1
Joints of lower limb
stage
st
1
Dr.Kalid Ali Zayer
Hip joint
Contents
1. Structures of the Hip Joint
o 1.1 Articulating Surfaces
2. Ligaments
3. Neurovascular Supply
4. Stabilizing Factors
5. Movements and Muscles
The hip joint is a ball and socket synovial joint, formed by an articulation between
the pelvic acetabulum and the head of the femur.
It forms a connection from the lower limb to the pelvic girdle, and thus is designed
for stability and weight-bearing – rather than a large range of movement.
Structures of the Hip Joint
Articulating Surfaces
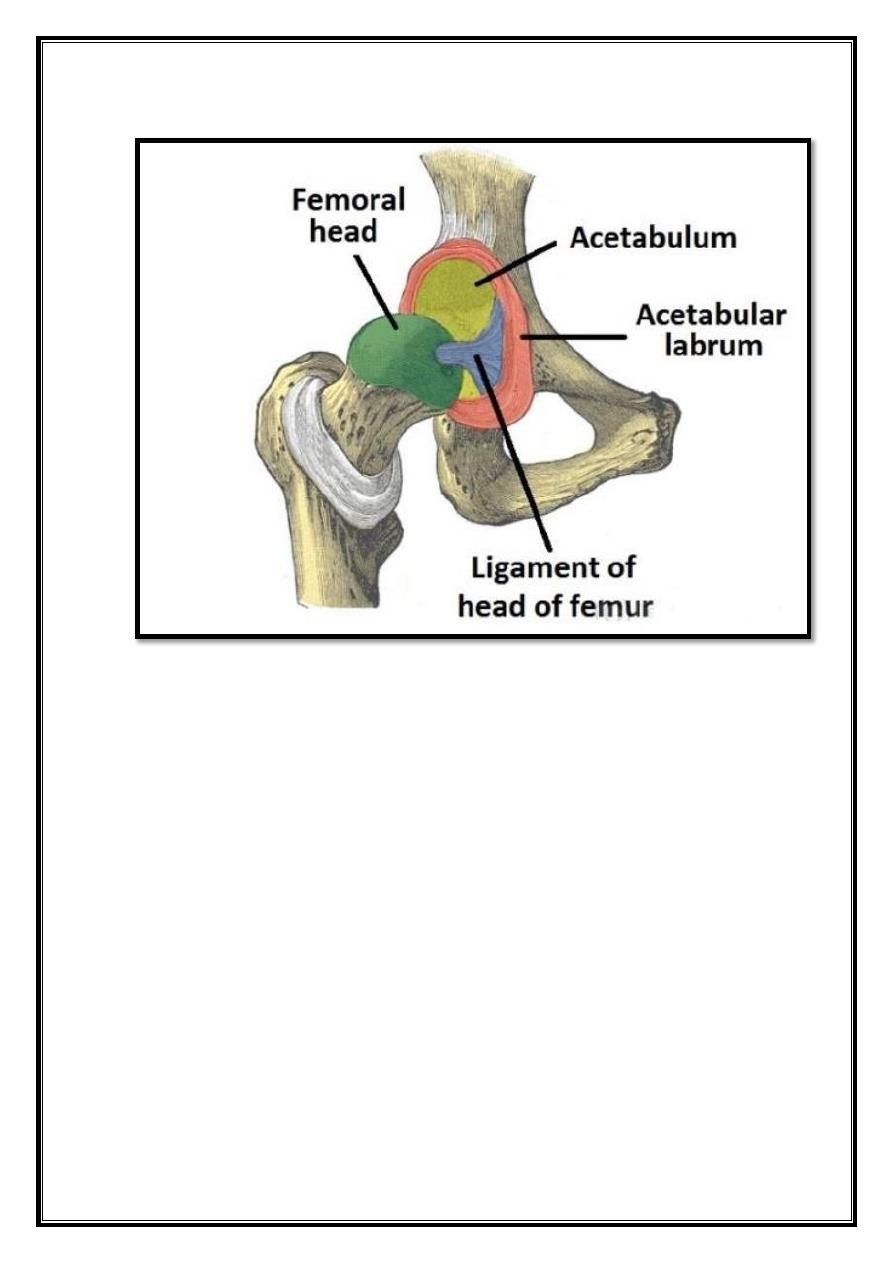
The hip joint consists of an articulation between the
head of femur
and
acetabulum
of the pelvis. The acetabulum is a cup-like depression located on the
inferolateral aspect of the pelvis. Its cavity is deepened by the presence of a
fibrocartilaginous collar – the acetabular labrum.
The head of femur is hemispherical, and fits completely into the concavity of the
acetabulum. Both the acetabulum and head of femur are covered in articular
cartilage, which is thicker at the places of weight bearing. The capsule of the hip
joint attaches to the edge of the acetabulum proximally. Distally, it attaches to the
intertrochanteric line anteriorly and the femoral neck posteriorly.
2
Fig 15 – The articulating surfaces of the hip joint – pelvic acetabulum
and head of the femur.
