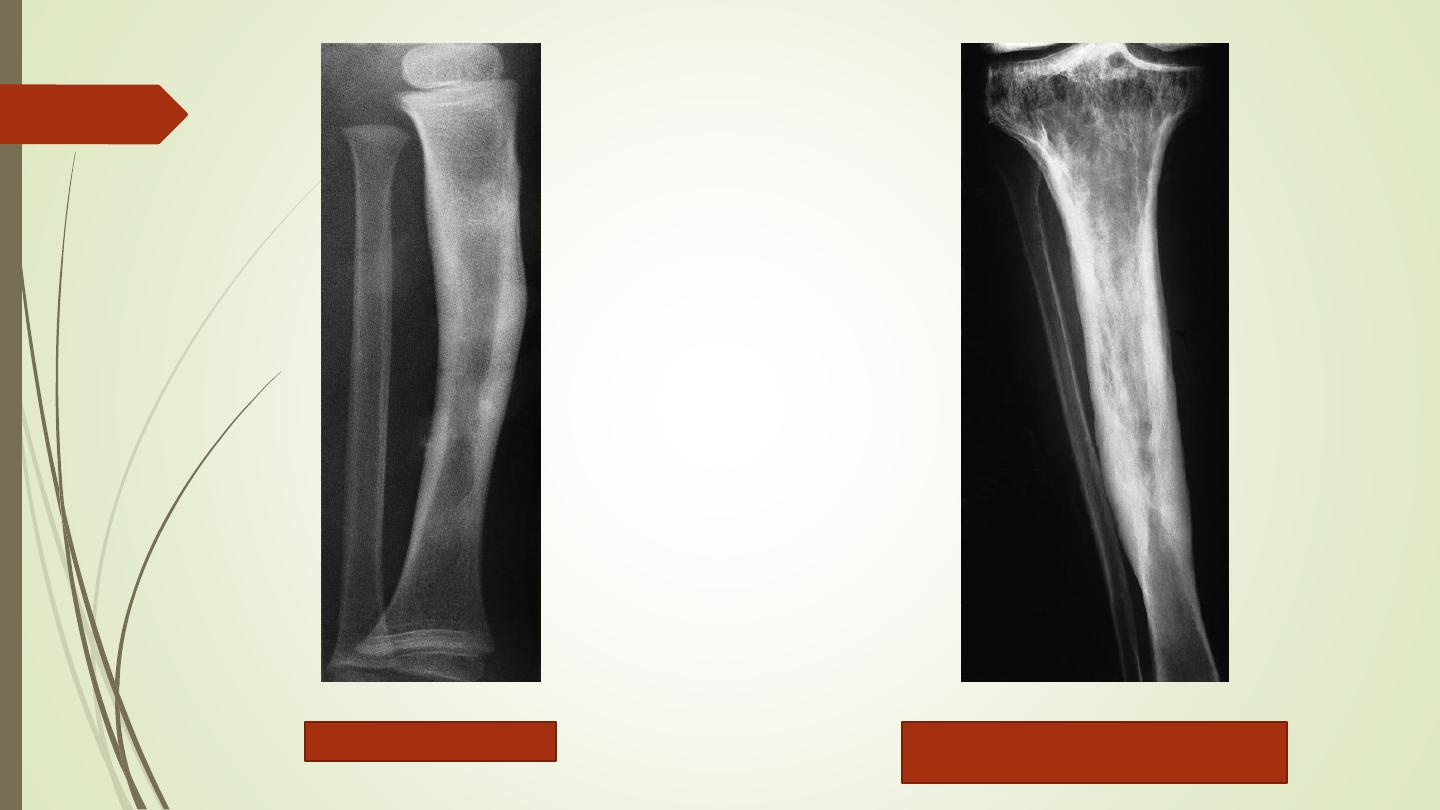
Generalized alteration of bone density
Osteoporosis
Normal
Osteopetrosis
Focal alteration of bone density
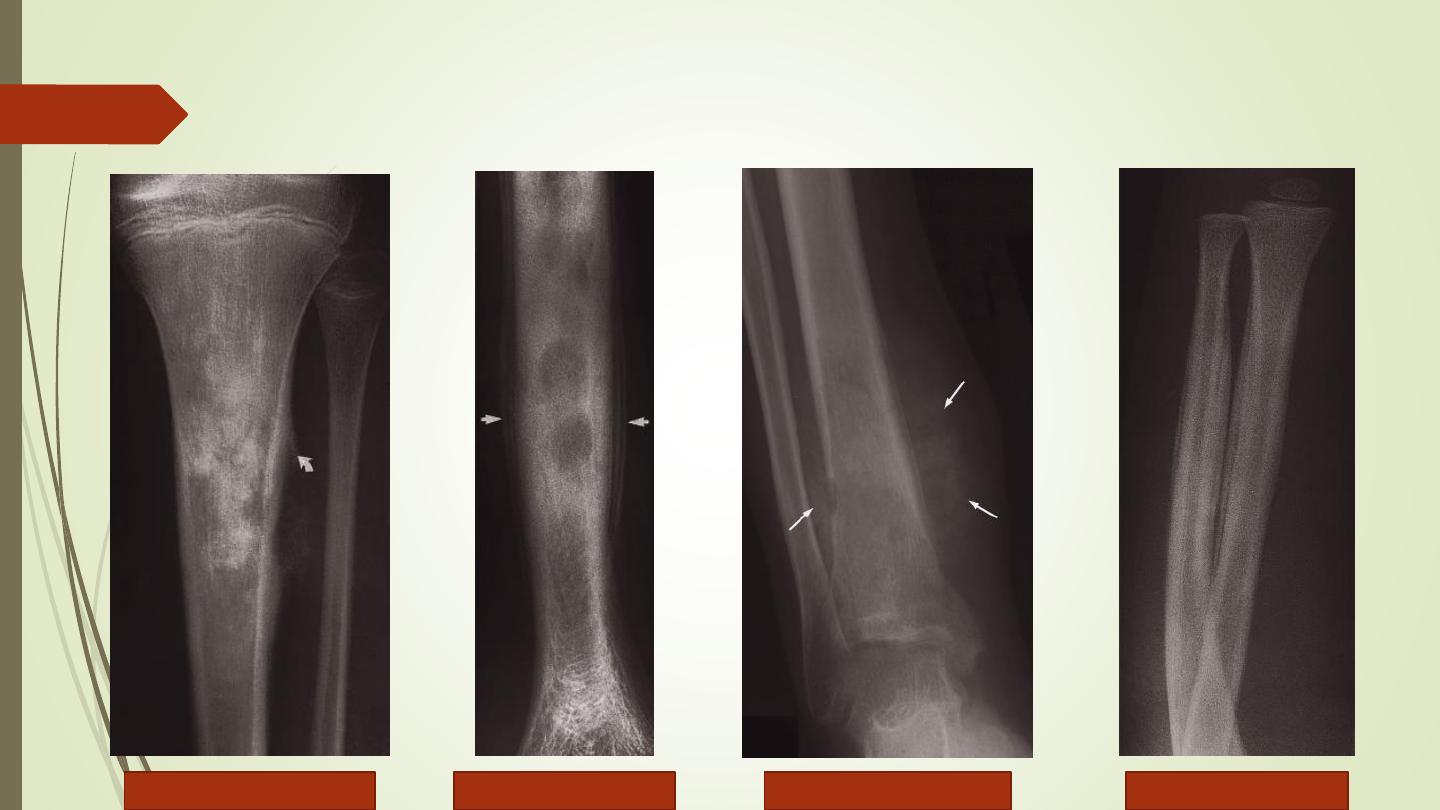
Periosteal reaction
Codman’s triangle
Smooth lamellar
Spiculated
(sunray
Onion skin
Cortical thickening
Alteration of trabecular
pattern in Paget’s disease
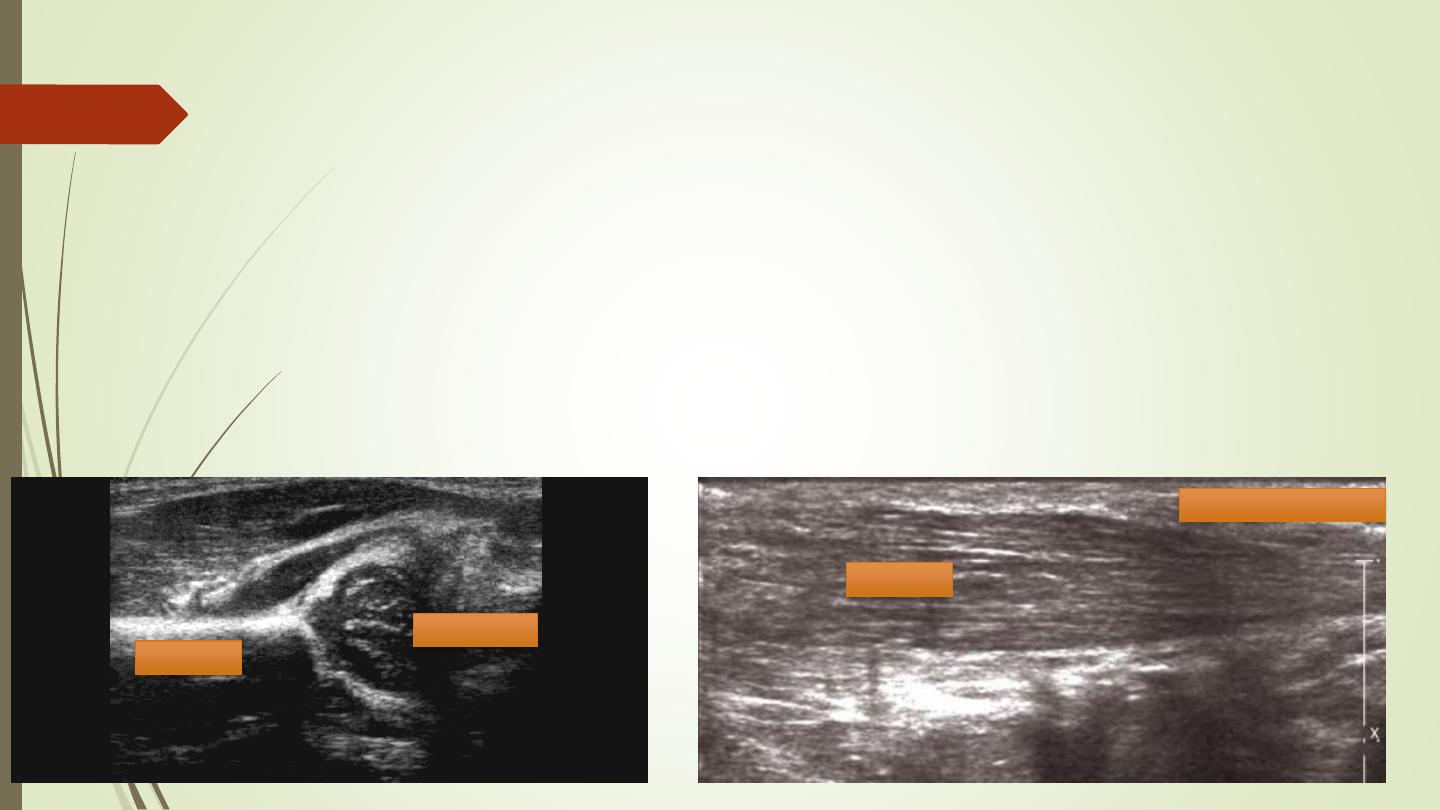
Ultrasonography:
Ultrasound cannot demonstrate bone pathology
Detecting tenosynovitis, tendon tears and rupture
Diagnosis of DDH in infants.
Diagnosis of osteomyelitis.
Soft tissue lesions or calcification
Muscle
Subcutaneous fat
Cartilage
Bone
Computed tomography
Demonstrating abnormalities in the spine, pelvis and
