
Congenital Heart Disease
Scope
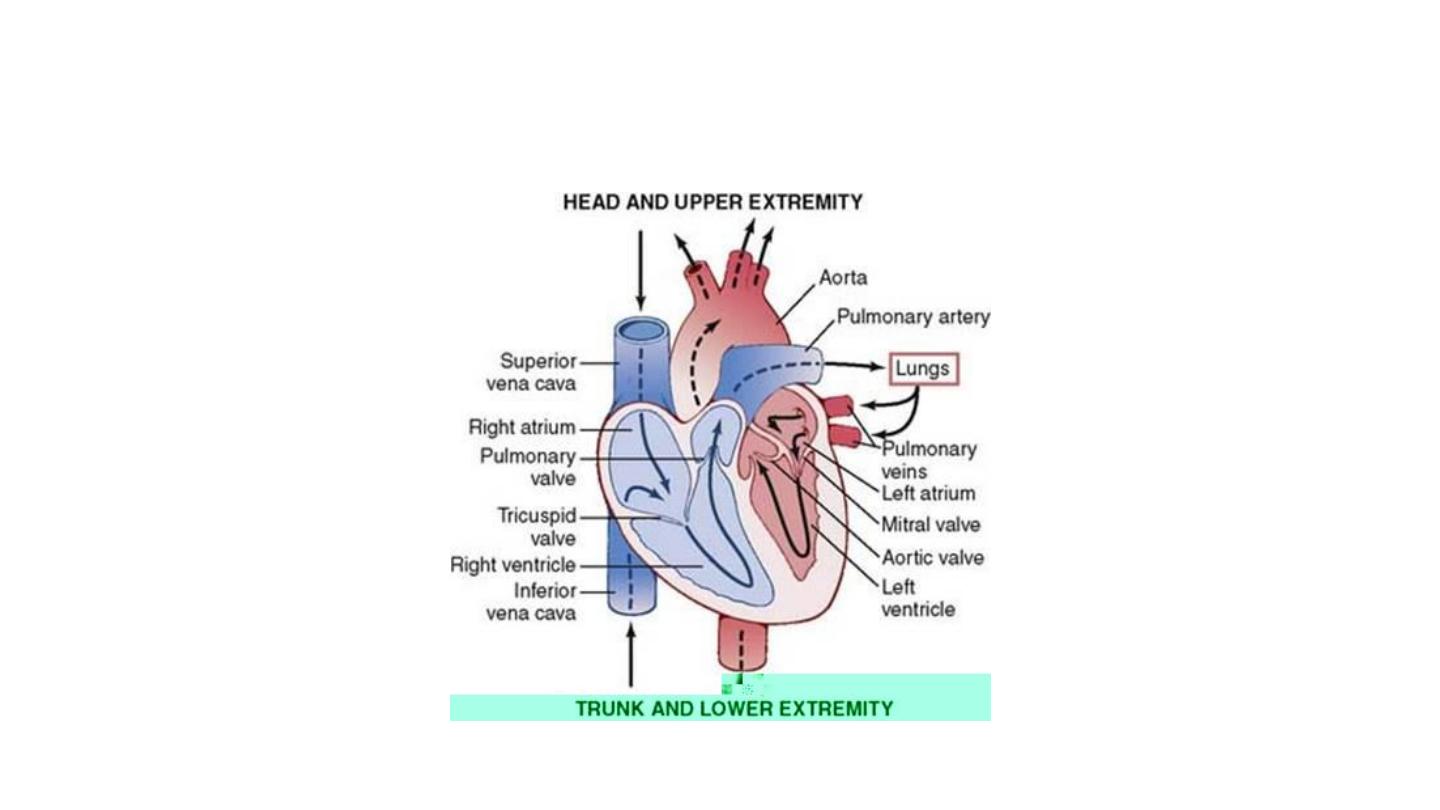
• Fetal circulation Vs mature circulation
• Development of pulmonary HT in CHD
• CHD with shunts: ASD, VSD, PDA
• CHD without shunts: congenital PS,
Co-A
• Cyanotic CHD: TOF
2

Objectives
• CHD can manifest for the first time in adulthood
• CHDs with shunt have similar clinical presentations
• PHT & Eisenmenger’s syndrome may complicate all
conditions with increased pulmonary blood flow
(including shunt lesions) if untreated
3

Objectives
• Initially, PHT develops due to increased flow & is
usually reversible; later due to increased pulmonary
vascular resistance & is irreversible
• Recognition depends on the underlying anatomical
defect and its hemodynamic consequences
4
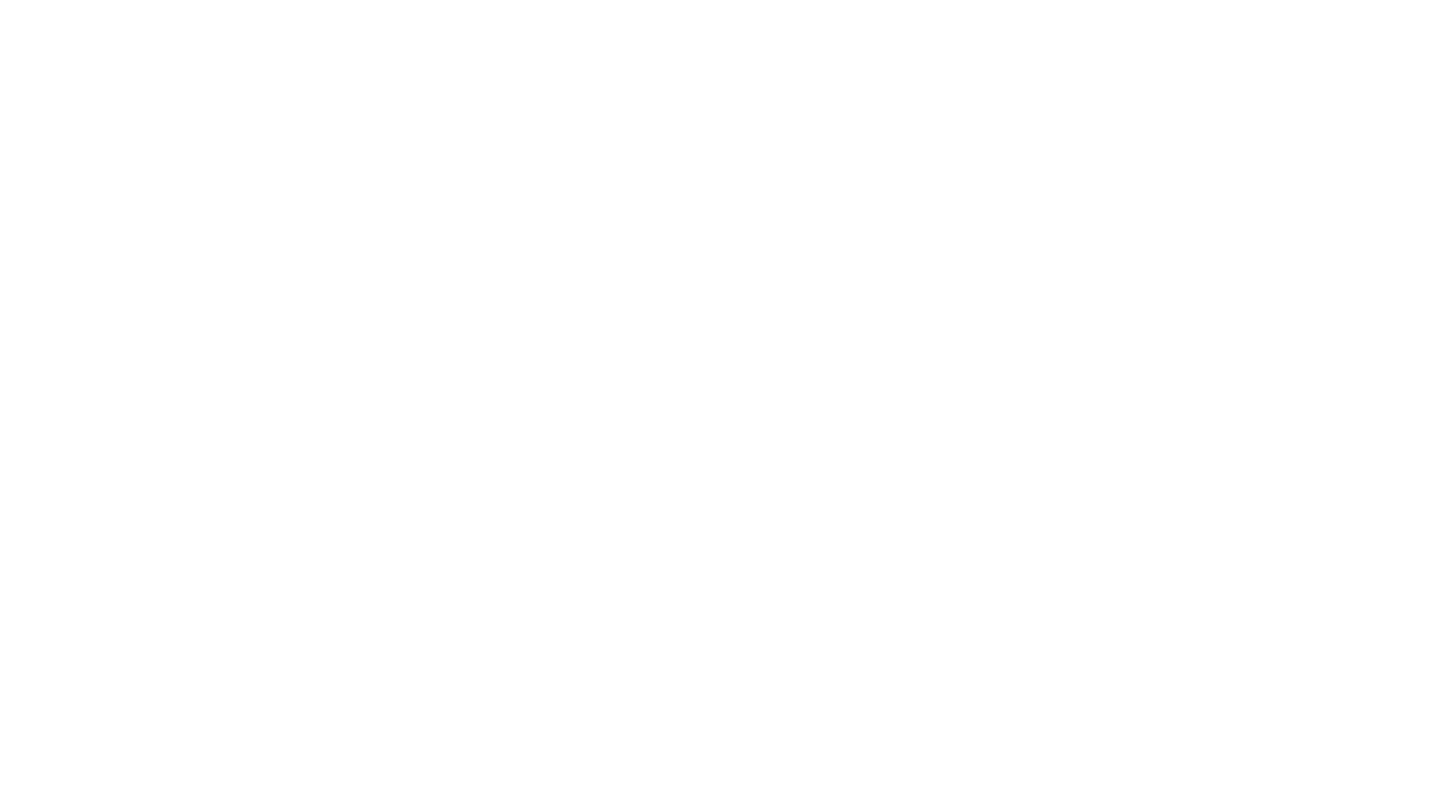
The Normal Circulation
5
6

Congenital Heart Disease:
Classification
• Acyanotic:
– With shunt: e.g. ASD, VSD, PDA
– Without shunt: e.g. PS, coarctation of
the aorta, congenital AS, congenital
MS……
• Cyanotic
– With reduced pulmonary blood flow: e.g.
TOF
– With increased blood flow: TGA
7

Common Congenital Heart Disease
• Atrial septal defect (ASD)
– Osteum secundum
– Osteum primum
• Ventricular septal defect (VSD)
• Patent ductus arteriosus (PDA)
• Coarctation of the aorta
• Congenital pulmonary stenosis
• Tetralogy of Fallot (TOF)
8

Clinical Presentation of CHD
• Asymptomatic
• Congestive heart failure
• Cyanosis and digital clubbing
• Failure to thrive
• Recurrent chest infections
9

Clinical Presentation of CHD
• Heart murmur
• Pulmonary hypertension with reversed shunt
(Eisenmenger syndrome)
10

Pulmonary Hypertension
• Initially caused by increased blood flow through the
pulmonary vessels due to left-to-right shunt
• Usually reversible on correction of the defect
11

Pulmonary Hypertension
• Later on: structural changes affect the walls of
pulmonary arterioles, including:
– Arterial wall thickening
– intraluminal thrombosis
– Capillary obliteration
• Probably irreversible!
12

Pulmonary Hypertension
These structural changes leads to:
• increased resistance to pulmonary blood flow
• Reduction of pulmonary blood flow
• Right-to-left shunt through the connection between
the two circulations (reversed shunt, the
Eisenmenger’s syndrome)
13

Eisenmenger
’s Syndrome:
clinical features
• Cyanosis and clubbing
• Raised JVP
• Left parasternal heave (RVH)
• Systolic expansion of the pulmonary
artery
• Palpable second heart sound
• Loud pulmonary second sound
14

Eisenmenger
’s Syndrome:
clinical features
• RV third heart sound
• Murmurs:
– early diastolic murmur at the pulmonary
area (Graham-Steel murmur)
– Tricuspid regurgitation (pansystolic
murmur at LSB)
15