Ligaments
The ligaments of the hip joint act to increase stability. They can be divided into
two groups –
intracapsular and extracapsular:
Intracapsular
The only intracapsular ligament is the ligament of head of femur. It is a
relatively small structure, which runs from the acetabular fossa to the fovea of
the femur.
It encloses a branch of the obturator artery (artery to head of femur), a minor
source of arterial supply to the hip joint.
Extracapsular
There are three main extracapsular ligaments, continuous with the outer
surface of the hip joint capsule:
3
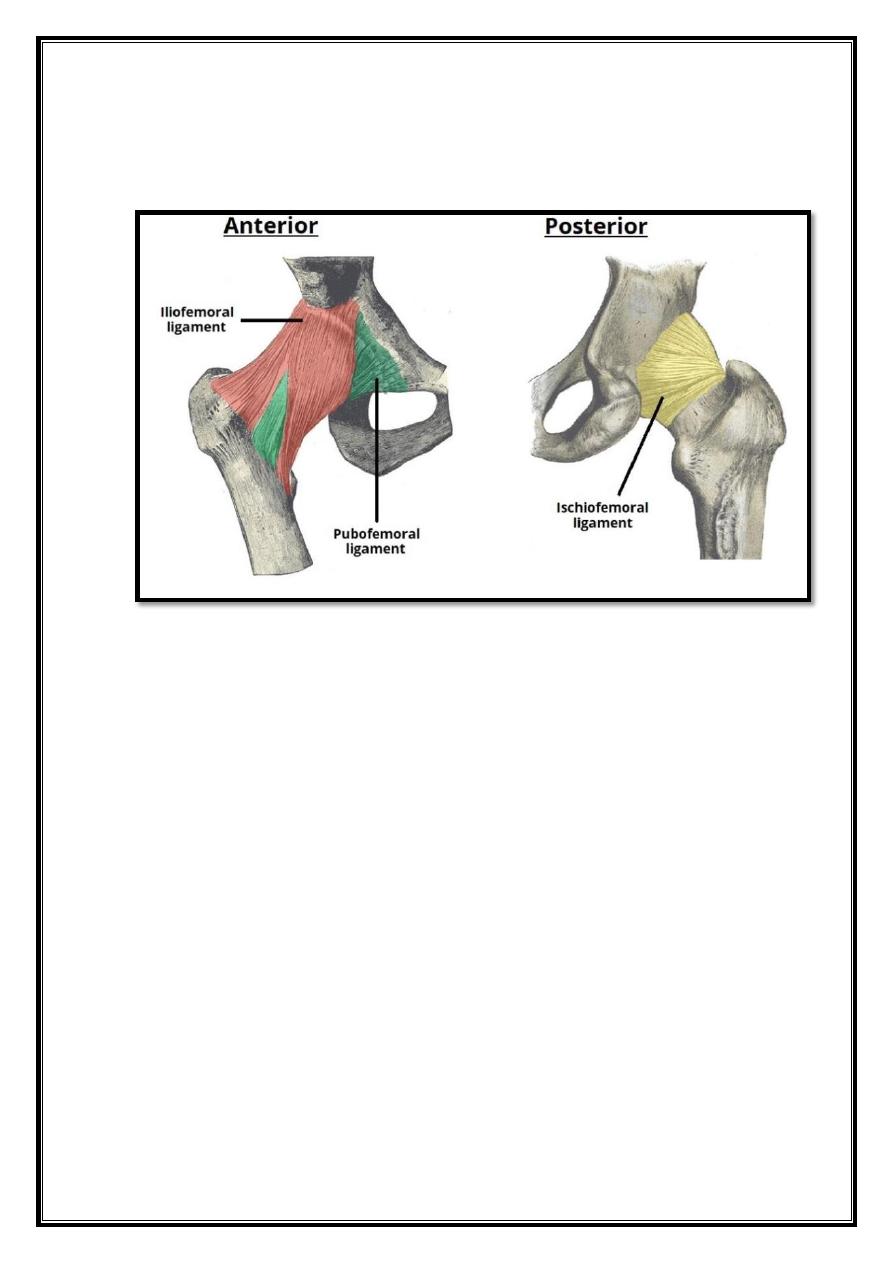
1.
Iliofemoral ligament
– arises from the anterior inferior iliac spine and
then bifurcates before inserting into the intertrochanteric line of the femur.
-
It has a ‘Y’ shaped appearance, and prevents hyperextension of the
hip joint. It is the strongest of the three ligaments.
2.
Pubofemoral
– spans between the superior pubic rami and the
intertrochanteric line of the femur, reinforcing the capsule anteriorly and
inferiorly.
-
It has a triangular shape, and prevents excessive abduction and
extension.
3.
Ischiofemoral
– spans between the body of the ischium and the greater
trochanter of the femur, reinforcing the capsule posteriorly.
-
It has a spiral orientation, and prevents hyperextension and holds
the femoral head in the acetabulum.