Hips. Three-dimensional reconstructions can be made
Demonstrating the extent and characterization of bone
lesion
As a guide for bone biopsy.
❖
Advantages:
❖
Disadvantages:
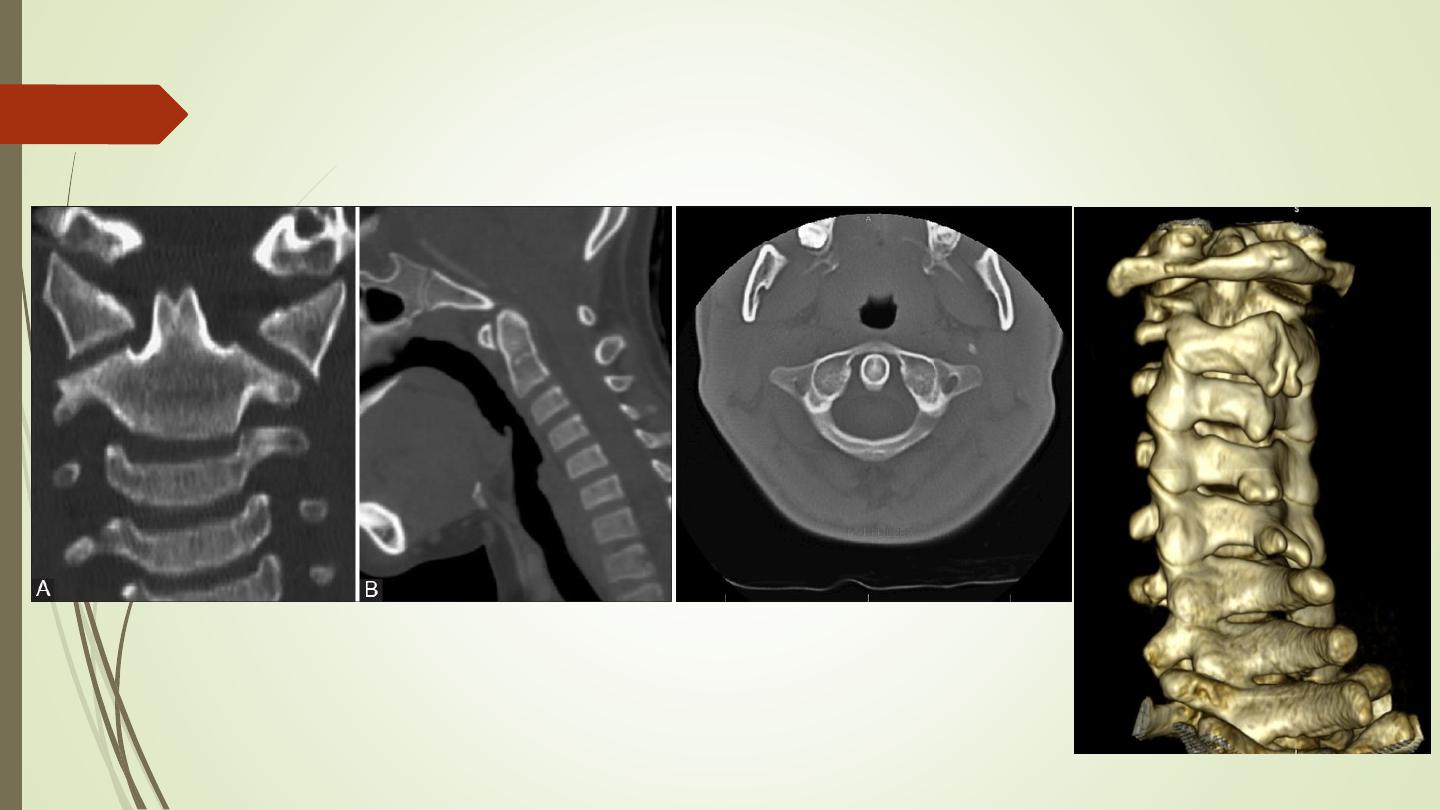
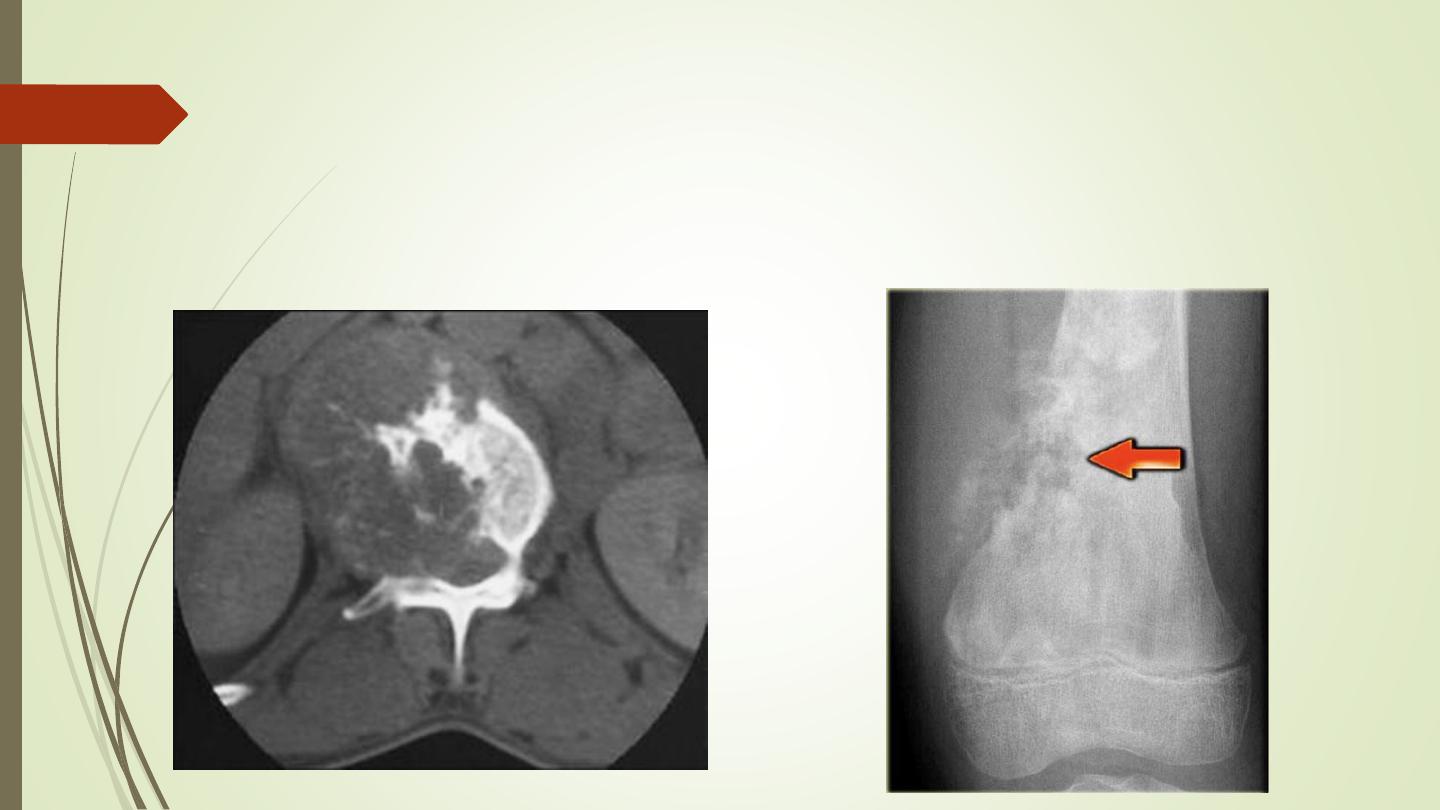
Computed tomography

CT scan of pelvis showing a large mass (arrows) due to a metastasis destroying
the medial half of the right iliac bone with extension into the adjacent soft
tissues
Magnetic resonance imaging
Calcified tissues such as bone produce no signal with MRI, but
MRI can demonstrate the bone marrow directly
The major indications for musculoskeletal MRI are:
To demonstrate disc herniation and spinal cord or nerve root
compression
To diagnose bone metastases
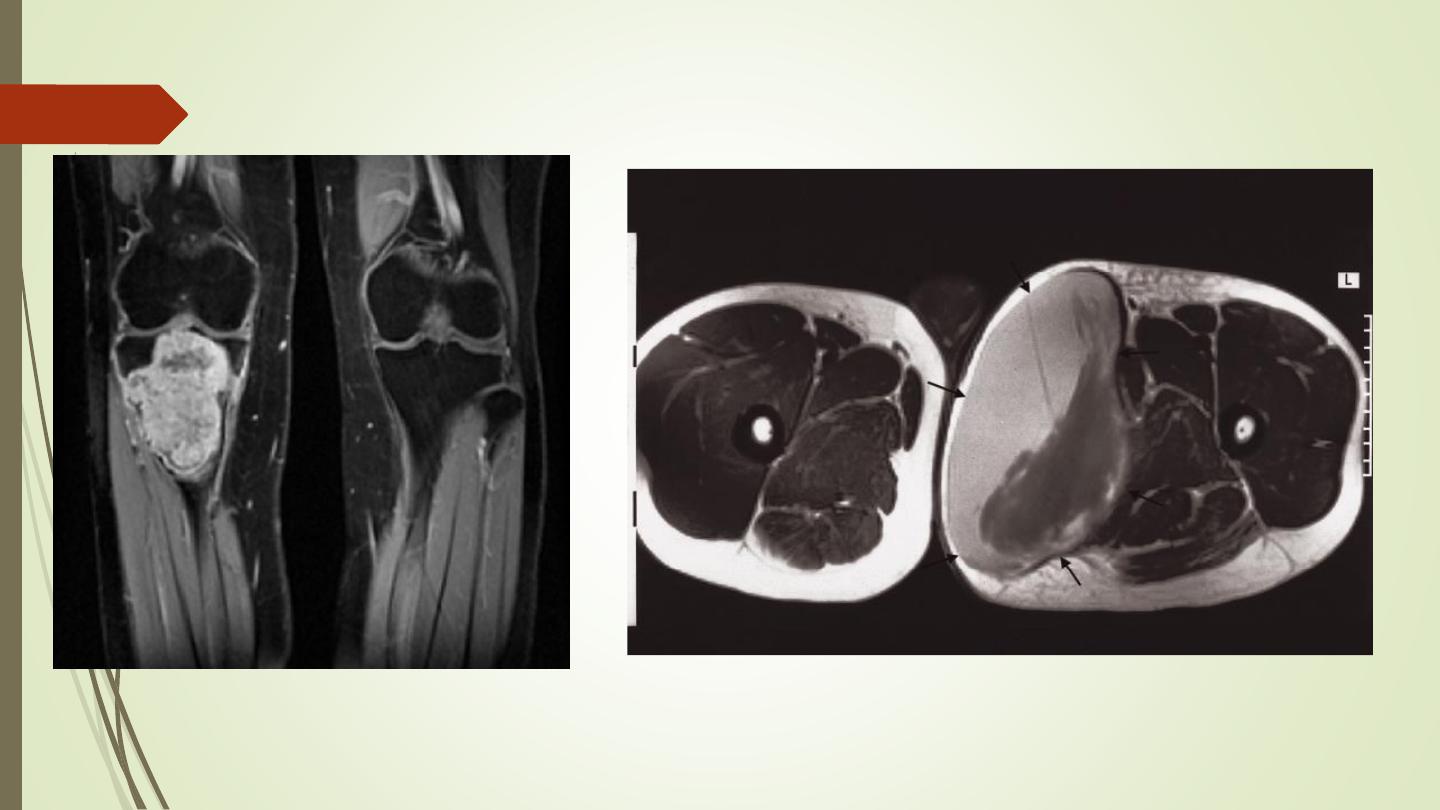
To show the extent of primary bone tumors
To image soft tissue masses
To diagnose osteomyelitis and show any soft tissue abscess
To diagnose avascular necrosis and other joint pathologies and
to image both acute and chronic injury to joint cartilages,
ligaments and other intra-articular soft tissues
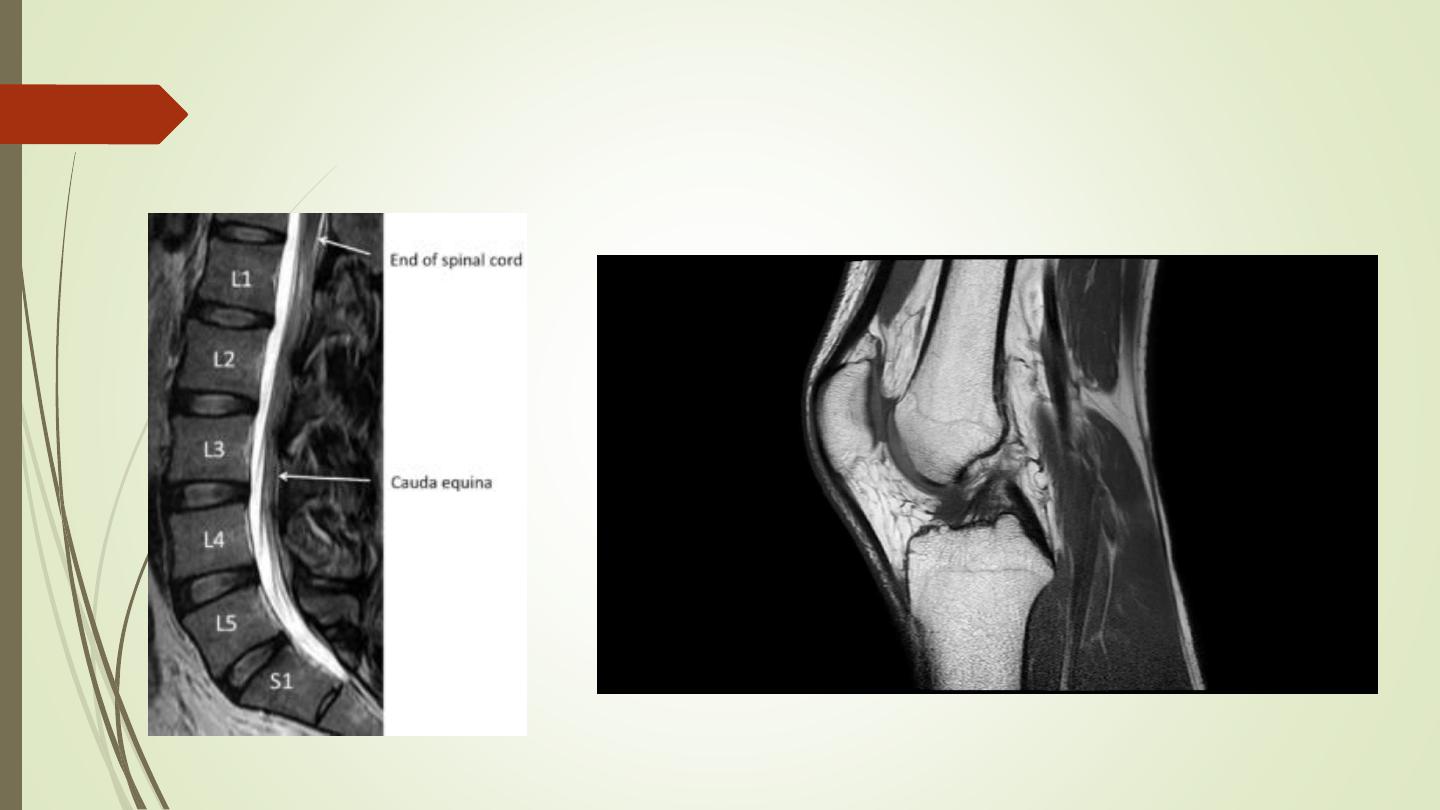
Magnetic resonance imaging
Radionuclide bone scanning
Using Technetium-99m (99mTc)-labelled phosphate
complexes given as an intravenous injection. They are taken
up selectively by the bones and excreted in the urine.