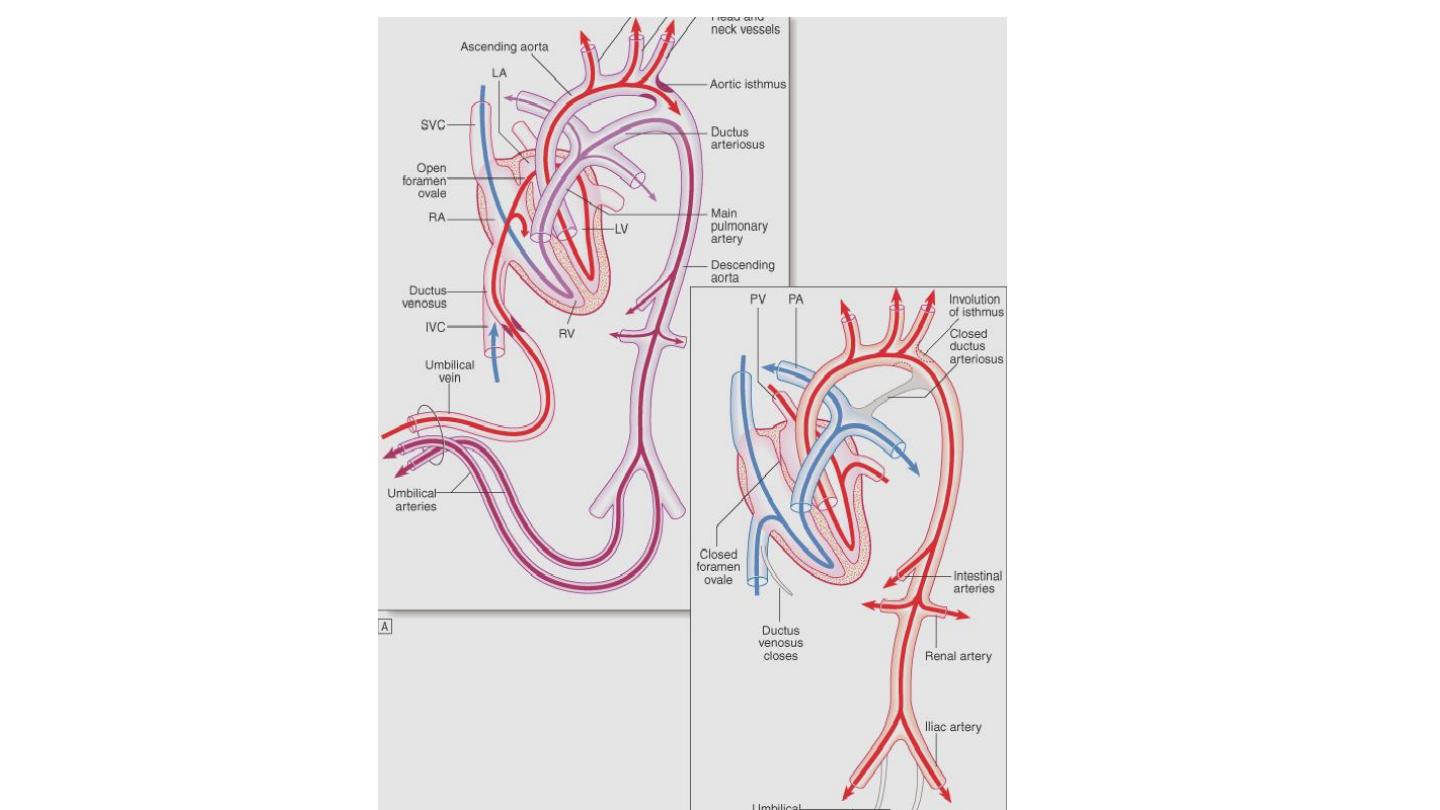
Eisenmenger
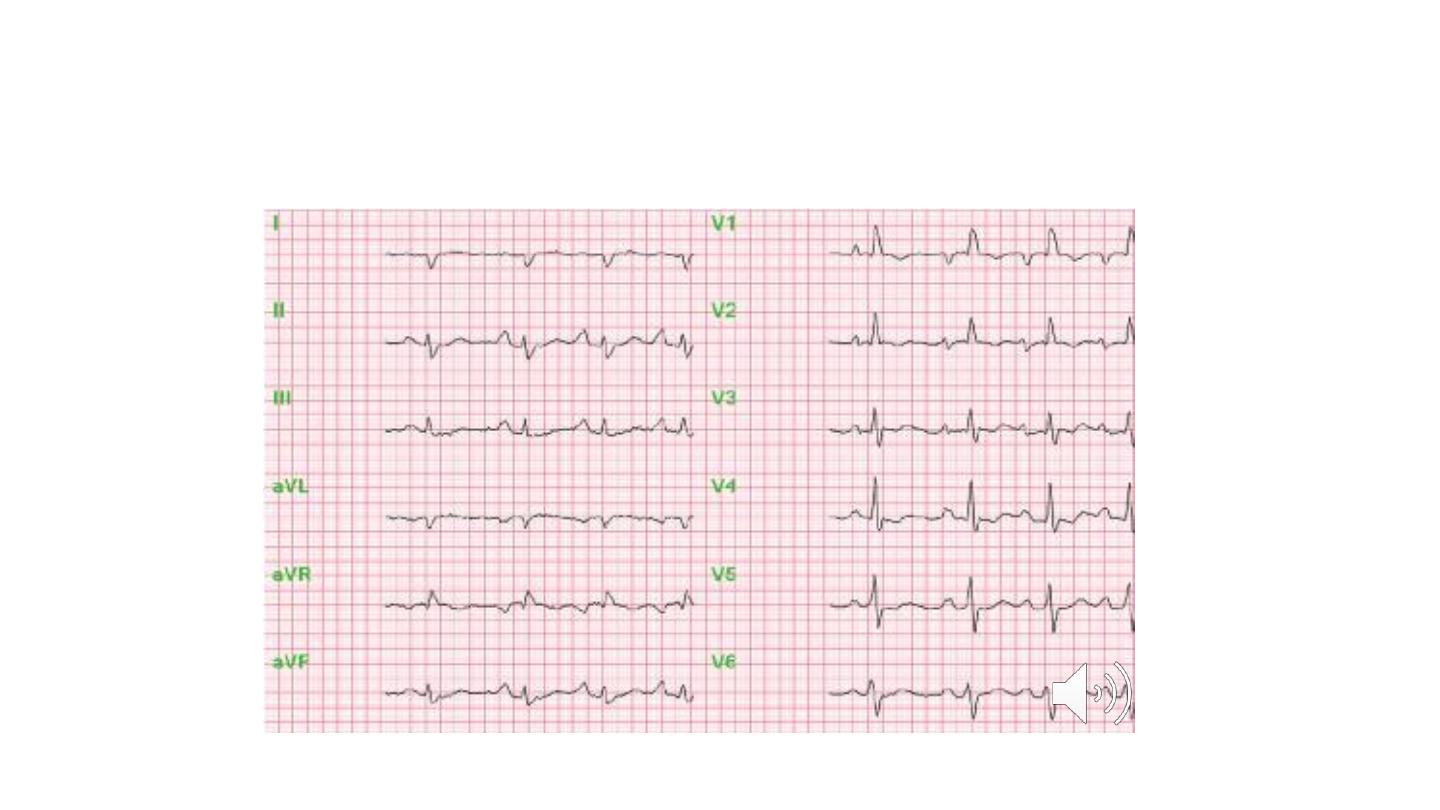
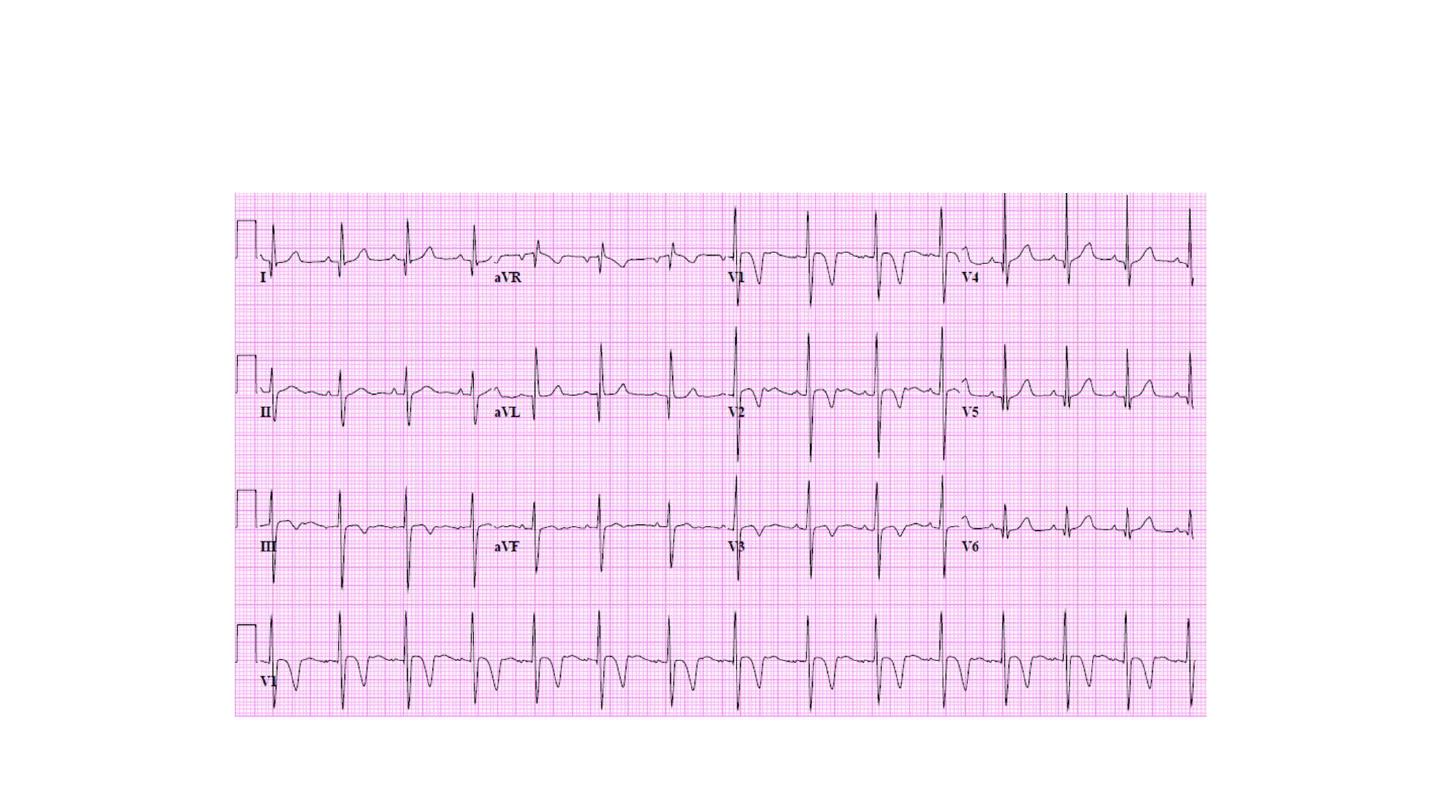
’s Syndrome: ECG
• Right axis deviation
• Right ventricular hypertrophy (tall R
waves in V1& V2)
• Peaked P wave (RA enlargement)
16
ECG in Eisenmenger
’s Synd.
17
ECG in Eisenmenger
’s Synd.
18

CXR in Eisenmenger
’s Synd.
• CXR shows enlarged central pulmonary arteries &
peripheral pruning of the pulmonary arteries
19

CXR in Eisenmenger
’s Synd.
20
Complications of
Cyanotic
Heart
Disease
• Polycythemia: hyperviscosity syndrome
• Hemoptysis, sometimes massive and
fatal
• Paradoxical embolization
• Brain abscess
21