Neurovascular Supply
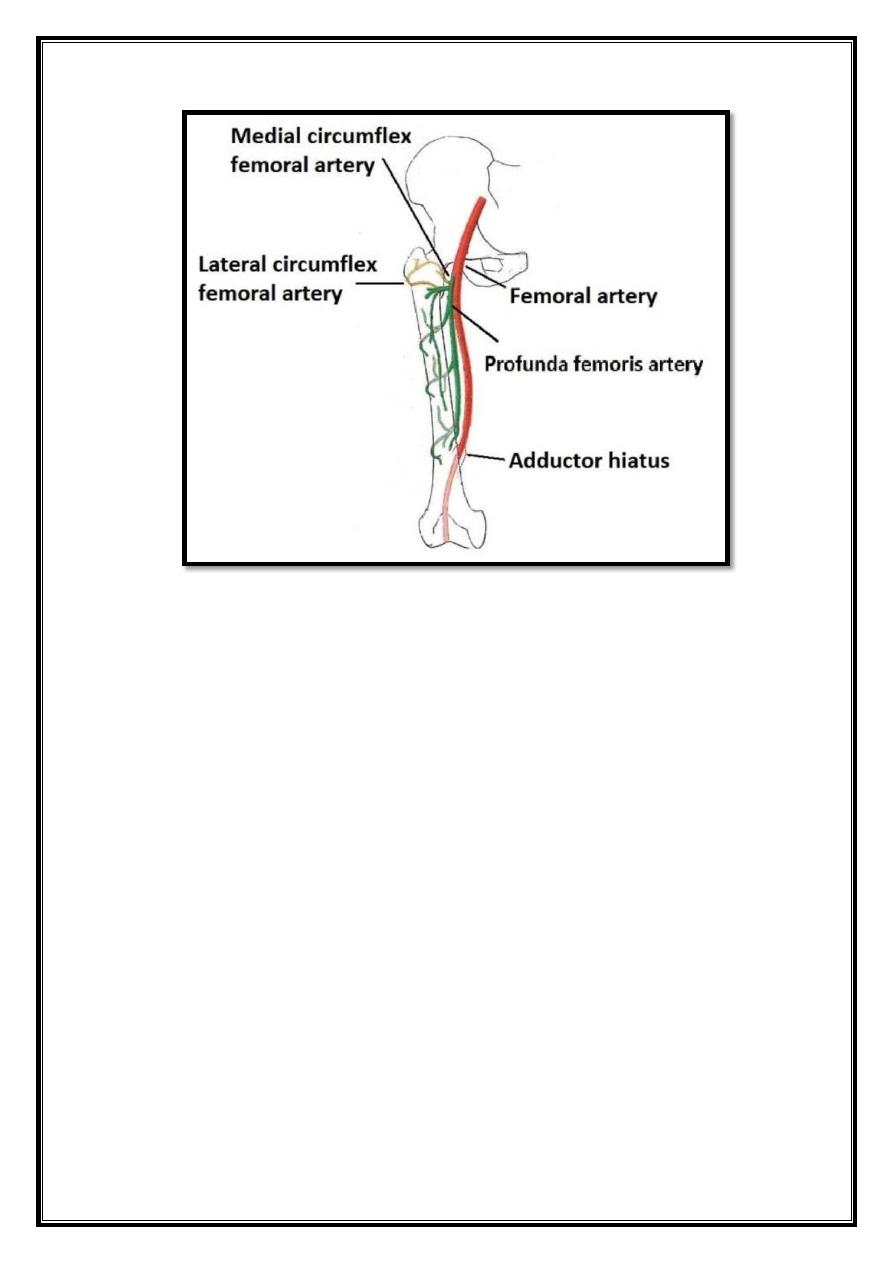
The arterial supply to the hip joint is largely via the medial and lateral
circumflex
femoral arteries
– branches of the profunda femoris artery (deep femoral artery).
They anastomose at the base of the femoral neck to form a ring, from which smaller
arteries arise to supply the hip joint itself. The medial circumflex femoral artery is
responsible for the majority of the arterial supply (the lateral circumflex femoral
artery has to penetrate through the thick iliofemoral ligament). Damage to the
medial circumflex femoral artery can result in
avascular necrosis
of the femoral
head.
The
artery to head of femur
and the superior/inferior gluteal arteries provide
some additional supply. The hip joint is innervated primarily by the
sciatic,
femoral
and
obturator
nerves.
These same nerves innervate the knee, which explains why pain can be referred to
the knee from the hip and vice versa.
4
Fig 16 – The medial and lateral circumflex femoral arteries are the
major blood supply to the hip joint.
Stabilizing Factors
The primary function of the hip joint is to weight-bear. There are a number of
factors that act to increase stability of the joint.
The first structure is the acetabulum. It is deep, and encompasses nearly all of
the head of the femur. This decreases the probability of the head slipping out of
the acetabulum (dislocation).