Indications for radionuclide bone scanning are:
Detection of metastases
Detection of osteomyelitis.
Determination of whether a lesion is solitary or multifocal
Investigation of a clinically suspected bone lesion despite a normal
radiograph osteomyelitis
Determination, in equivocal cases, of whether an abnormality seen on
the radiograph is significant or not
Investigation of painful joint prostheses.

Radionuclide bone
scanning
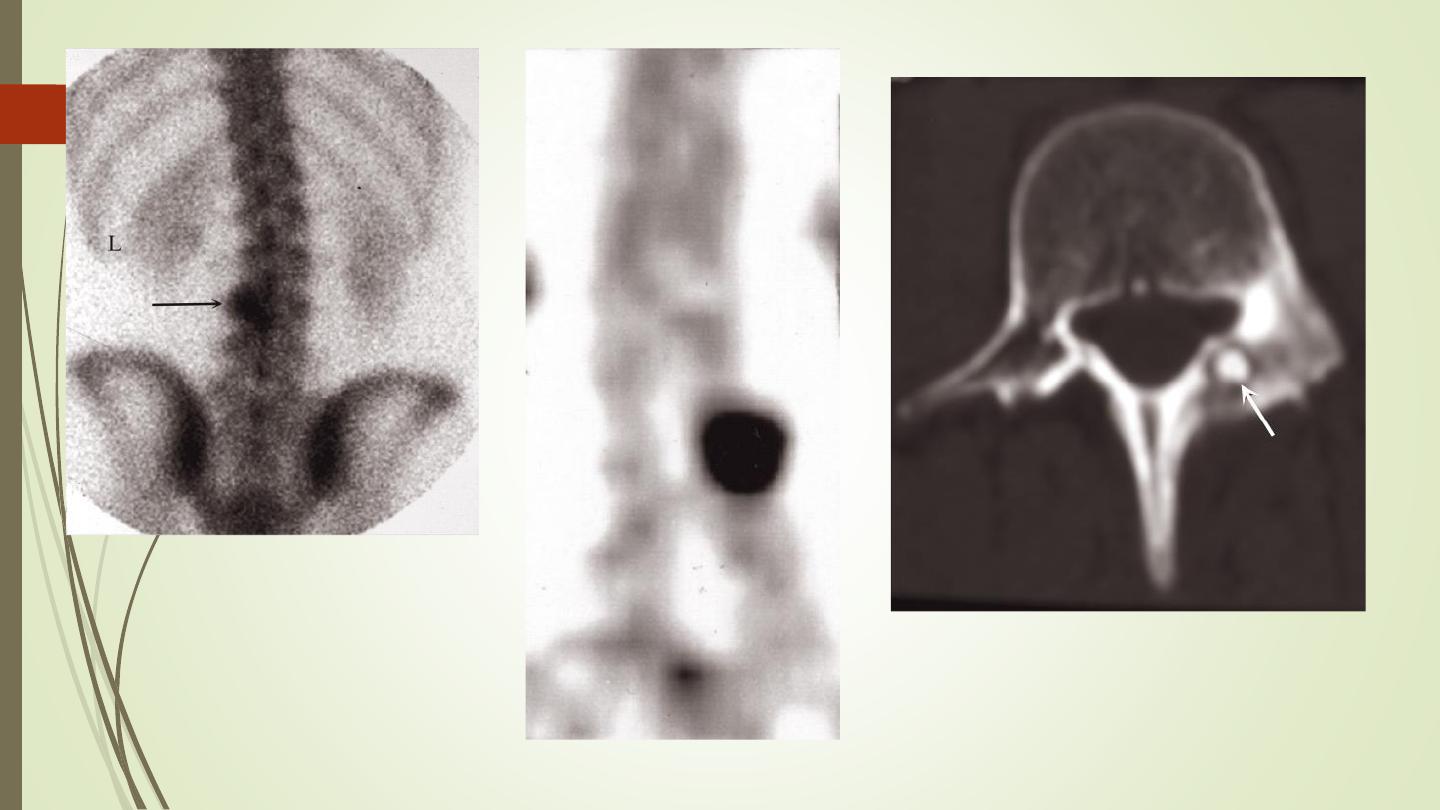
Osteoid osteoma
• Bone scan (posterior view) showing a focal area
of intense increased uptake in L3
• CT demonstrates the tumor arising in the
pedicle.
II) Bone pathology:
Solitary lytic or sclerotic lesions
Multiple focal lesions, i.e. several discrete lytic or
sclerotic lesions in one or more bones
Generalized increase or decrease in bone density
Alteration of the trabecular pattern or change its
shape
Solitary bone lesion
➢
Lytic
➢
Sclerotic
➢
Mixed
o
bone tumors (a) malignant (primary or secondary) (b) benign
o
osteomyelitis
o
bone cysts, fibrous dysplasia or other non-neoplastic defects
of bone
o
conditions of uncertain nature such as Langerhans histiocytosis
and osteoid osteoma
How to determine the nature of the lesion?