Specific Congenital Heart
Diseases
22

Atrial Septal Defect (ASD)
• Osteum primum ASD:
– part of endocardial cushion defects
– associated with mitral regurgitation and tricuspid
regurgitation
• Osteum secundum ASD: at the area of fossa ovalis
23
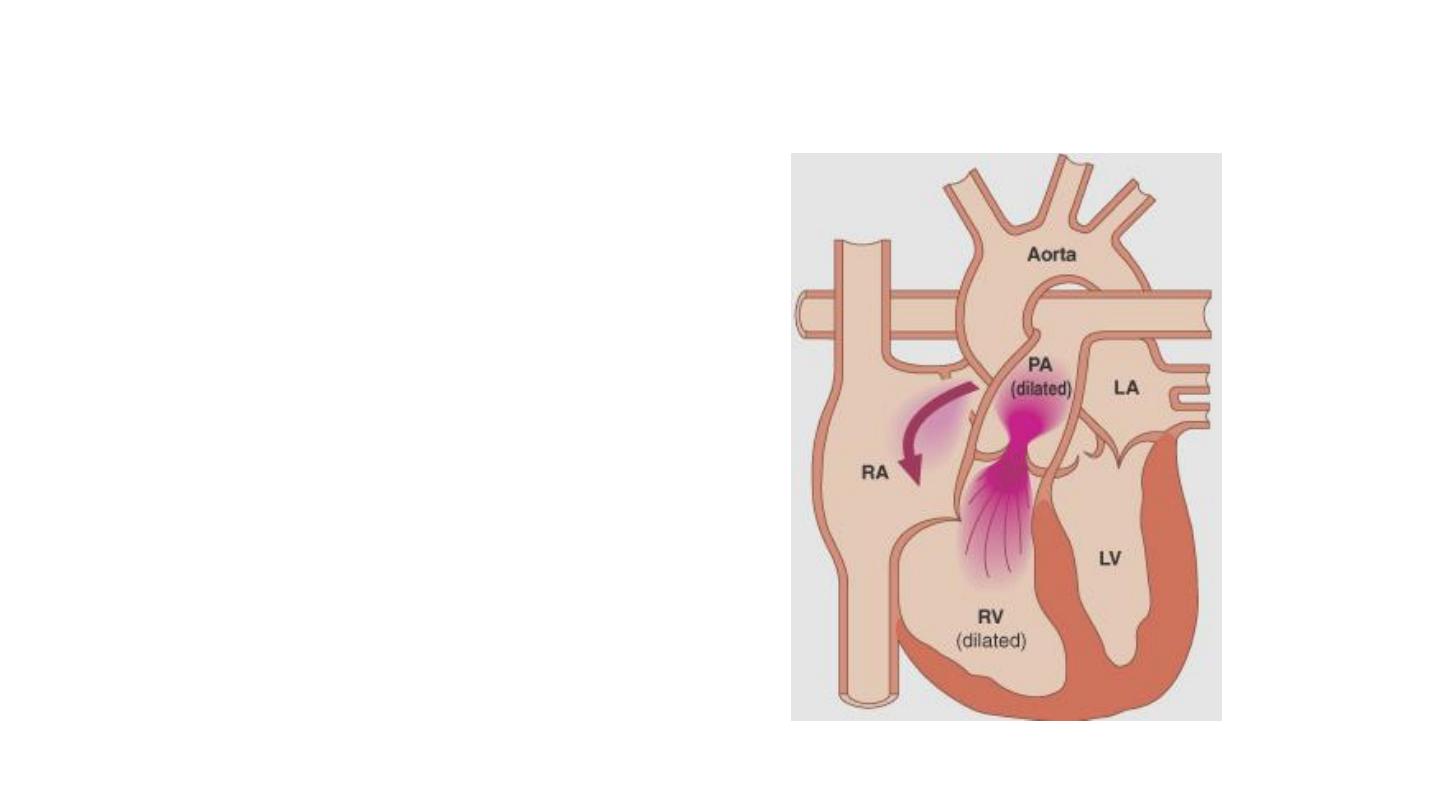
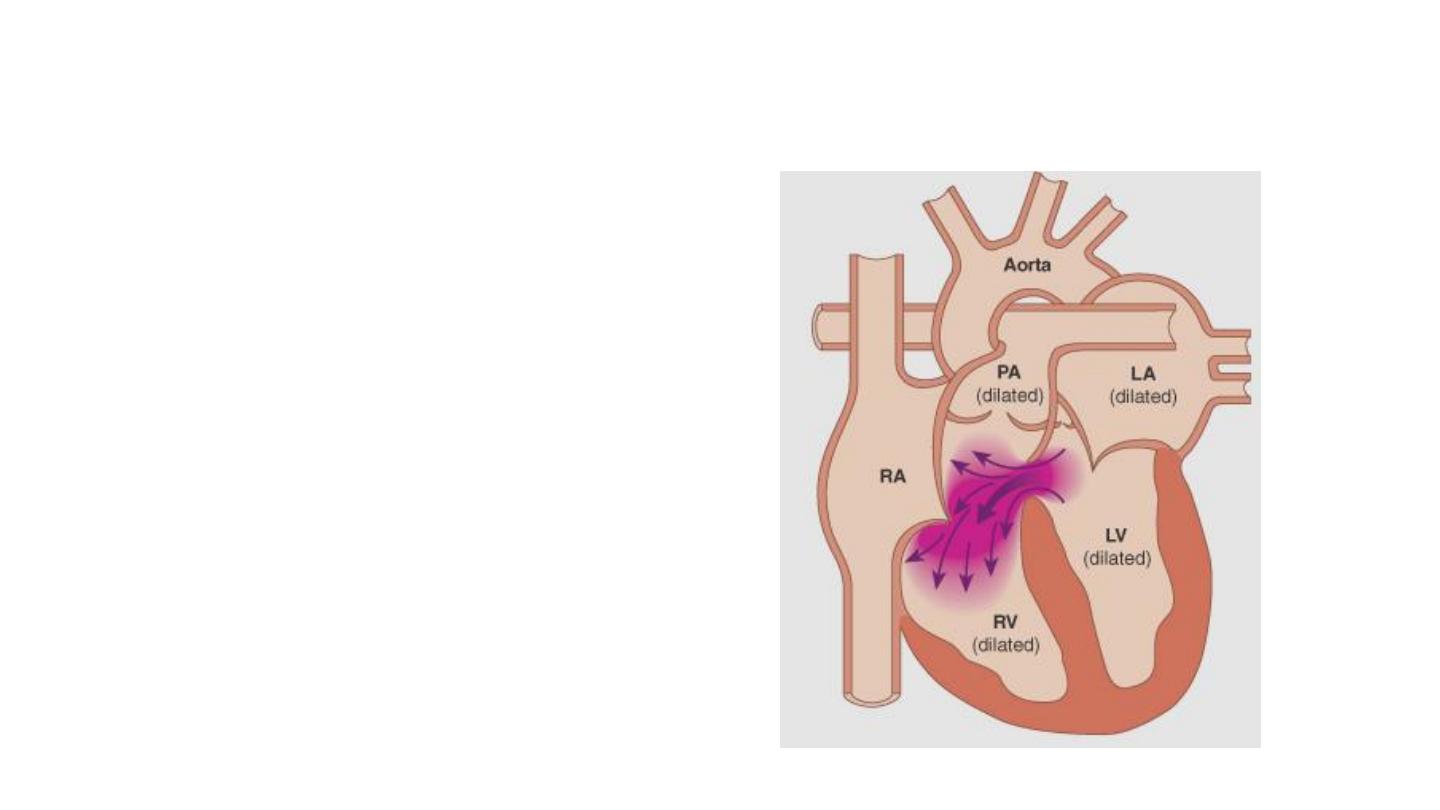
ASD: Pathophysiology
• Shunting of blood
from LA to RA
through the defect
leads to dilatation
of RA, RV, & PA,
but not LA or LV
24

ASD: Symptoms
• Dyspnea
• Recurrent chest infections
• Heart failure
• Arrhythmias (palpitations)
25

ASD: Signs
• ↑ JVP
• Left parasternal heave
• Fixed splitting of S2
• Systolic murmur at the pulmonary area
• NO THRILL is felt at the pulmonary area (unlike
valvular PS)
26

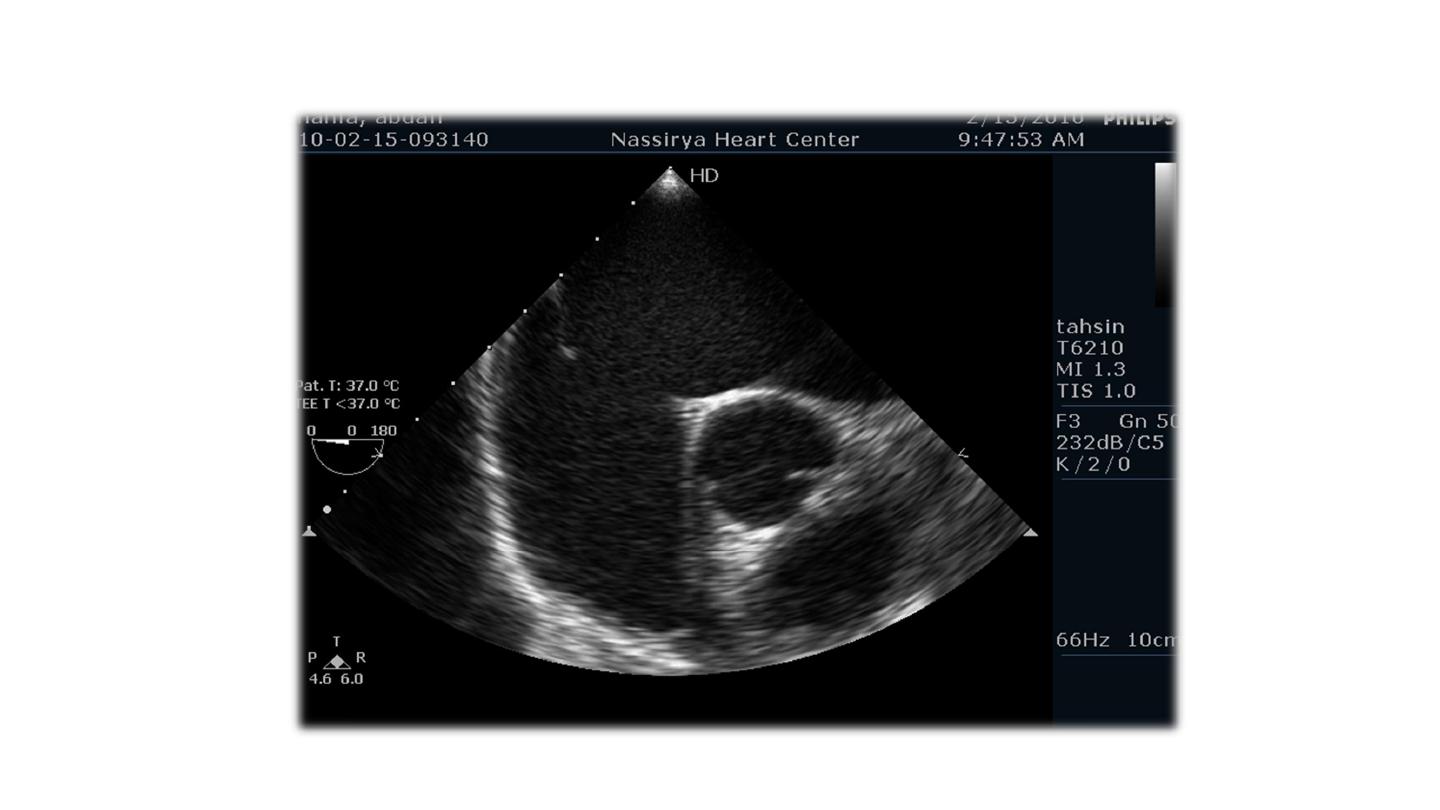
ASD: Investigations
• ECG:
• CXR
• Echocardiography
• Trans-esophageal echocardiography (TEE)
27

ASD: ECG
• Incomplete RBBB
• With secundum ASD: right axis deviation
• With primum ASD: left axis deviation
28
Ostium Secundum ASD
29
Ostium Primum ASD
30

ASD: CXR
• Dilated RV, RA, and PA
• plethoric lungs: increased pulmonary arterial and
venous markings
31