There is a horseshoe shaped fibrocartilaginous ring around the acetabulum which
increases its depth, known as the
acetabular labrum
. The increase in depth
provides a larger articular surface, further improving the stability of the joint.
The iliofemoral, pubofemoral and ischiofemoral ligaments are very strong, and
along with the thickened joint capsule, provide a large degree of stability. These
ligaments have a unique
spiral orientation
; this causes them to become tighter
when the joint is extended.
In addition, the muscles and ligaments work in a reciprocal fashion at the hip
joint:
Anteriorly
, where the ligaments are strongest, the medial flexors
(located anteriorly) are fewer and weaker.
5
Posteriorly
, where the ligaments are weakest, the medial rotators are
greater in number and stronger – they effectively ‘pull’ the head of the femur into
the acetabulum.
Fig 17 – The extracapsular ligaments of the hip joint; ileofemoral,
pubofemoral and ischiofemoral ligaments.
Movements and Muscles
The movements that can be carried out at the hip joint are listed below, along
with the principle muscles responsible for each action:
Flexion
– iliopsoas, rectus femoris, sartorius, pectineus.
Extension
– gluteus maximus; semimembranosus, semitendinosus and biceps
femoris (the hamstrings).
Abduction
– gluteus medius, gluteus minimus, piriformis and tensor fascia latae.
Adduction
– adductors longus, brevis and magnus, pectineus and gracilis.
Lateral rotation
– biceps femoris, gluteus maximus, piriformis, assisted by the
obturators, gemilli and quadratus femoris.
Medial rotation
– anterior fibers of gluteus medius and minimus, tensor fascia
latae
The degree to which flexion at the hip can occur depends on whether the knee is
flexed – this relaxes the
hamstring muscles
, and increases the range of flexion.
Extension at the hip joint is limited by the joint capsule and the
iliofemoral
ligament
. Theses tructures become taut during extension to limit further
movement.
6
knee joint
Contents
1. Articulating Surfaces
2. Neurovasculature
3. Menisci
4. Bursae
5. Ligaments
6. Movements
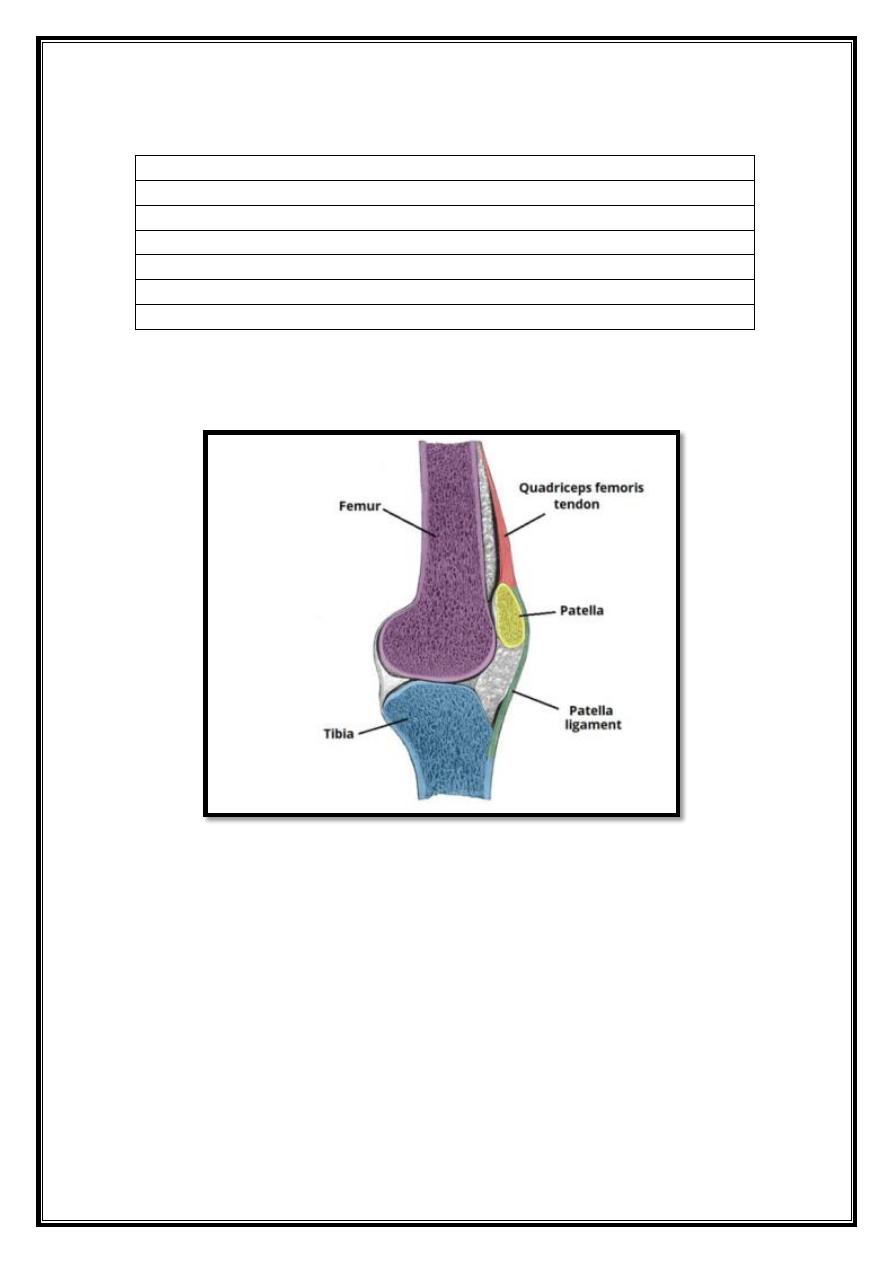
The knee joint is a hinge type synovial joint, which mainly allows for flexion
and extension (and a small degree of medial and lateral rotation). It is formed by
articulations between the patella, femur and tibia.