Age of the patient
Site of the lesion
Zone of transition
The adjacent cortex
Expansion
Periosteal reaction
Calcific densities within the lesion
Soft tissue swelling
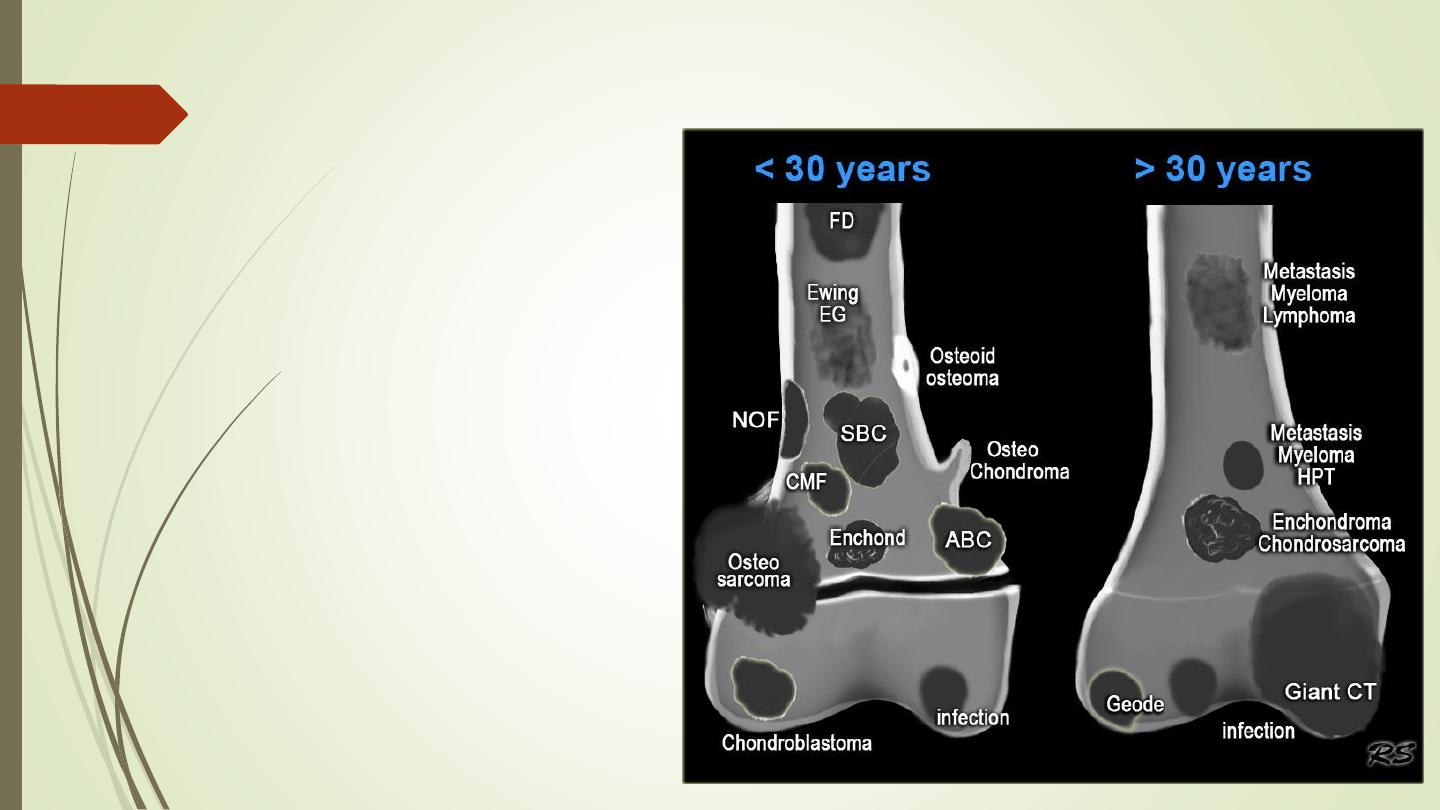
1- Age of the patient
2- Site of the lesion
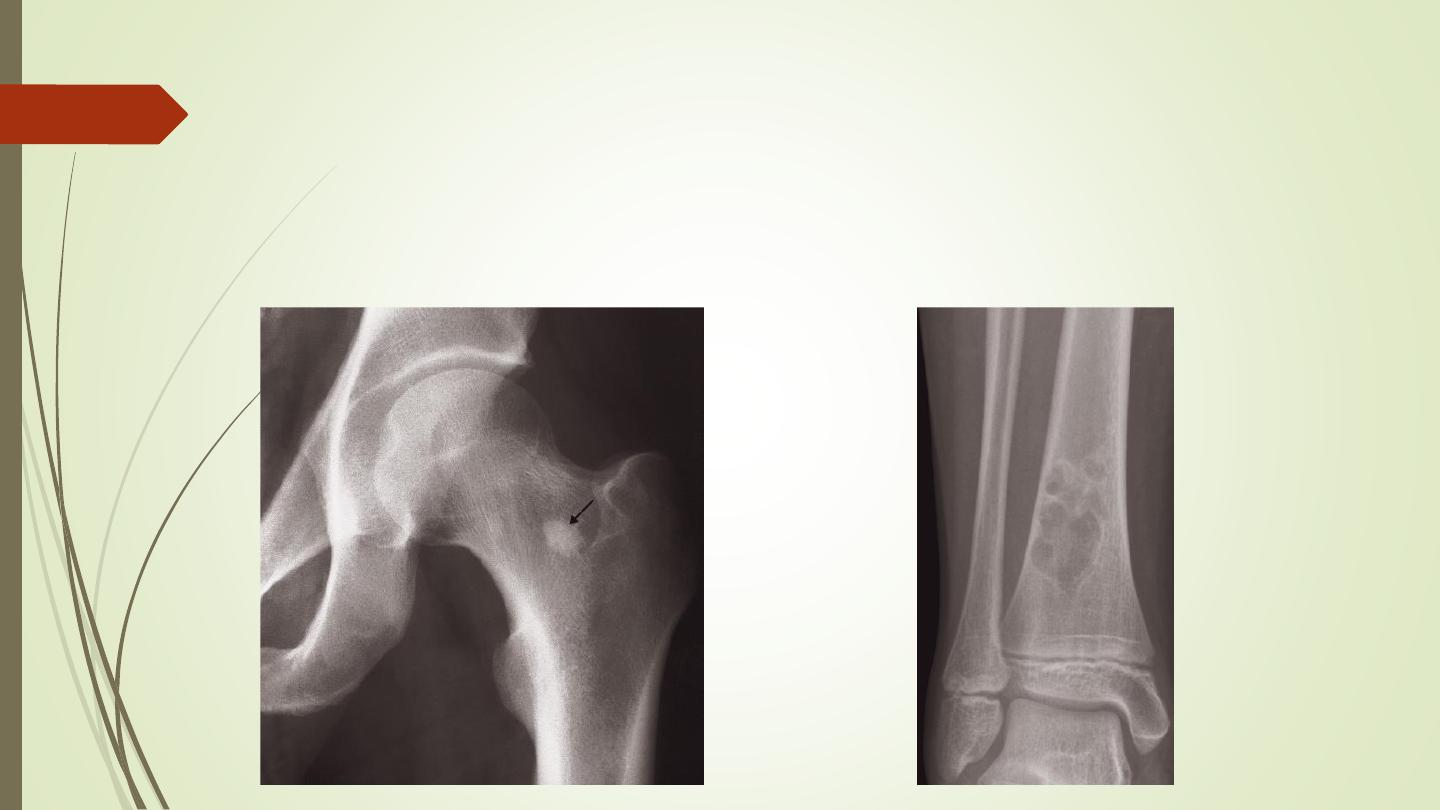
3- Zone of transition
❖
A lesion with a well-defined sclerotic edge is almost certainly benign,
e.g. a fibrous cortical defect or a bone island
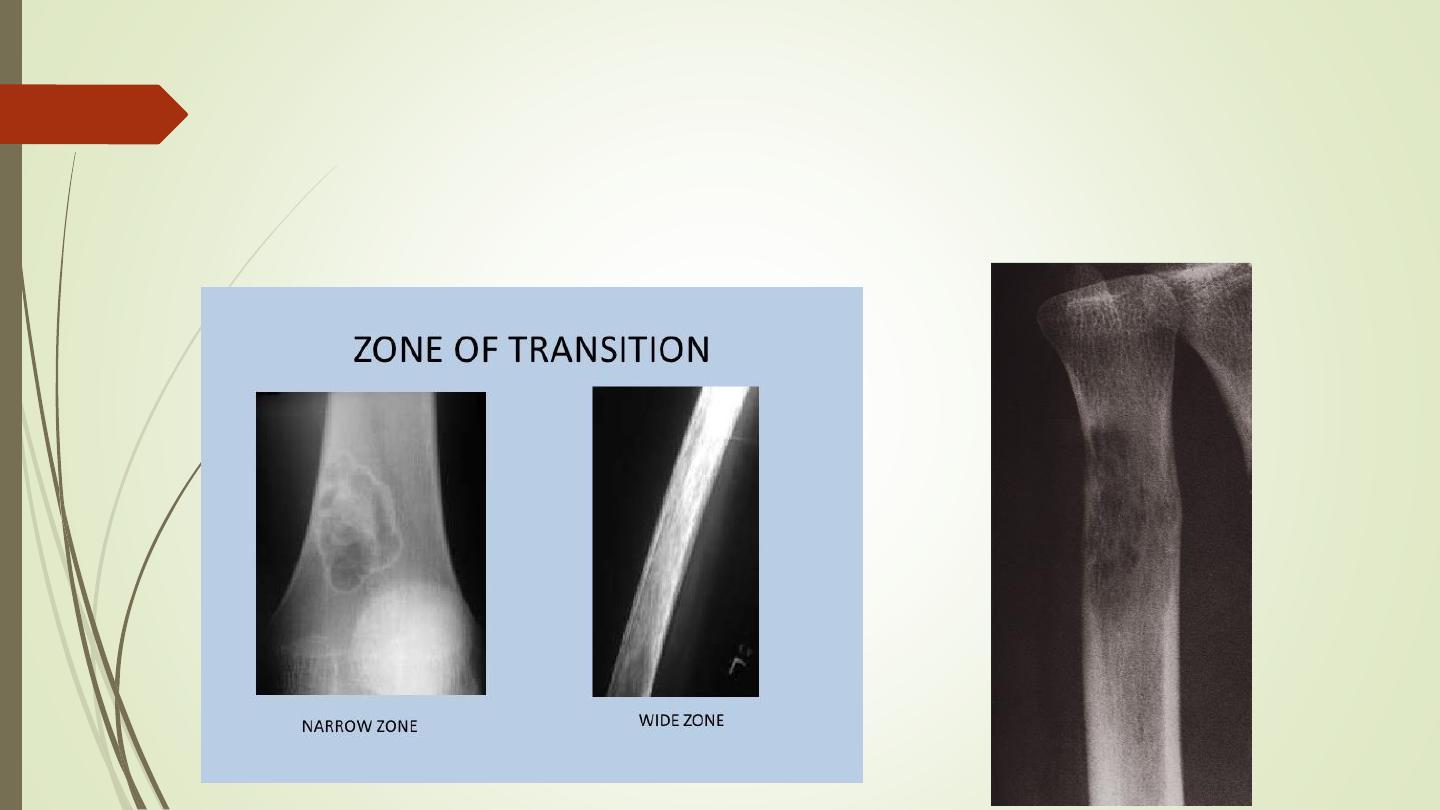
3- Zone of transition
❖
A lytic area with an ill-defined edge is likely to be aggressive. E.g.