ASD: CXR
32

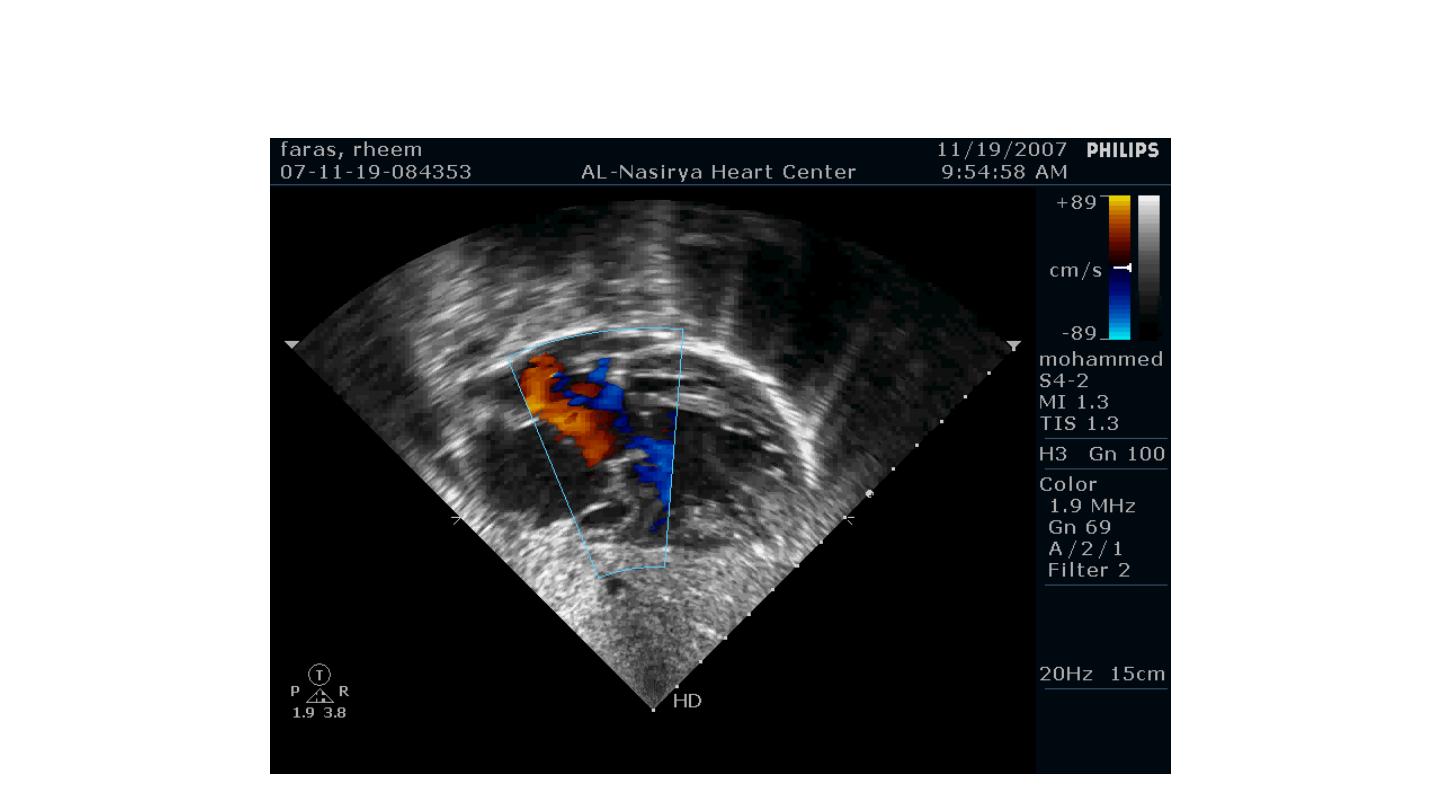
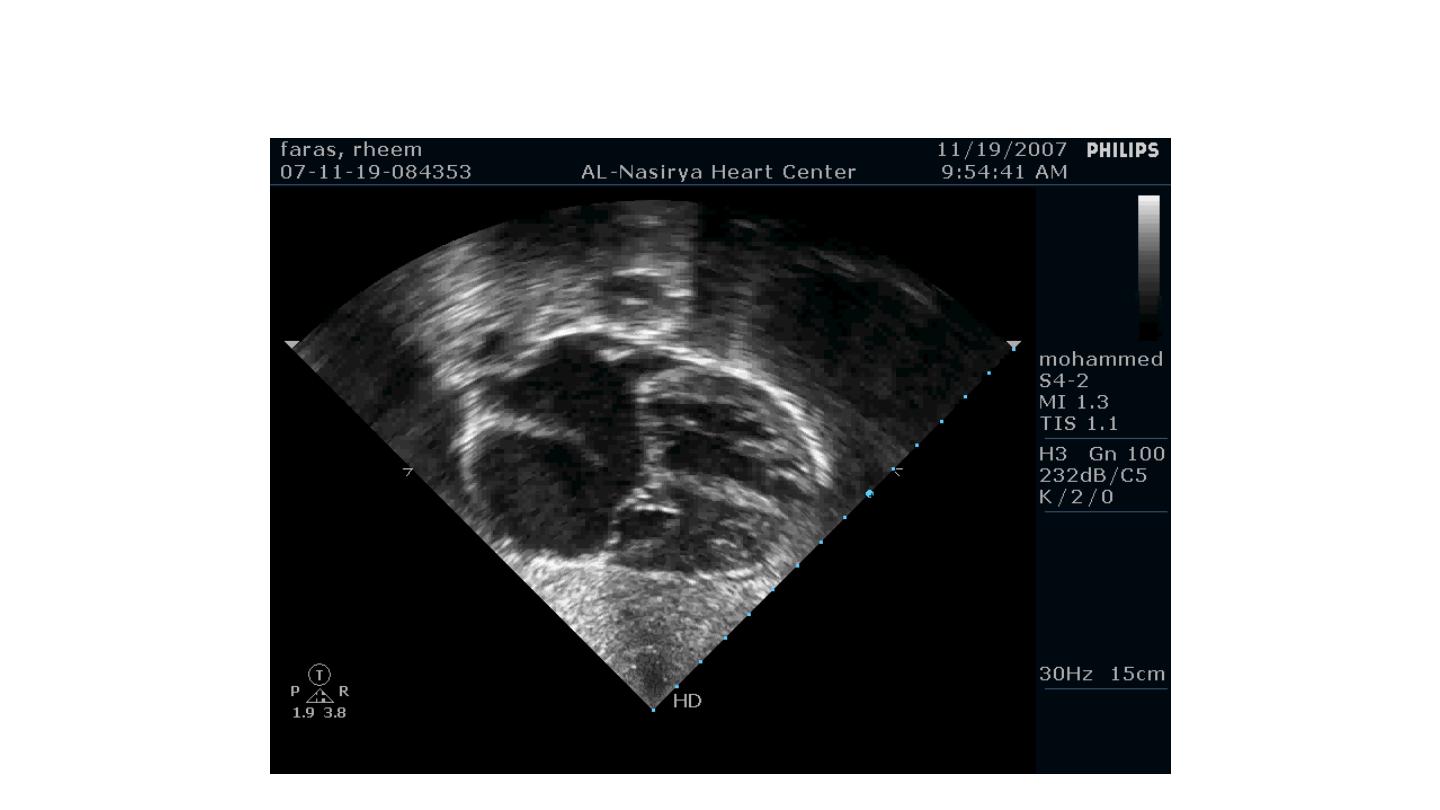
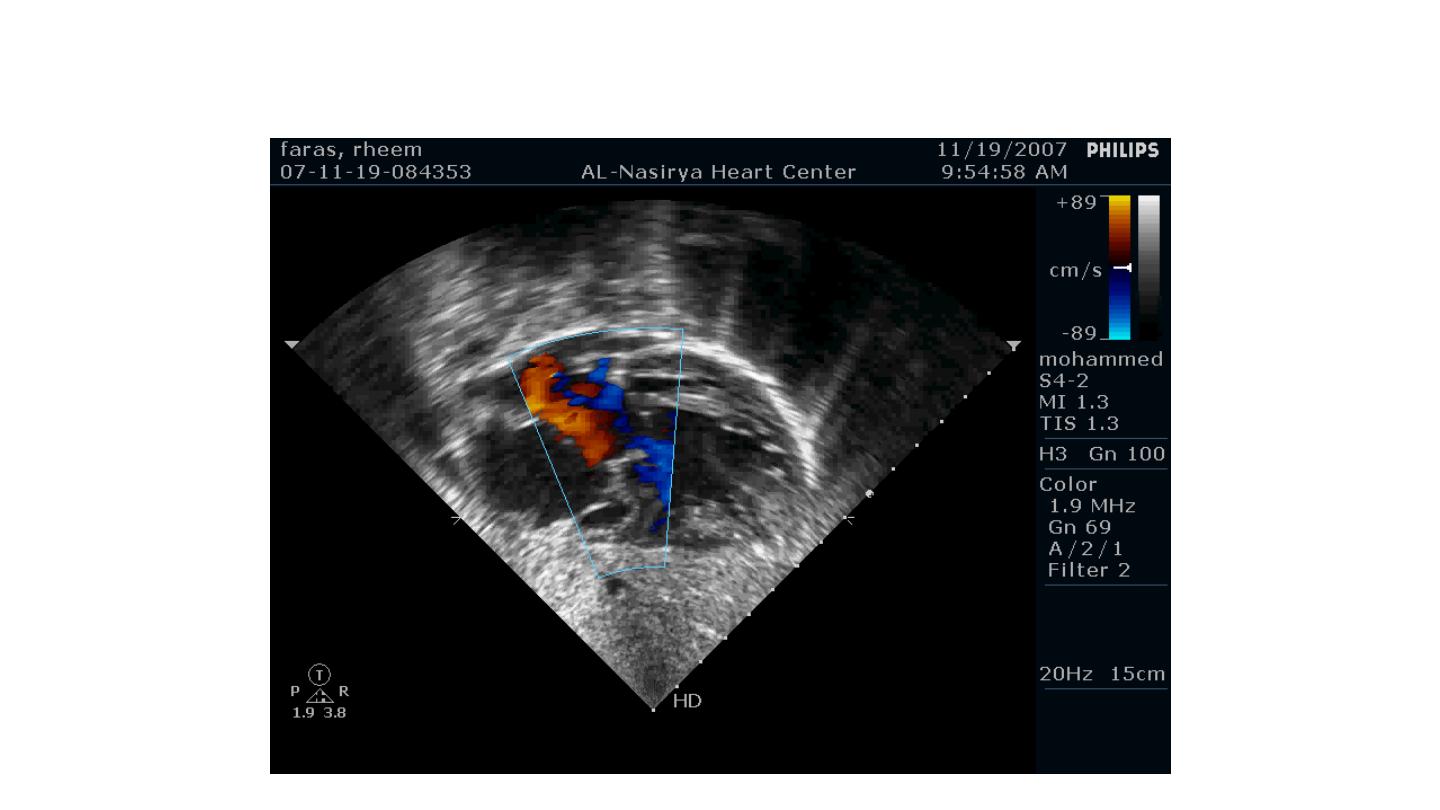
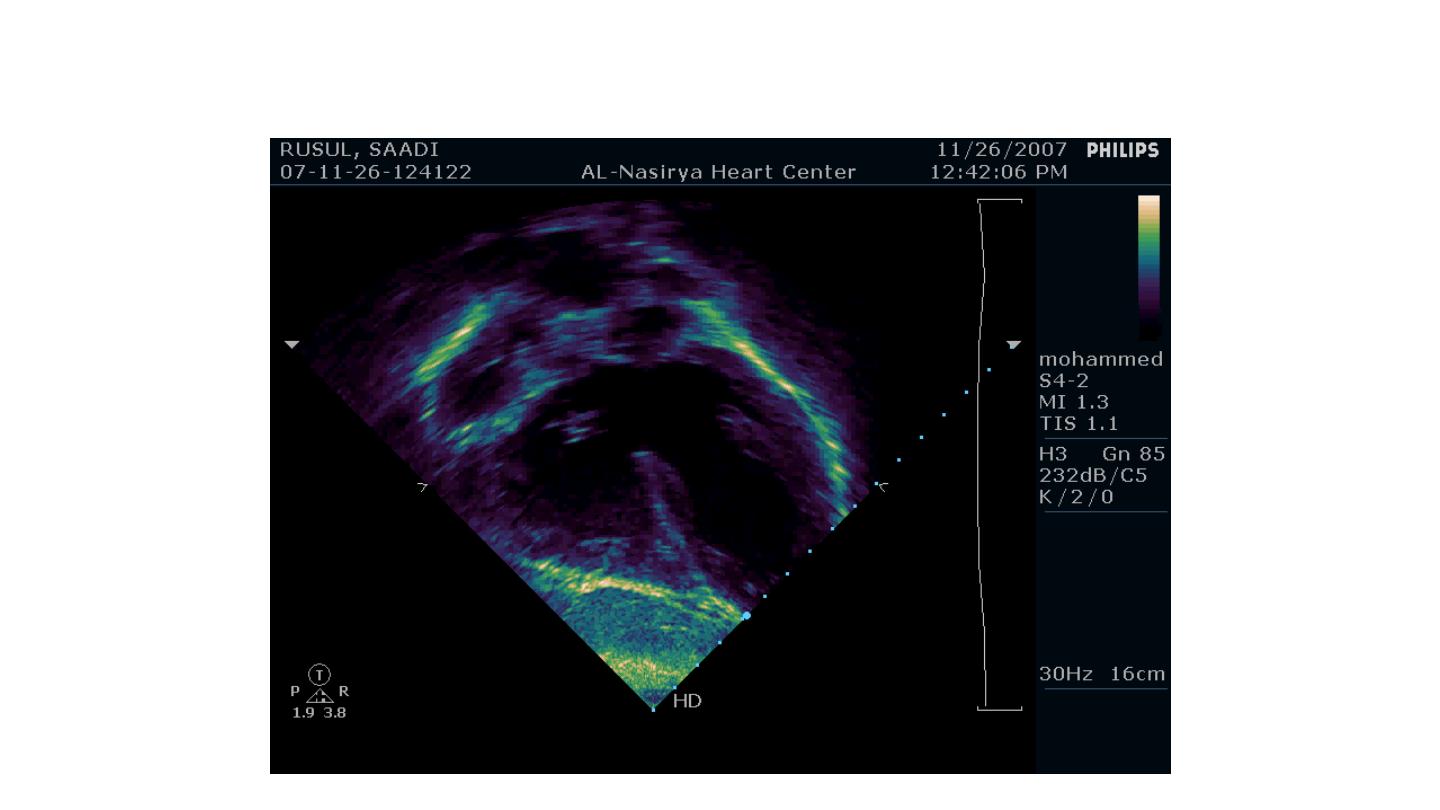
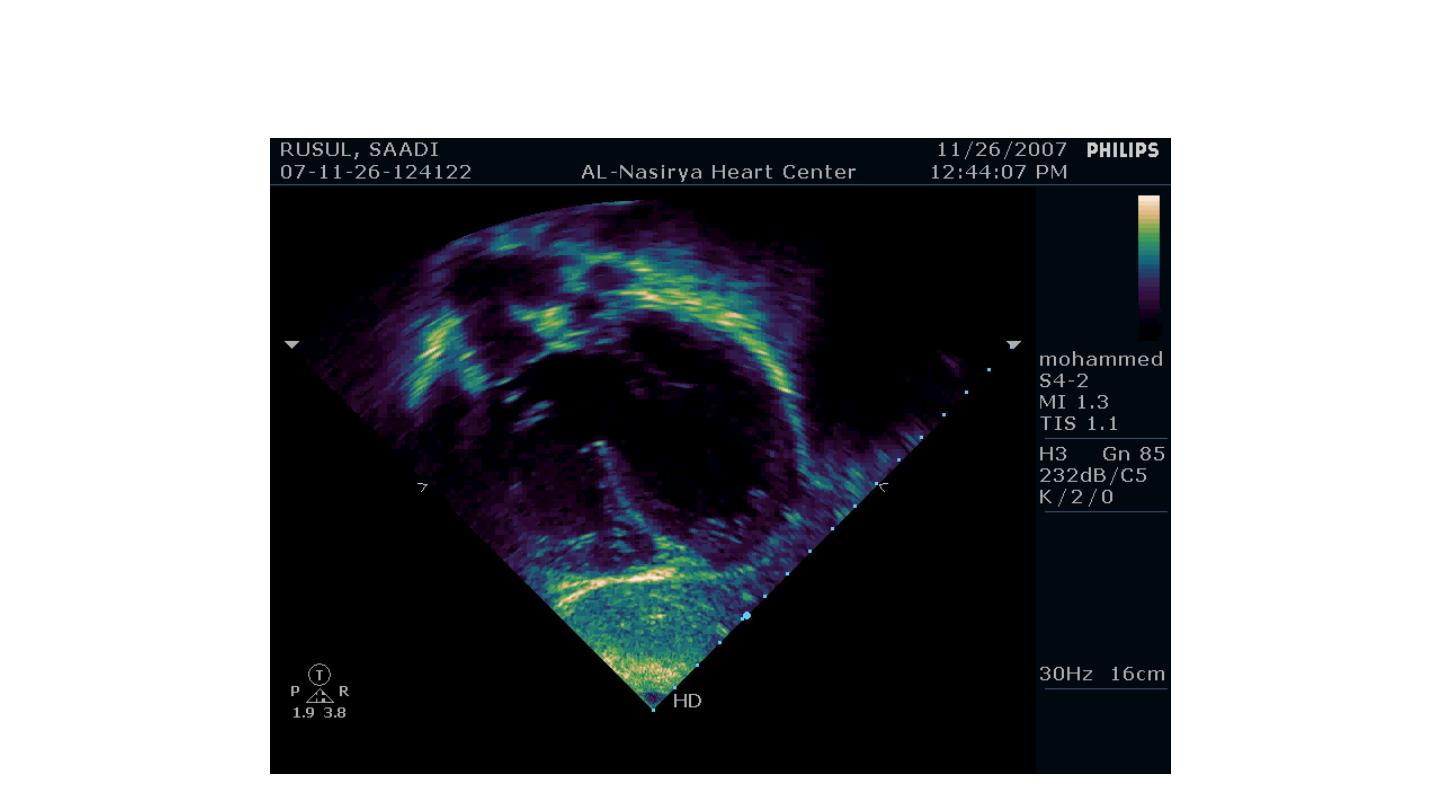