Fig 18 – The femur, tibia and patella of the knee joint.
7
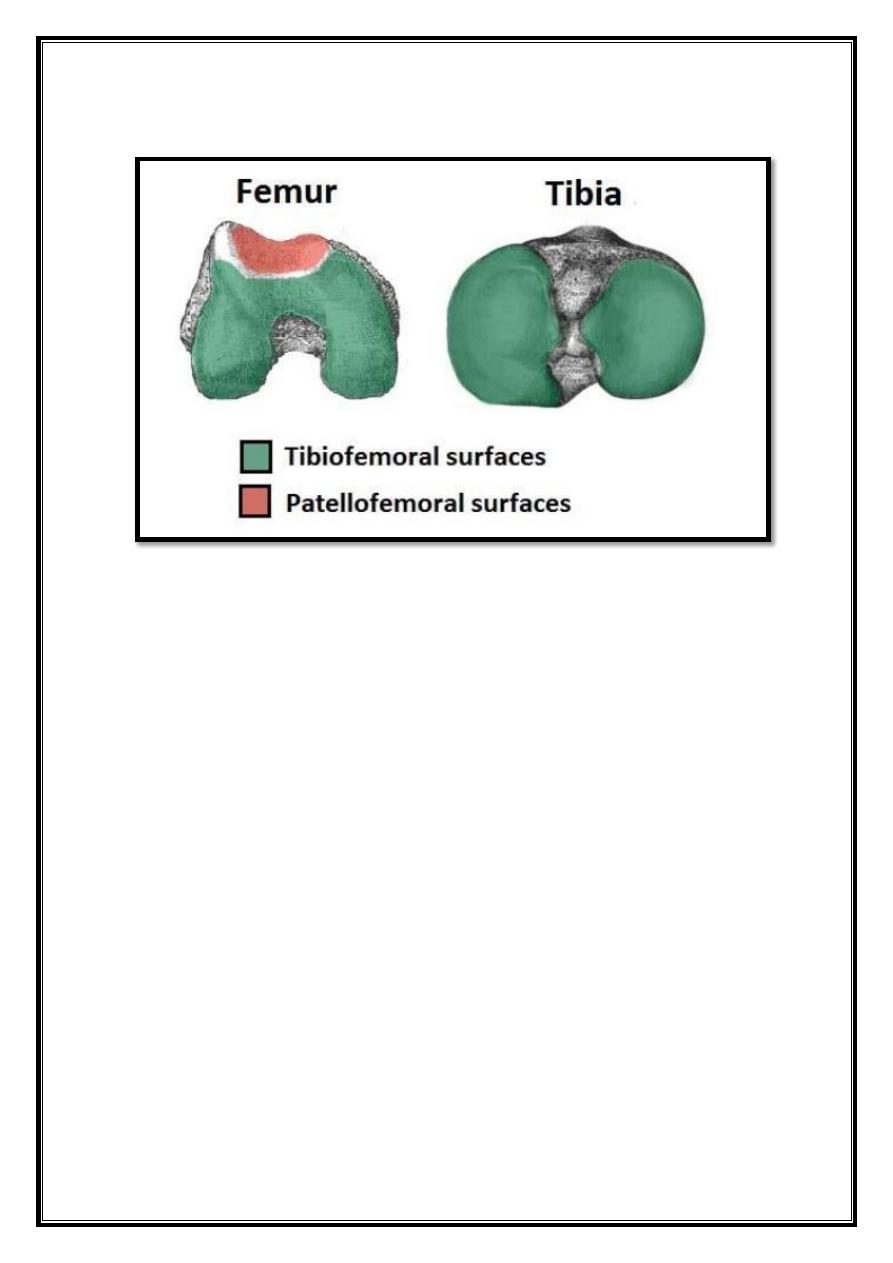
Articulating Surfaces
Fig 19 – More detailed view of the bony surfaces. The inferior surface
of the femur and superior surface of the tibia is shown.
The knee joint consists of two articulations:
Tibiofemoral
– medial and lateral condyles of the femur articulating with the
tibial condyles.
Patellofemoral
– anterior aspect of the distal femur articulating with the patella.