malignant tumor and infection
3- Zone of transition
❖
A lytic area with no sclerotic rim,
which may be a benign or
malignant lesion. E.g. metastases
and myeloma
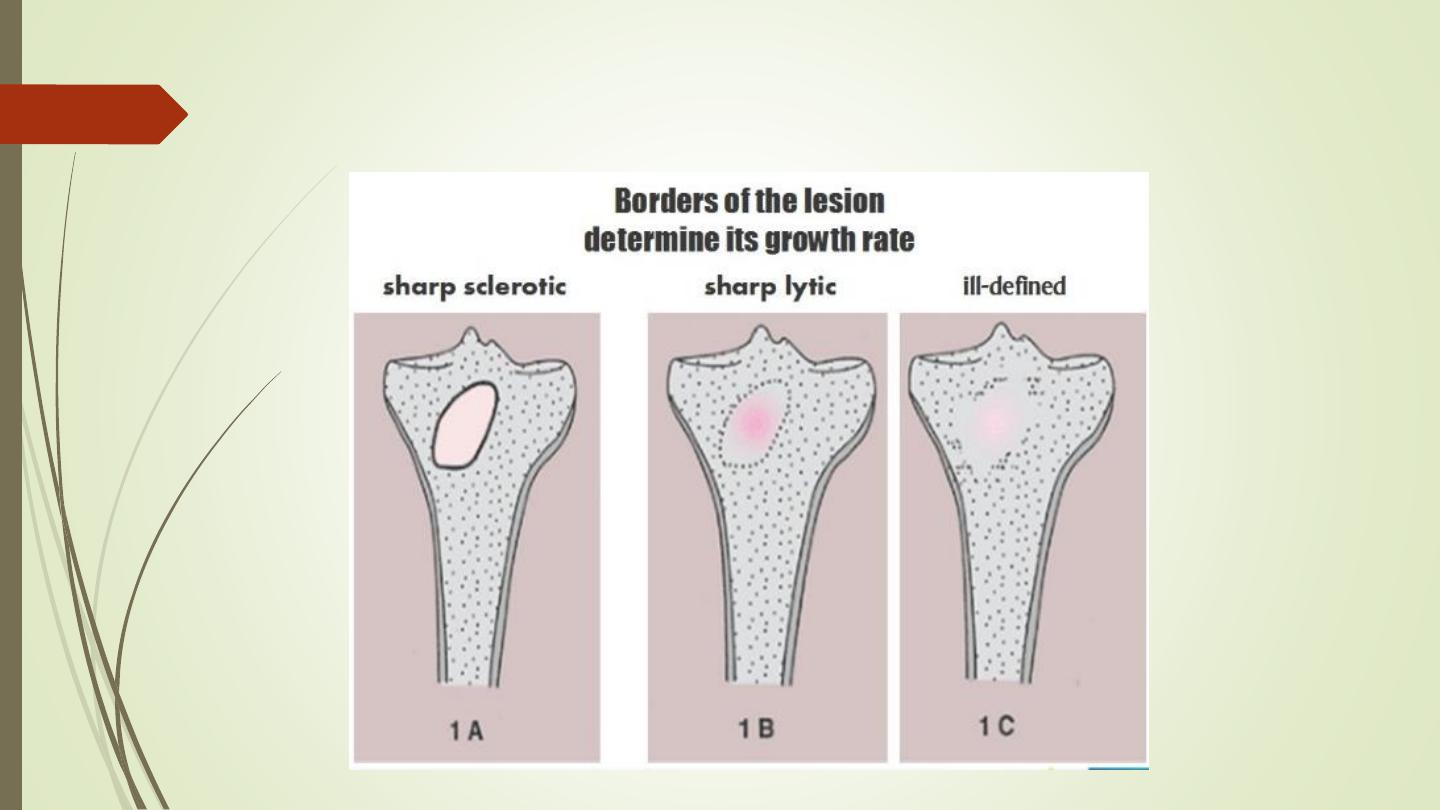
3- Zone of transition
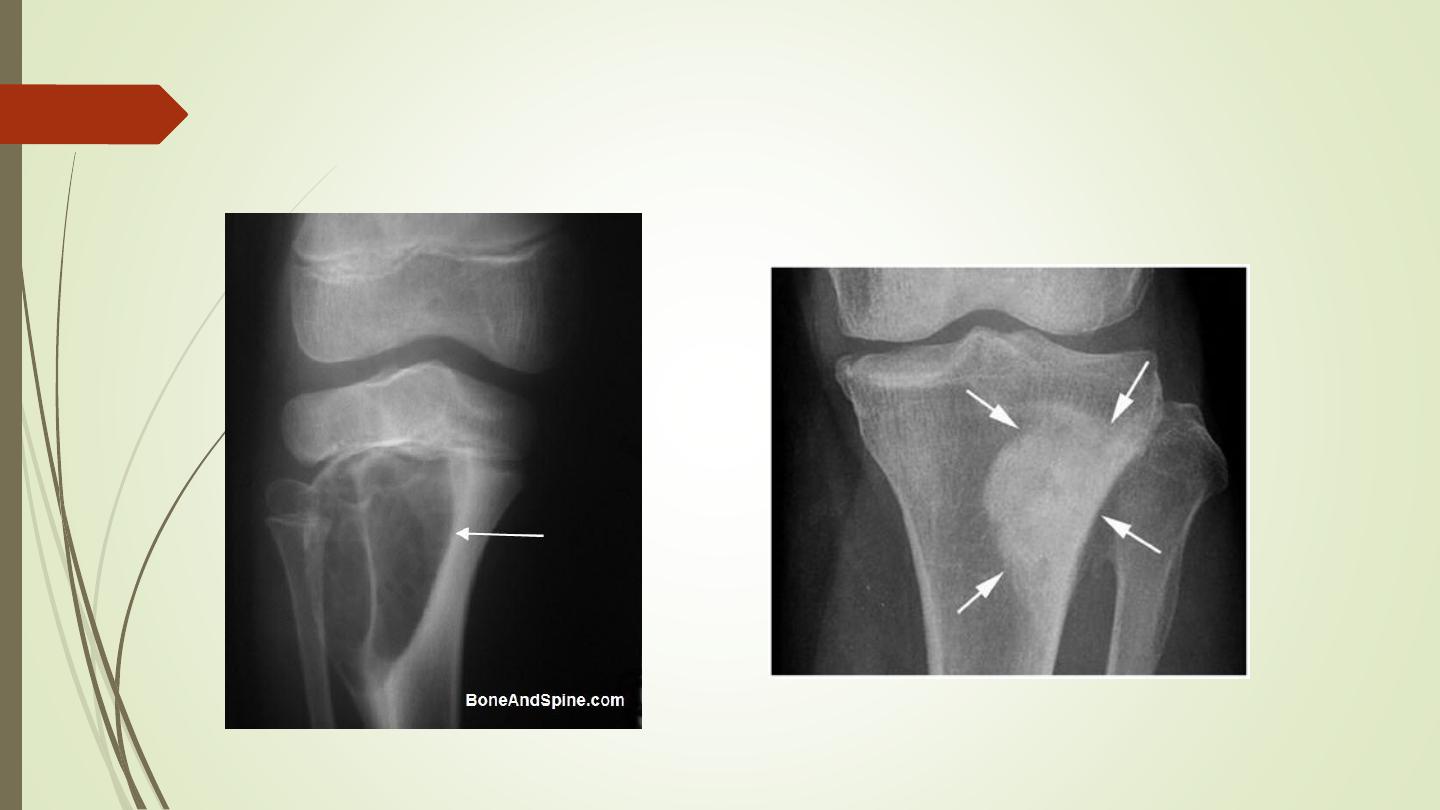
4- The adjacent cortex
Any destruction of the adjacent cortex indicates an aggressive lesion
such as a malignant tumor or osteomyelitis.