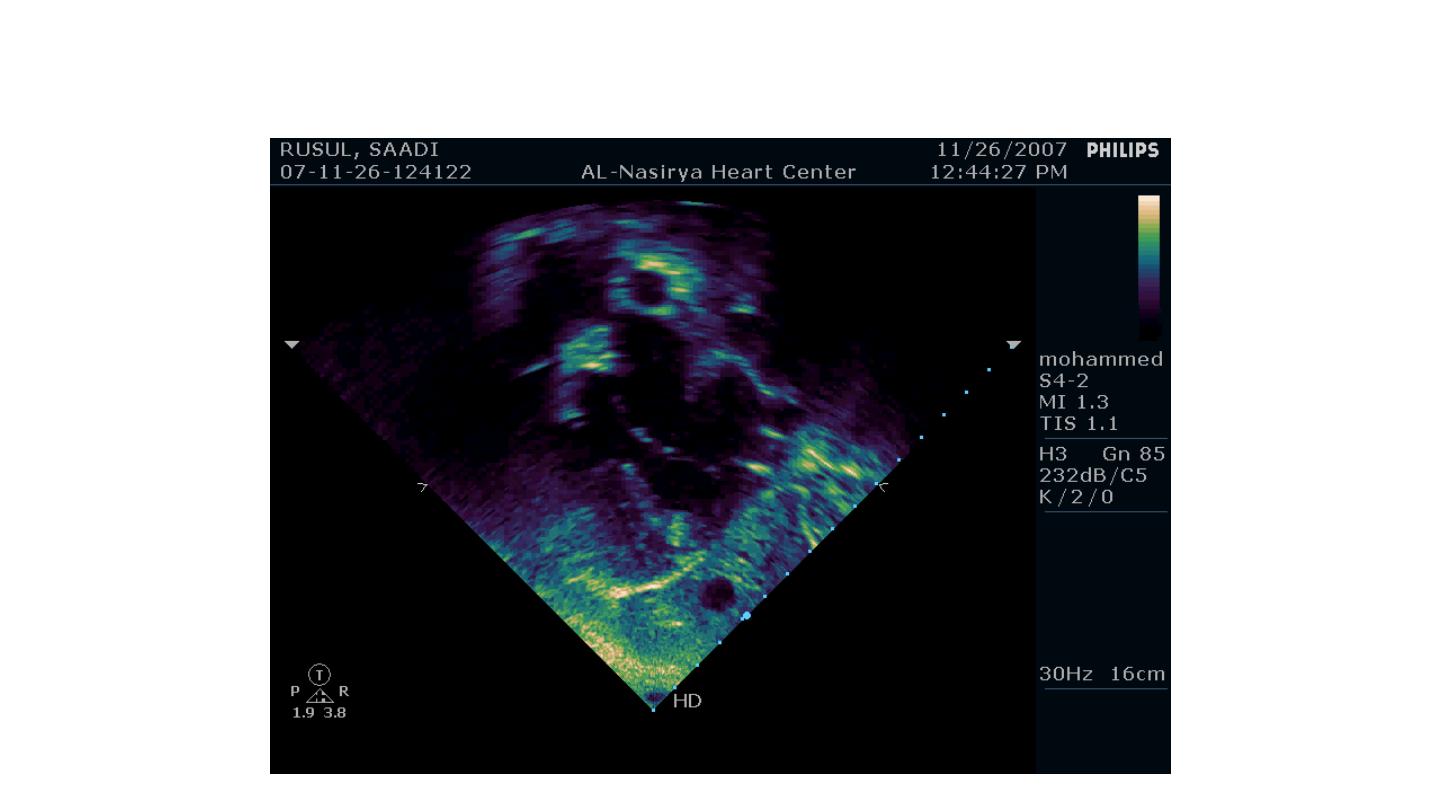
Echocardiography & TEE
• Shows the size of the defect
• The direction of blood flow
• The pulmonary artery pressure
33
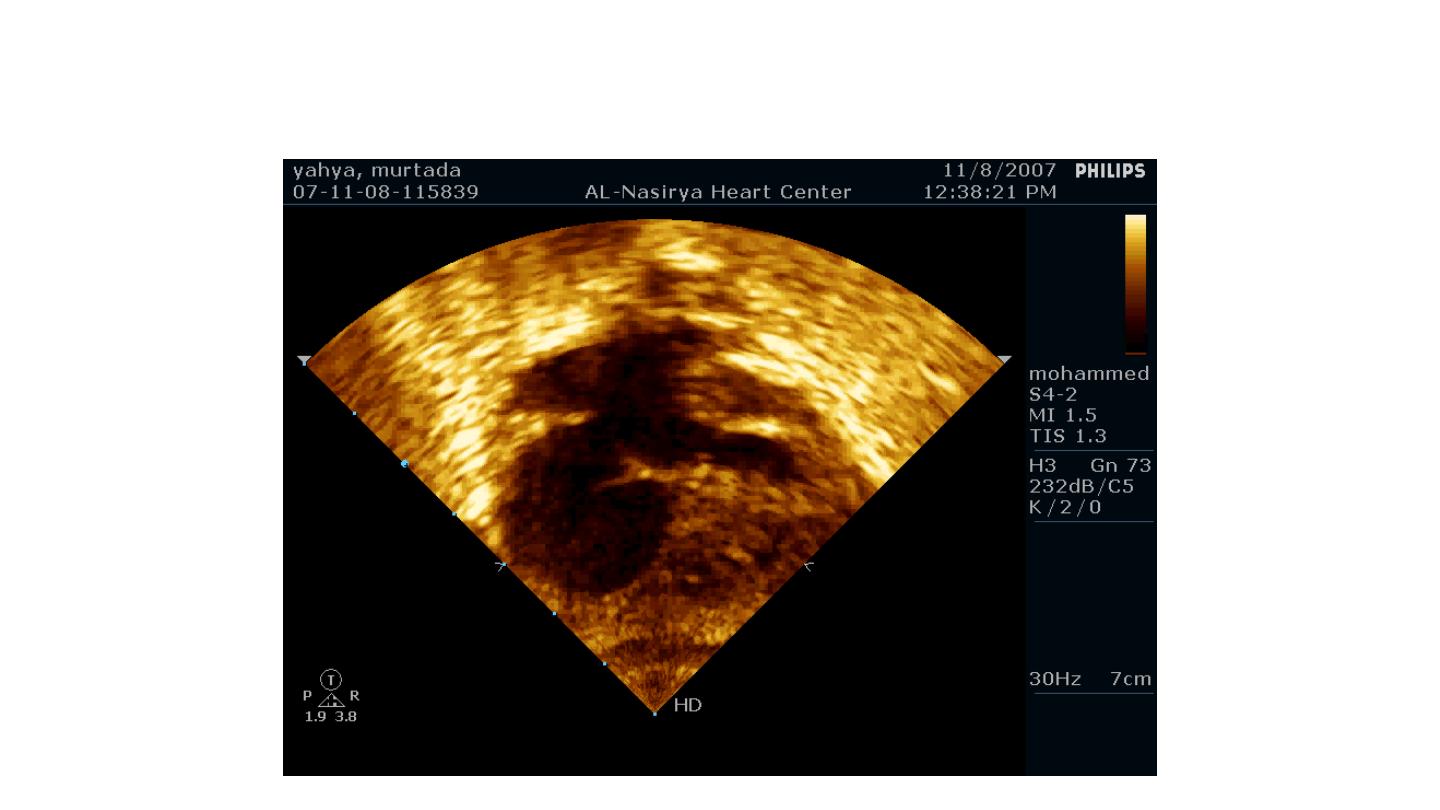