The tibiofemoral joint is the weight-bearing joint of the knee.
The patellofemoral joint allows the tendon of the
quadriceps femoris
(the main
extensor of the knee) to be inserted directly over the knee, increasing the
efficiency of the muscle.
As the patella is both formed and resides within the quadriceps femoris tendon, it
provides a fulcrum to increase power of the knee extensor, and serves as a
stabilizing structure that reduces frictional forces placed on femoral condyles.
Both joint surfaces are lined with hyaline cartilage, and enclosed within a single
joint cavity.
8
Neurovasculature
The blood supply to the knee joint is through the
genicular anastomoses
around
the knee, which are supplied by the genicular branches of the femoral and
popliteal arteries.
The nerve supply, according to Hilton’s law, is by the nerves which supply the
muscles which cross the joint. These are the
femoral, tibial and common
fibular
nerves.
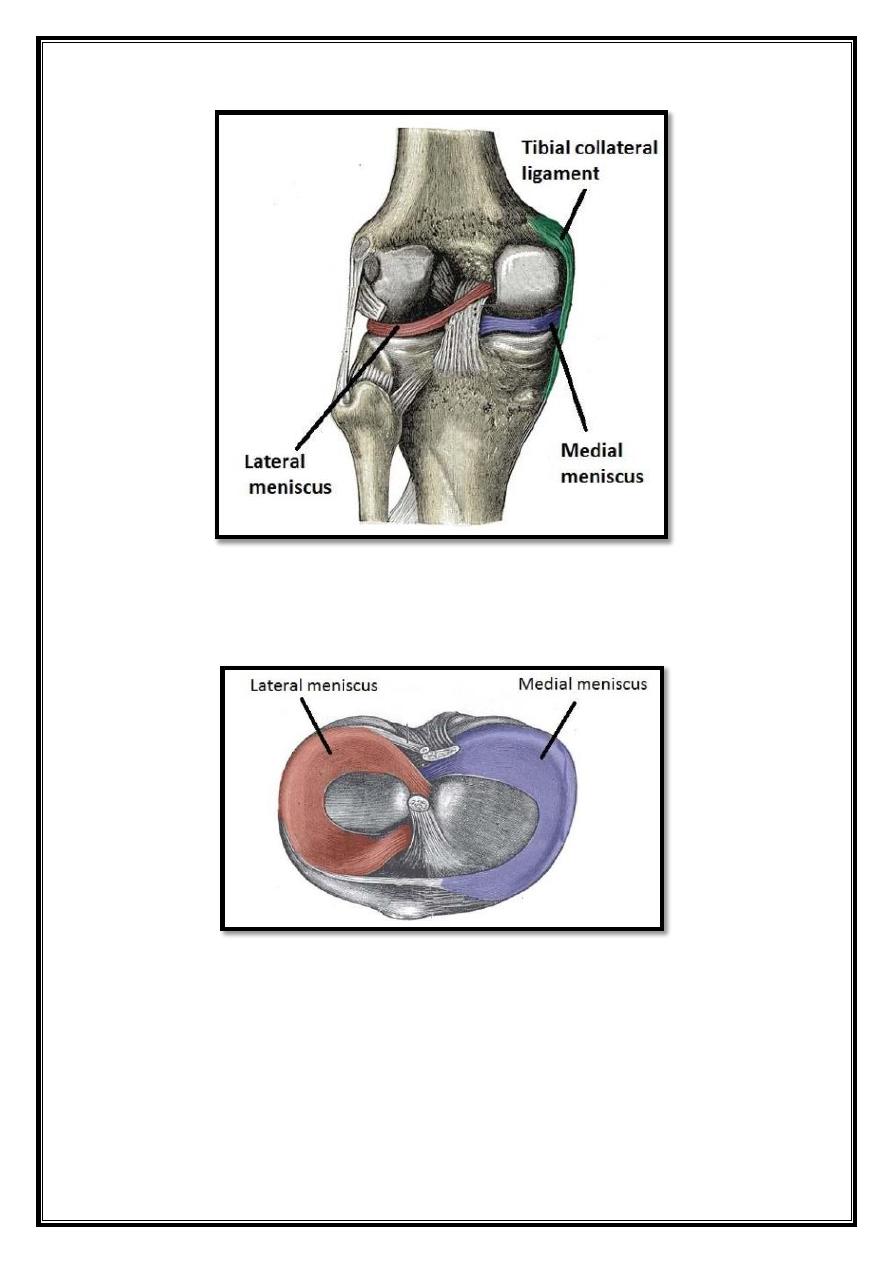
Menisci
The medial and lateral menisci are
fibrocartilage
structures in the knee that
serve two functions:
To deepen the articular surface of the tibia, thus increasing stability of
the joint.
To act as shock absorbers by increasing surface area to further
dissipate forces.
They are C shaped, and attached at both ends to the intercondylar area of the
tibia.