5- Expansion
Bone expansion with an intact well-formed cortex usually indicates a
slow-growing lesion such as an enchondroma or fibrous dysplasia
6- Periosteal reaction
The causes of localized periosteal reactions adjacent to a
lytic or sclerotic lesion are:
❖
Osteomyelitis
❖
Trauma
❖
Malignant bone tumor, particularly Ewing’s sarcoma and
osteosarcoma
❖
occasionally metastasis, particularly neuroblastoma
❖
Langerhans histiocytosis.
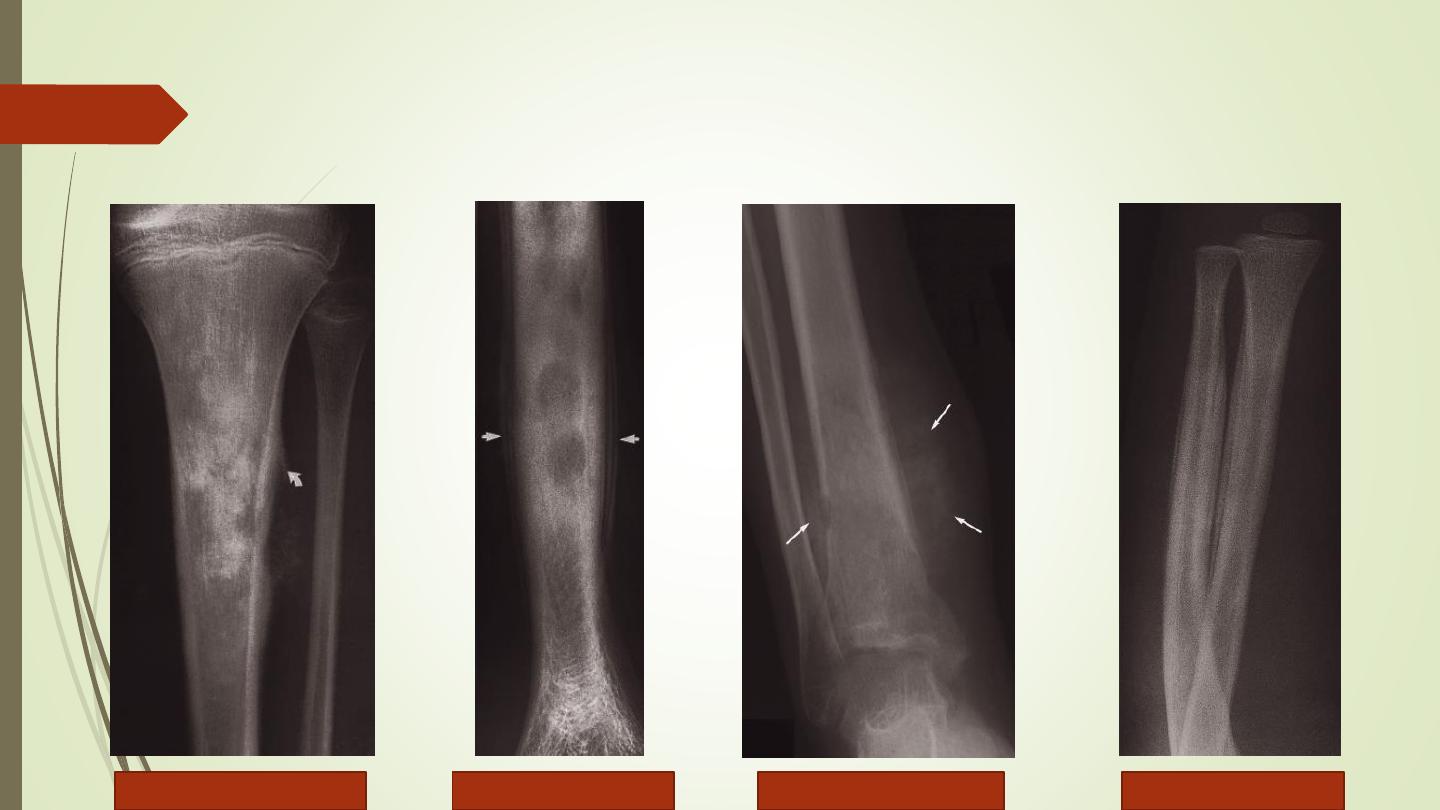
Codman’s triangle
Smooth lamellar
Spiculated
(sunray
Onion skin
6- Periosteal reaction