Ostium Secundum ASD
34
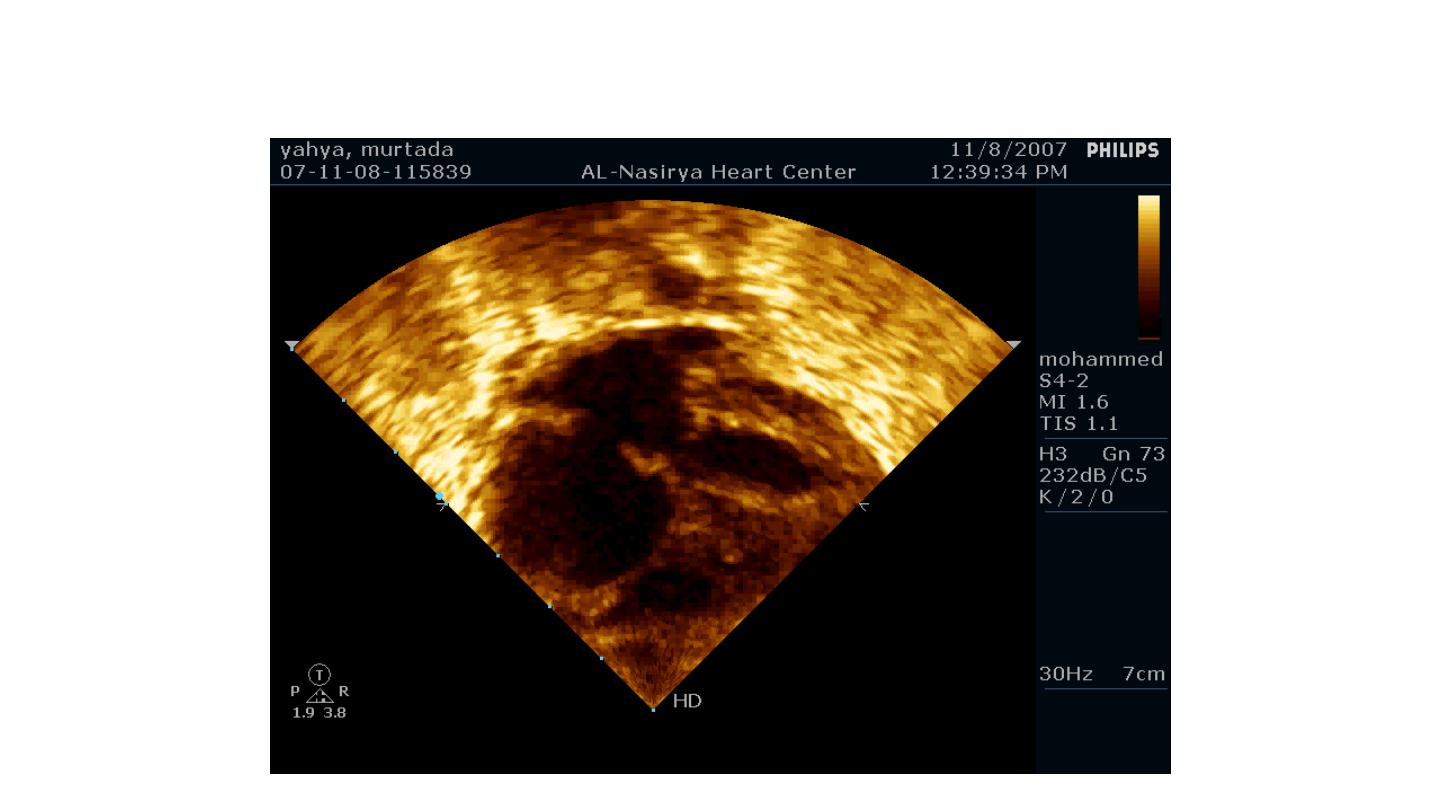
Ostium Secundum ASD
35
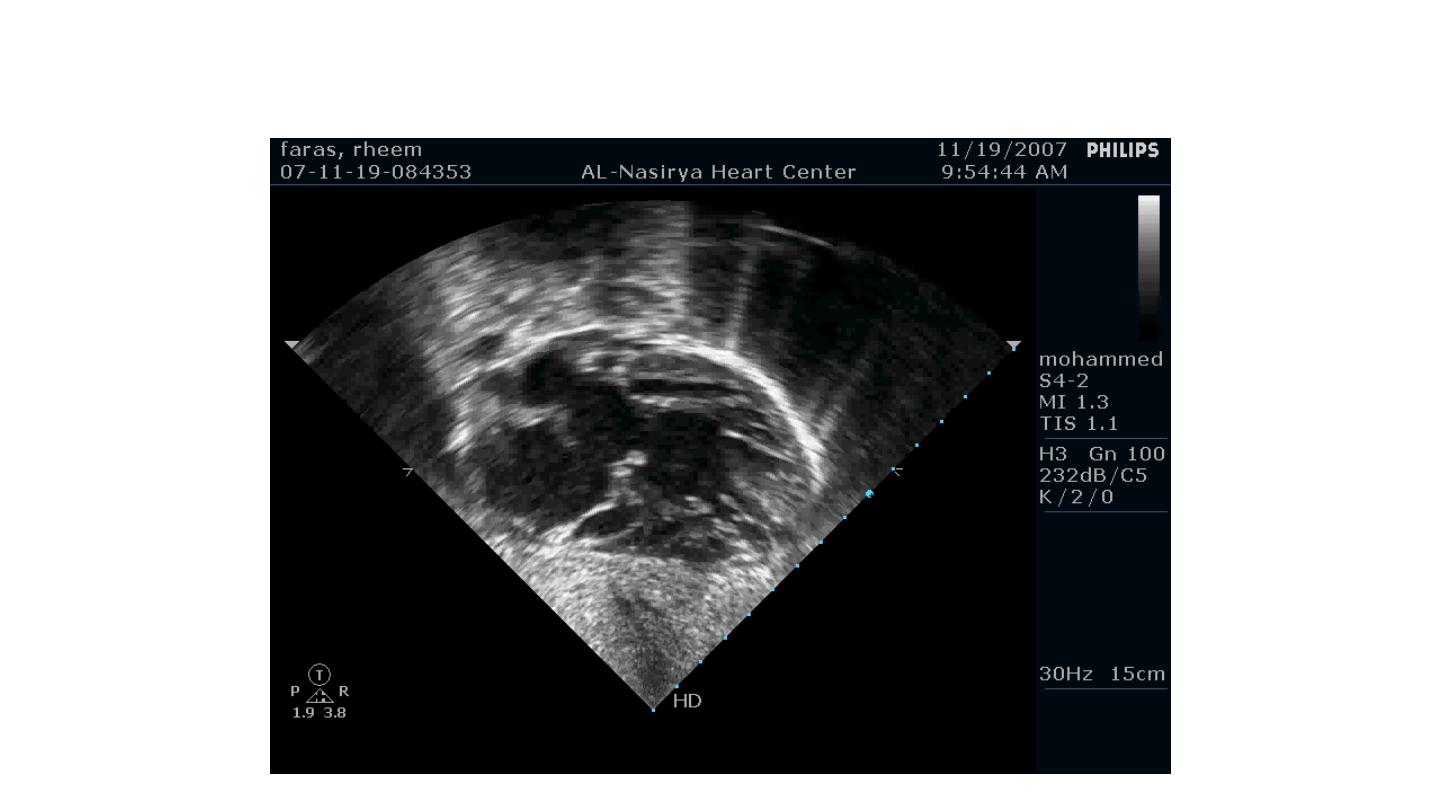
Ostium Primum ASD
36
Ostium Primum ASD
37
38
39
40