In addition to the intercondylar attachment, the medial meniscus is fixed to
the tibial collateral ligament and the joint capsule. Damage to the tibial
collateral ligament usually results in a medial meniscal tear.
The lateral meniscus is smaller and does not have any extra attachments,
rendering it fairly mobile
9
Fig 20 – Posterior view of the knee joint, with the joint capsule
removed. Note the close relationship of the tibial collateral ligament,
and the medial meniscus
Fig 21 – The menisci of the knee joint. Superior surface of the tibia
10
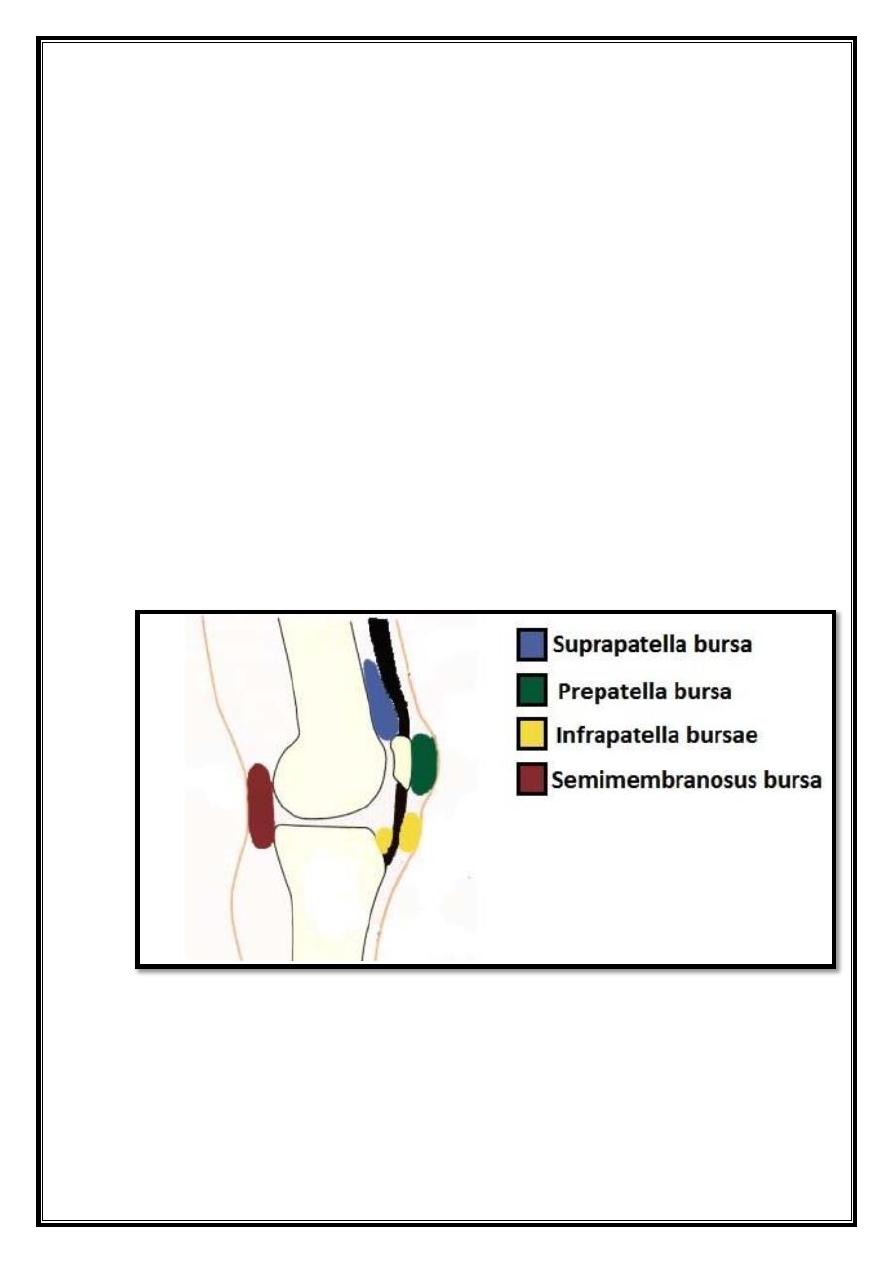
Bursae
A bursa is synovial fluid filled sac, found between moving structures in a
joint – with the
aim of reducing wear and tear on those structures. There are four bursae
found in the knee joint.
Suprapatella bursa
– This is an extension of the synovial cavity
of the knee, located between the quadriceps femoris and the femur.
Prepatella bursa
– Found between the apex of the patella and the
skin.
Infrapatella bursa
– Split into deep and superficial. The deep
bursa lies between the tibia and the patella ligament. The
superficial lies between the patella ligament and the skin.
Semimembranosus bursa
– Located posteriorly in the knee joint,
between the semimembranosus and the medial head of the
gastrocnemius.
Fig 22 – Sagittal view of the knee joint, showing the major bursae.