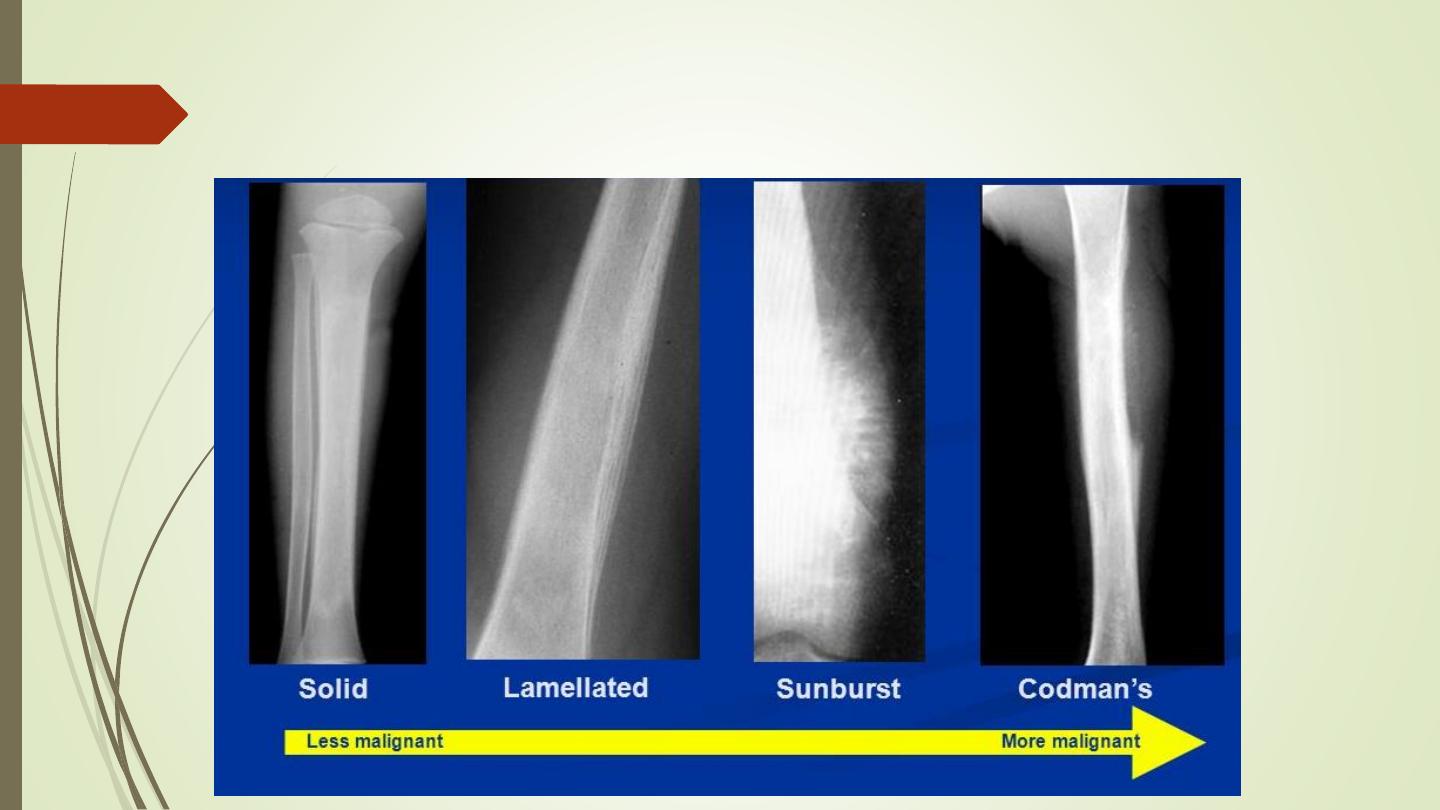
6- Periosteal reaction
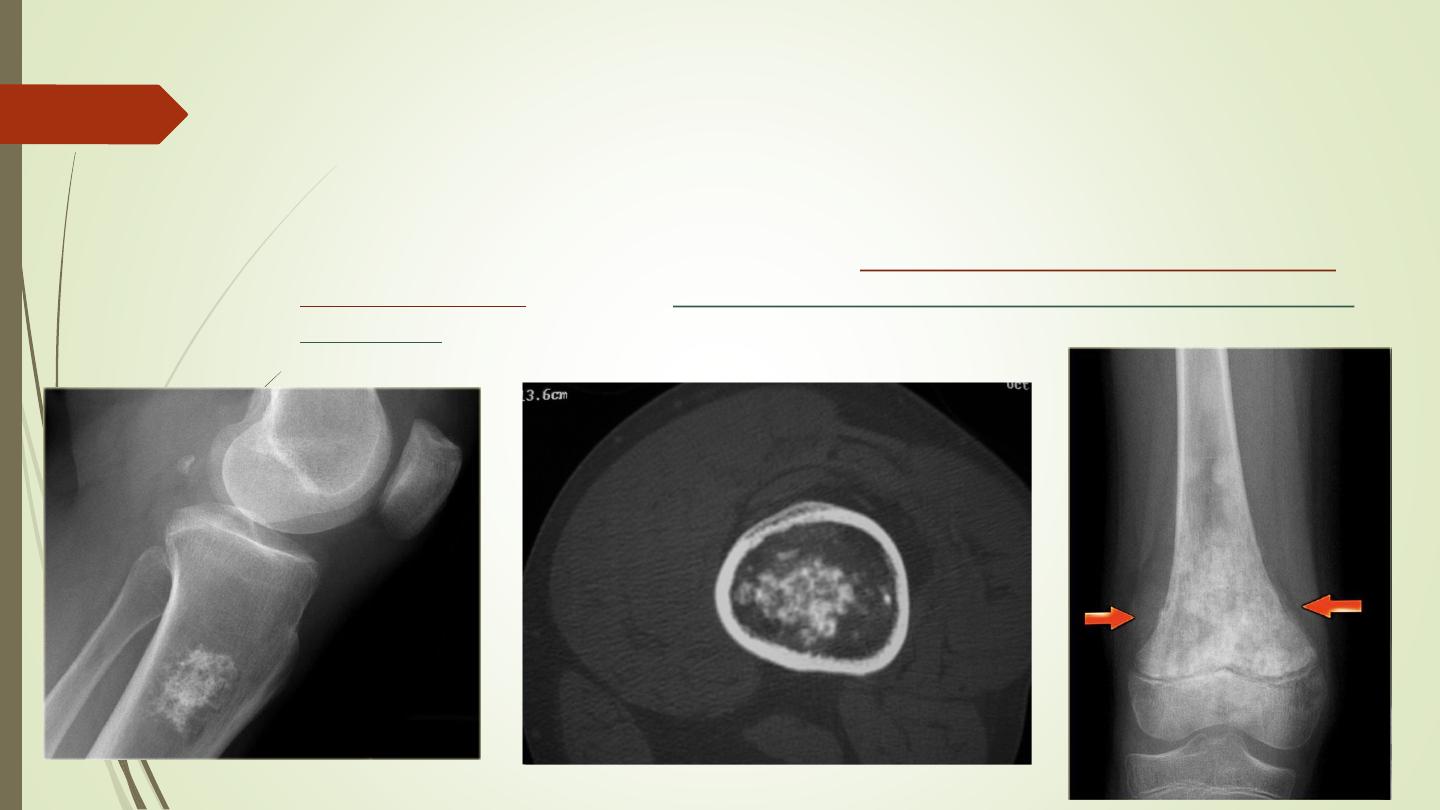
7- Calcific densities within the lesion
Calcification within an area of bone destruction occurs in specific conditions;
for example, patchy calcification of a
popcorn type usually indicates a
cartilage tumor
, whereas
diffuse ill-defined calcification suggests osteoid
formation
and indicates an osteosarcoma
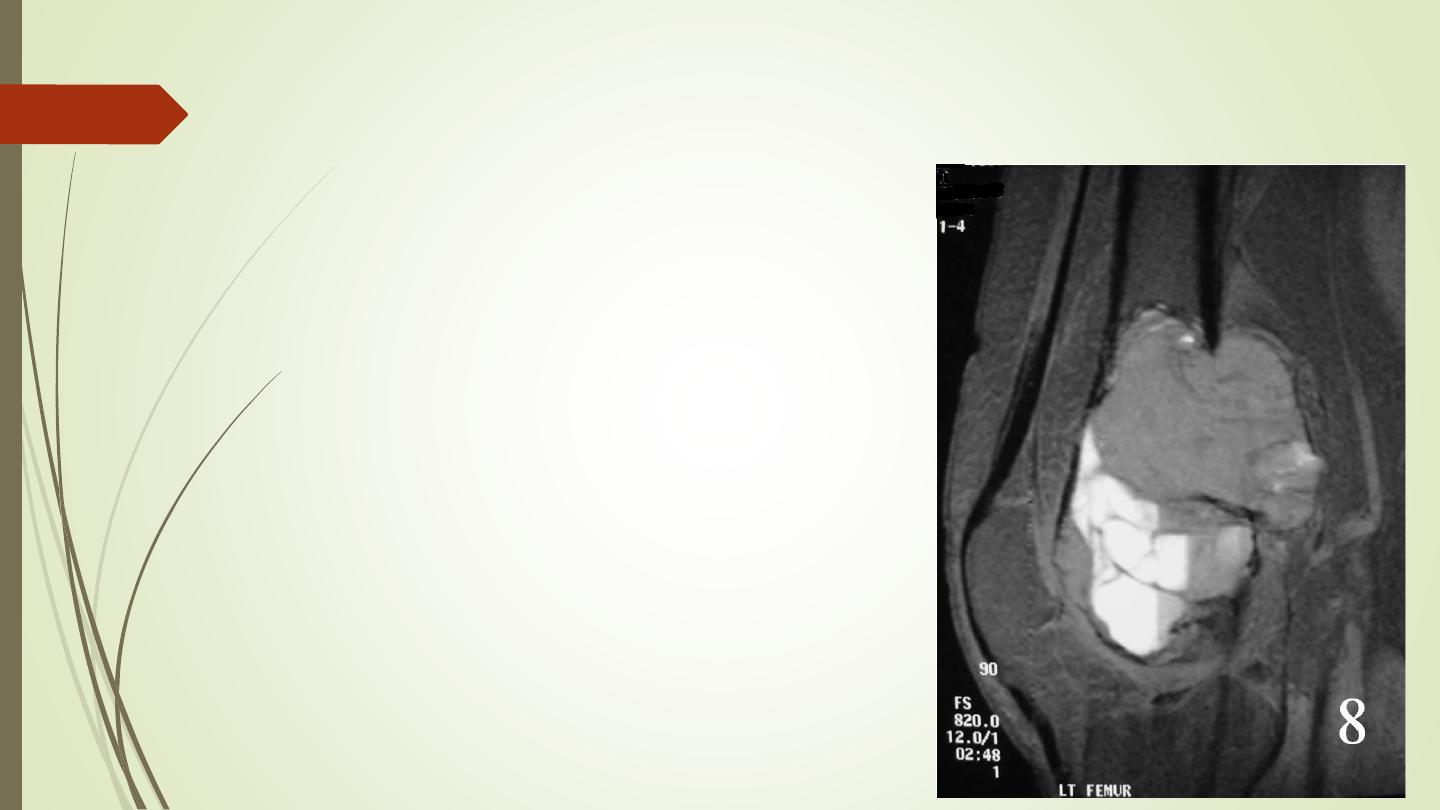
8- Soft tissue swelling
The presence of a soft tissue mass
suggests an aggressive lesion

Thank you