ASD: Management
• Surgical closure when the shunt is large (exceeds
1.5:1)
• Recently: closure with implantable closure devices
during cardiac catheterization
• Endocarditis prophylaxis for primum ASD
41

ASD: Management
• Endocarditis prophylaxis is not required in osteum
secundum ASD unless associated with other valvular
or congenital defects
42

Ventricular Septal Defect
(VSD)
Ventricular Septal Defect (VSD)
• Failure of septation
of the ventricles
• The interventricular
septum is normally
composed of small
membranous and
large muscular parts.
44
Ventricular Septal Defect (VSD)
• The usual position of
the defect is around
the membranous
septum
(perimembranous
VSD)
45
VSD: Pathophysiology
• The magnitude of the
shunt depends on the
size of the defect &
the relative systemic &
pulmonary resistance
46
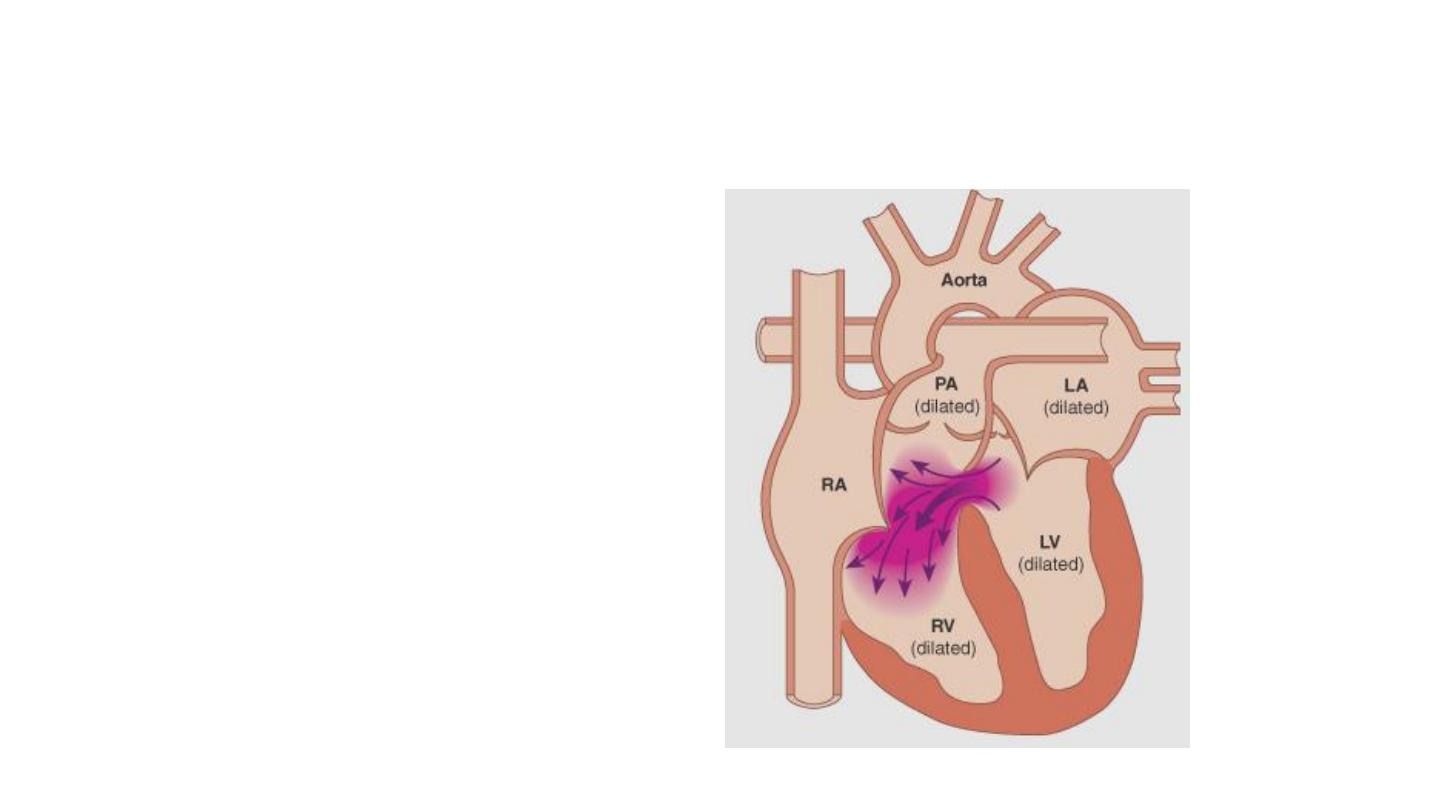
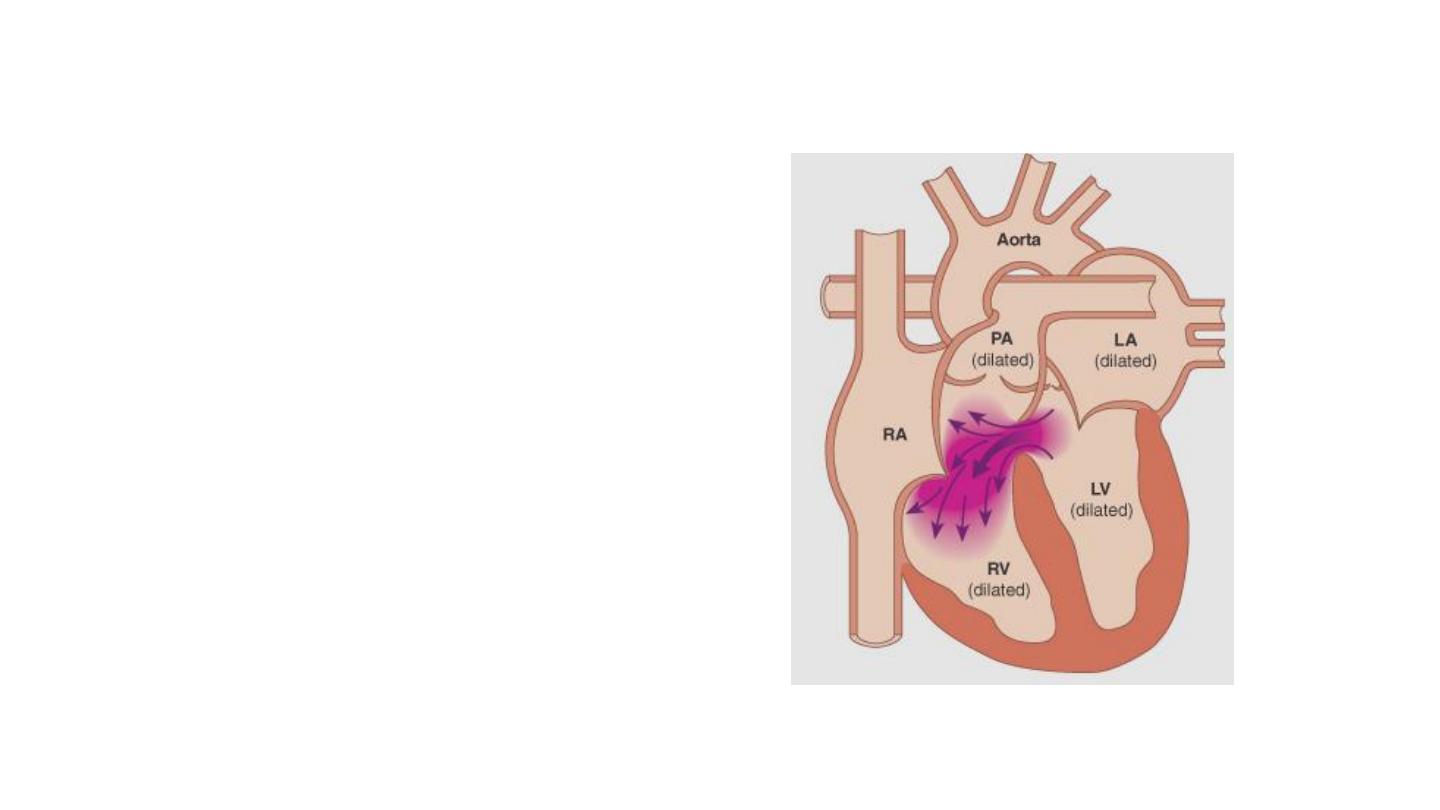
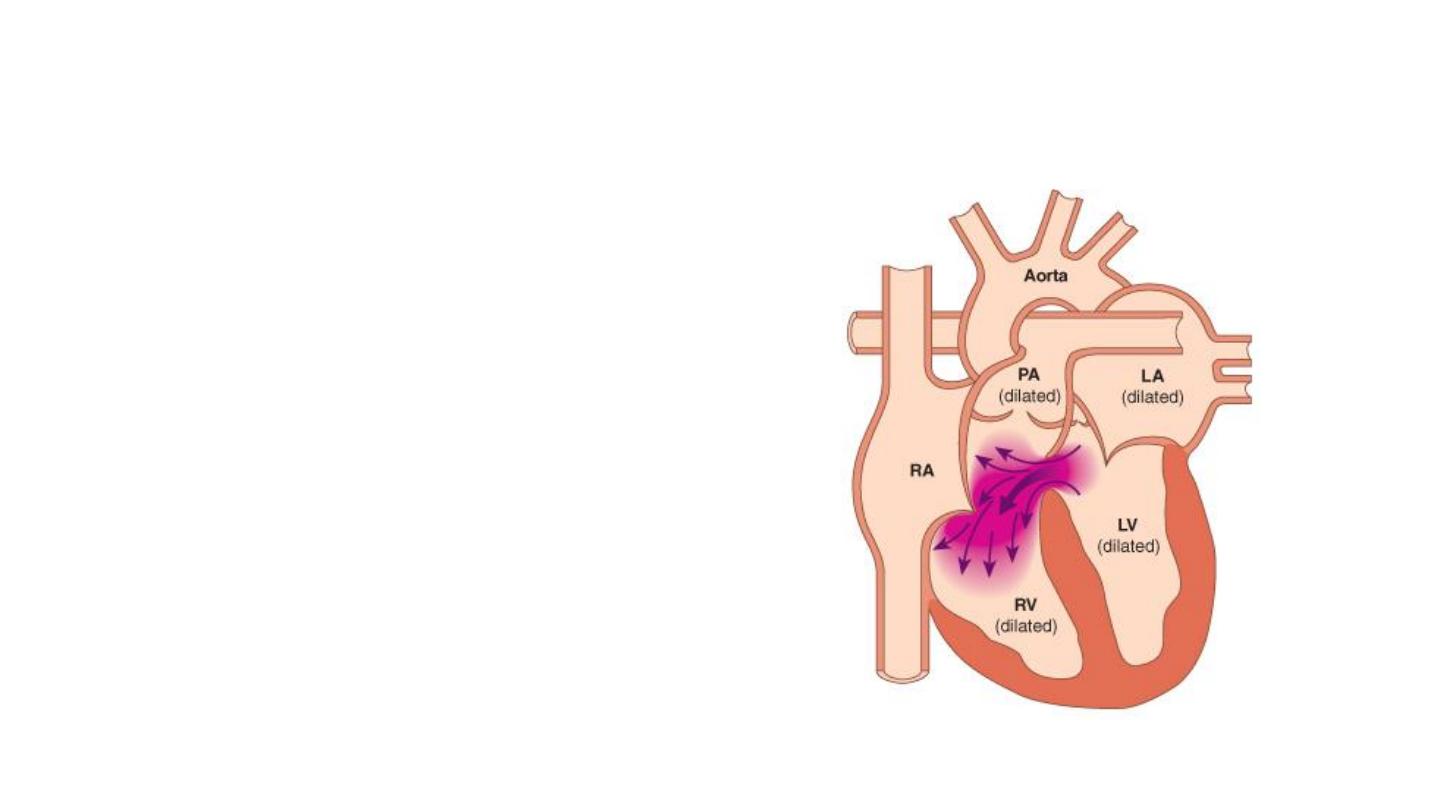
VSD: Pathophysiology
• The shunt involves the
LV, RV, PA, PVs, & LA
47
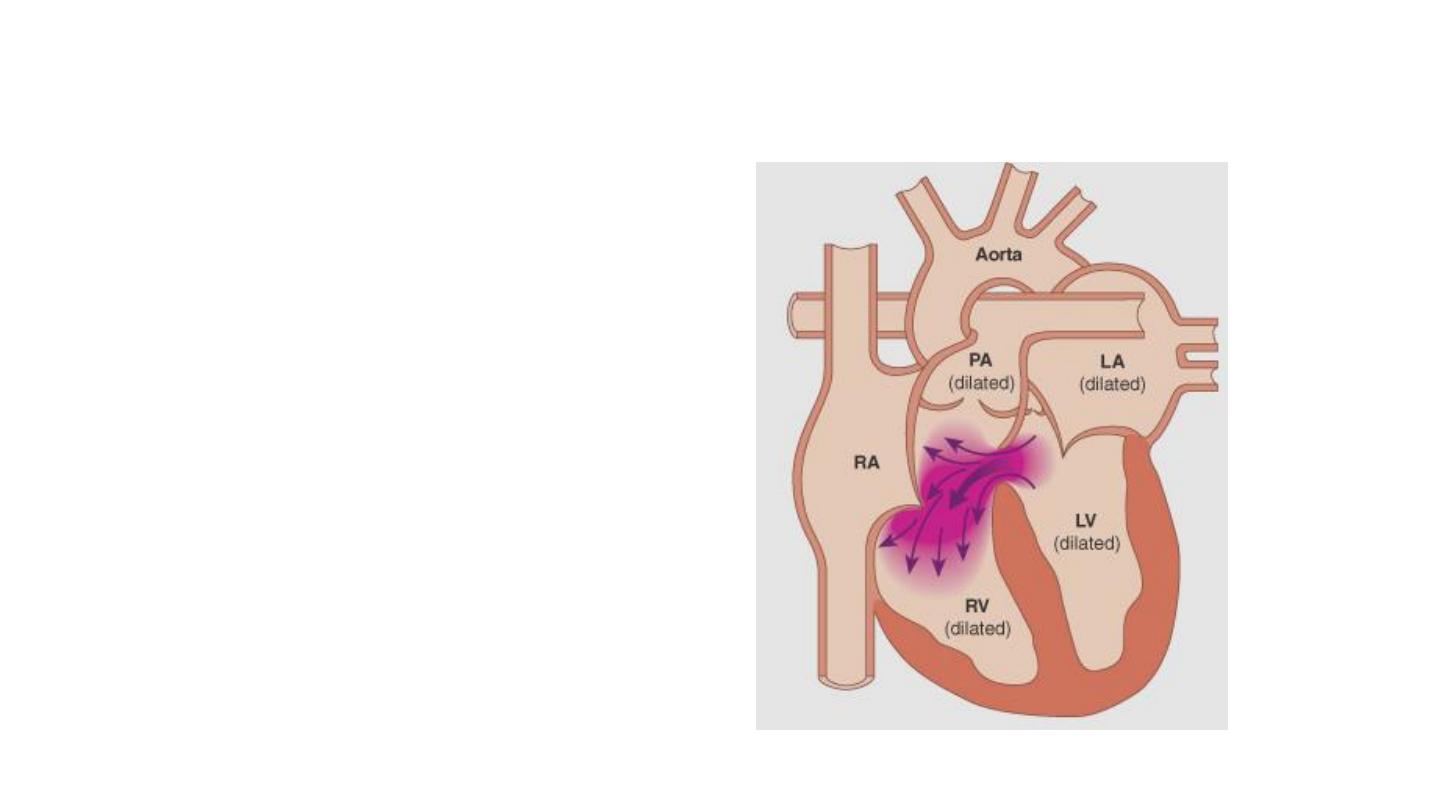
VSD: Pathophysiology
• The shunt does not
involve the RA or
the aorta
• There is increased
flow through the
mitral valve & LV
volume overload
48

VSD: Clinical Presentation
• Dyspnea
• Recurrent chest infections
• Heart failure
• Accidental finding of a murmur
• Eisenmenger’s syndrome
49

VSD: Physical Findings
• Hyperdynamic apex beat
• Systolic thrill: flow through the
defect
• Physiological splitting of S2 (↑ with
breathing)
• S3: LV volume overload
50

VSD: Physical Findings
• LV-RV shunt causes pansystolic murmur at the left
sternal border
• Increased flow through the mitral valve causes
diastolic murmur at the apex
51

VSD: Investigations
• ECG
• CXR
• Echocardiography
52

VSD: CXR
• Plethoric lungs
• Prominent main pulmonary artery
• LA dilatation
• Cardiomegaly of LV configuration
53
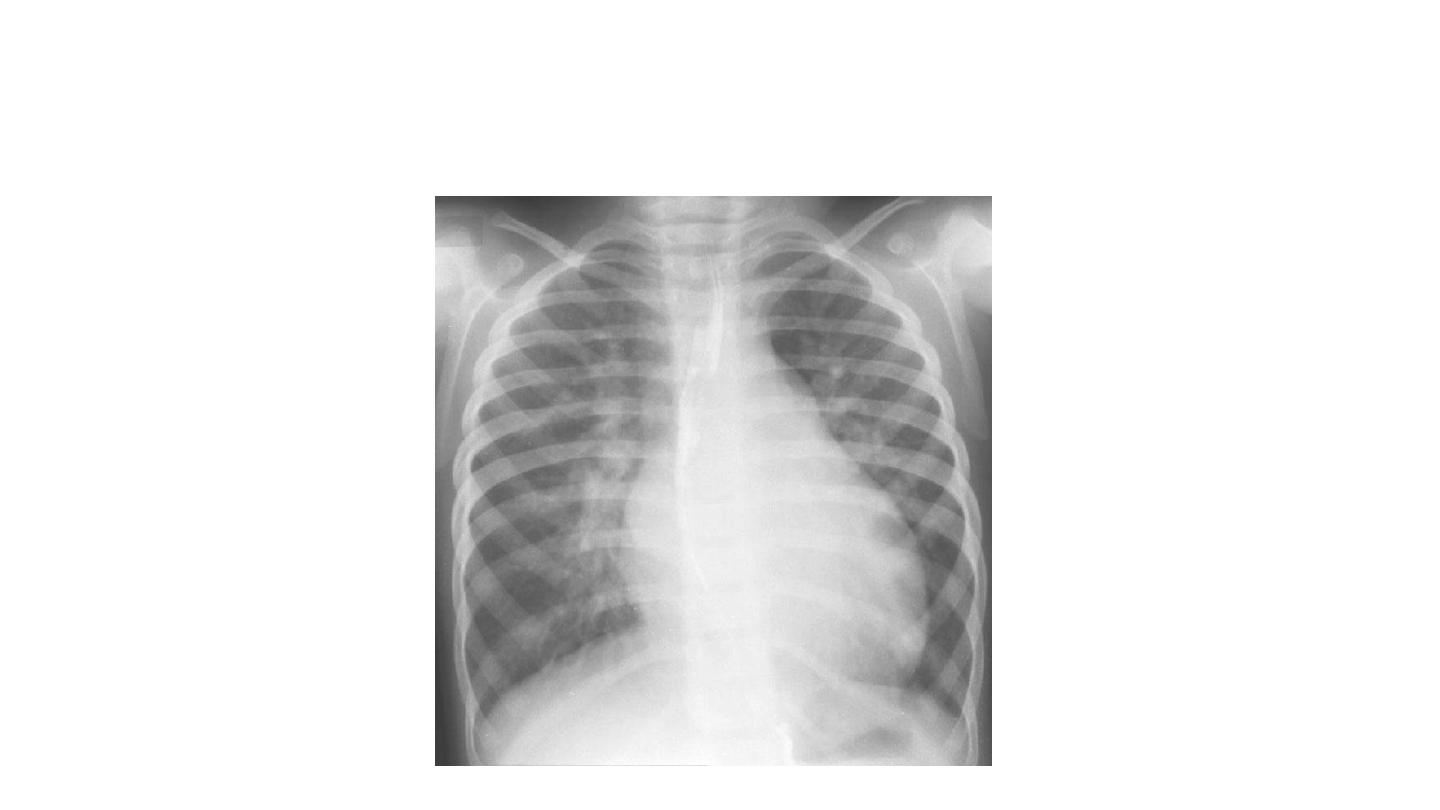
CXR of VSD
54

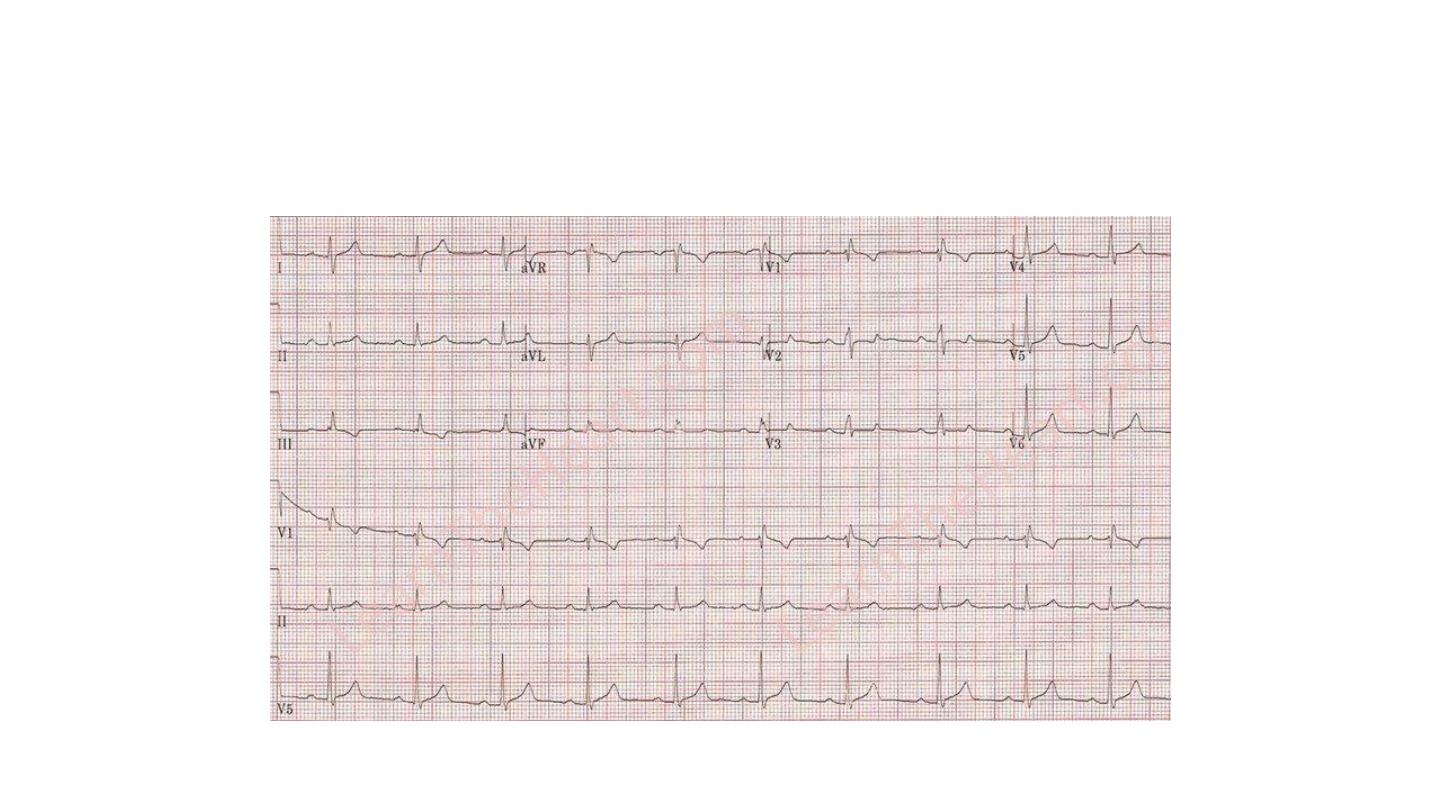
VSD: ECG
• LVH: Tall R waves in V5 & V6 & Deep S waves in
V1 & V2
• Biventricular hypertrophy: tall R in V1 & V2, tall R
in V5 & V6
55
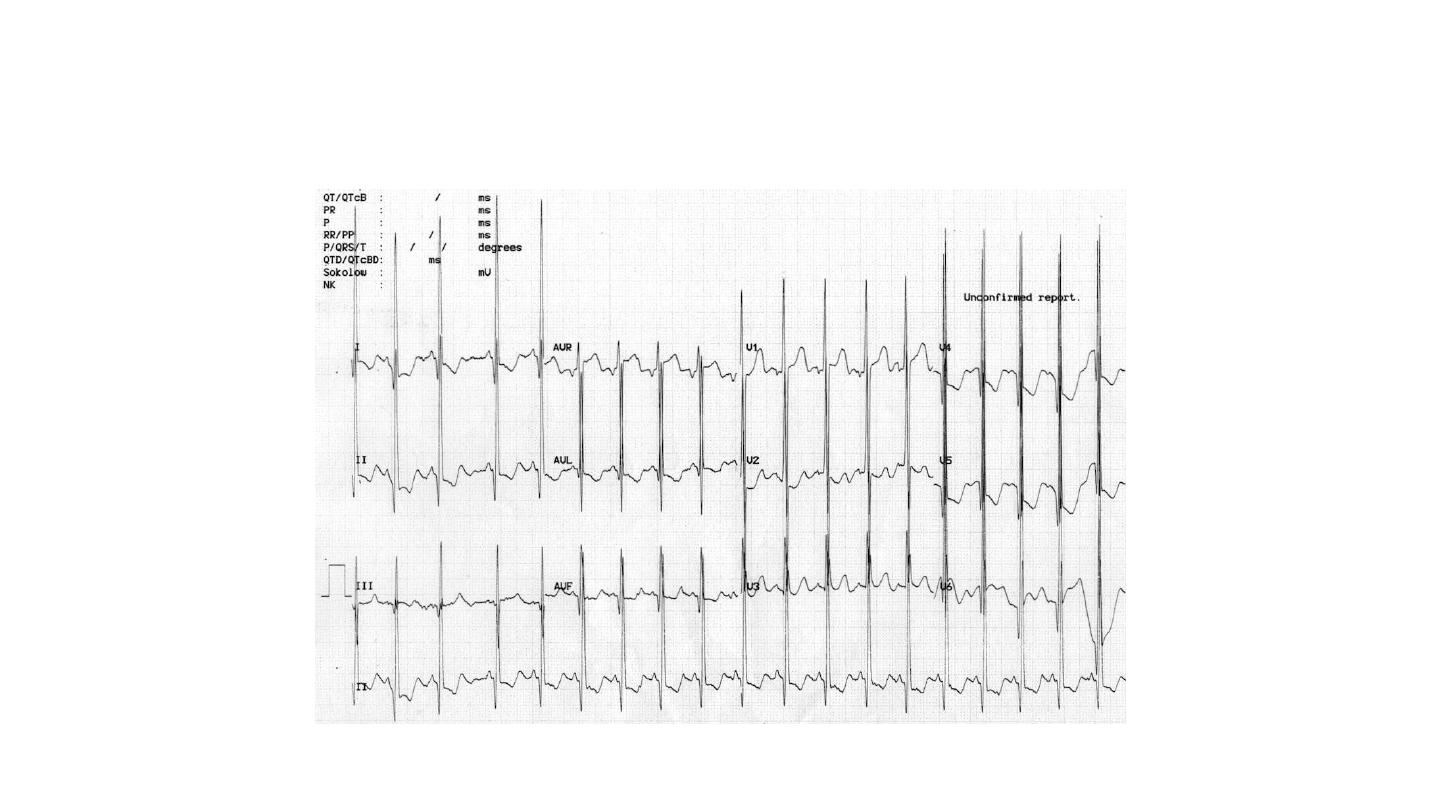
ECG in VSD: Biventricular Hypertrophy
56
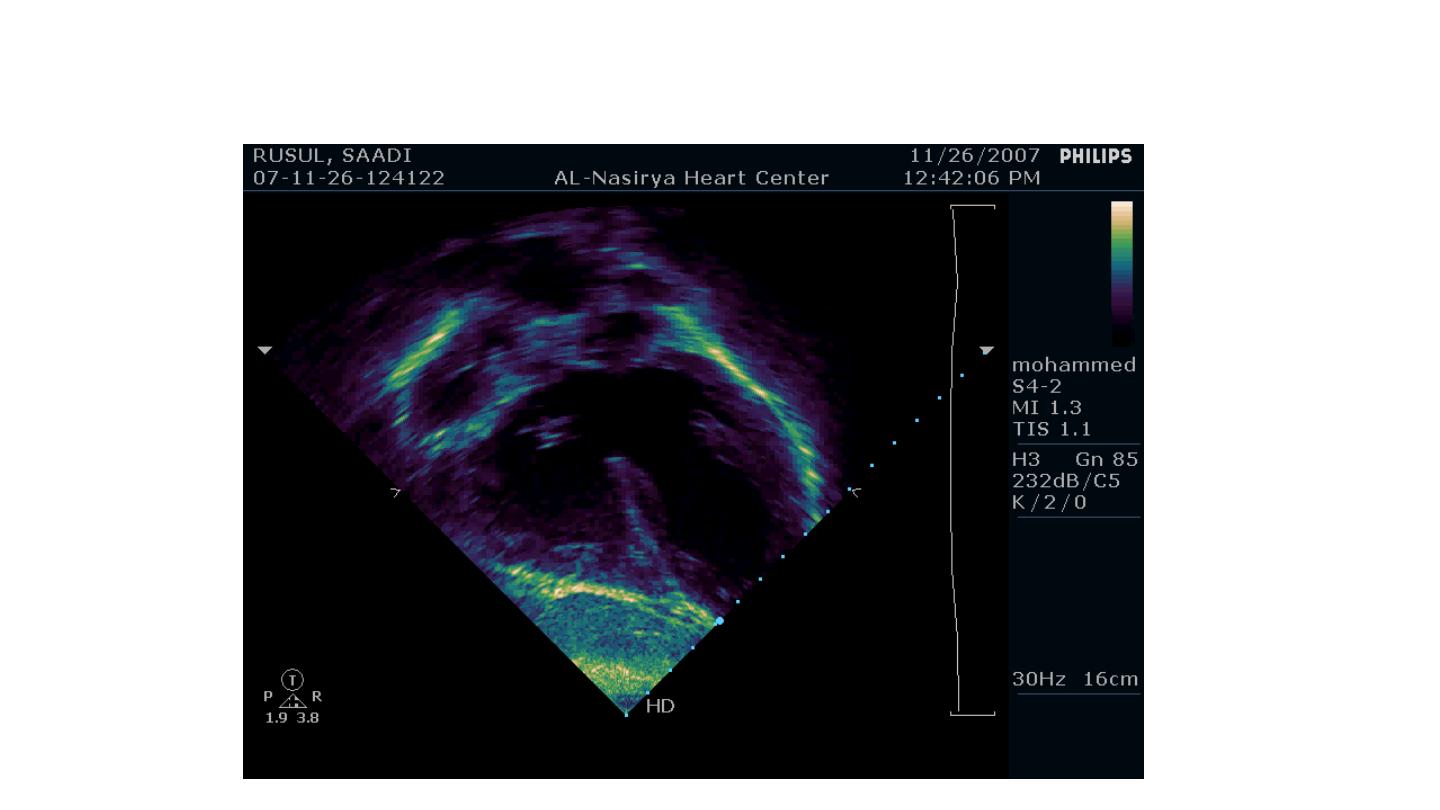
VSD: Echocardiography
57
58
59
60

VSD: Treatment
• Small defects:
– no indication for surgical closure
– Attention should be paid for endocarditis prophylaxis
61

VSD: Treatment
• Large defects with heart failure:
– Medical treatment: digoxin, diuretics, ACEIs
– Definitive treatment: surgical repair of the defect
– Lately: closure by catheterization (occluder)
62

VSD: Treatment
• If the Eisenmenger’s syndrome has developed:
– Heart-lung transplantation
63