11
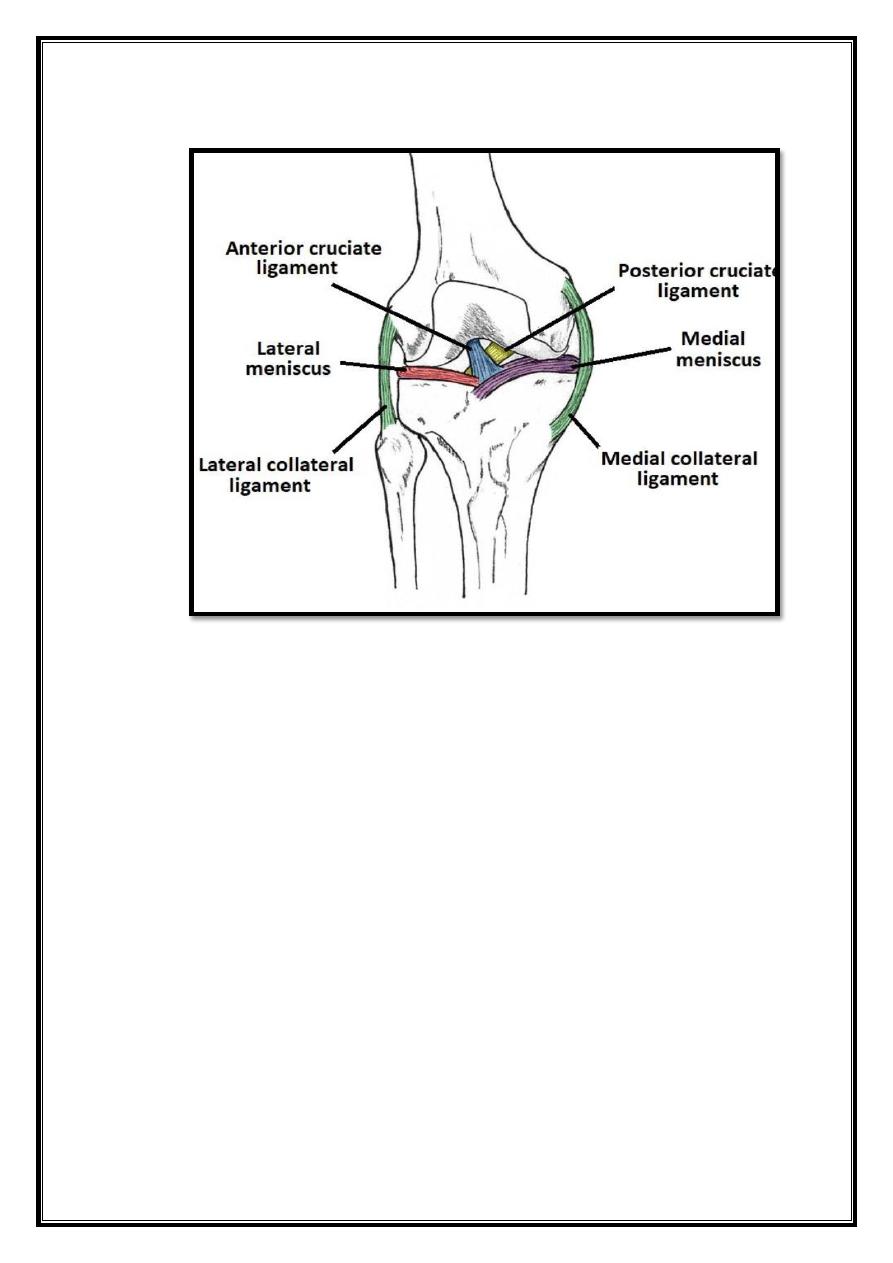
Ligaments
The major ligaments in the knee joint are:
Patellar ligament
– a continuation of the quadriceps femoris
tendon distal to the patella. It attaches to the tibial tuberosity.
Collateral ligaments
– two strap-like ligaments. They act to
stabilize the hinge motion of the knee, preventing excessive medial
or lateral movement
- Tibial (medial) collateral ligament – A wide and flat ligament,
found on the medial side of the joint. Proximally, it attaches to the
medial epicondyle of the femur, distally it attaches to the medial
condyle of the tibia.
- Fibular (lateral) collateral ligament – Thinner and rounder than the
tibial collateral, this attaches proximally to the lateral epicondyle of
the femur, distally it attaches to a depression on the lateral surface
of the fibular head.
Cruciate Ligaments
– These two ligaments connect the femur and
the tibia. In doing so, they cross each other, hence the term
‘cruciate’ (Latin for like a cross).
- Anterior cruciate ligament– it attaches at the anterior intercondylar
region of the tibia where it blends with the medial meniscus. It
ascends posteriorly to attach to the femur in the intercondylar
fossa. It prevents anterior dislocation of the tibia onto the femur.
- Posterior cruciate ligament– attaches at the posterior intercondylar
region of the tibia, and ascends anteriorly to attach to
theanteromedial femoral condyle. It prevents posterior dislocation
of the tibia onto the femur.
12
-
Fig 23 – Anterior view of the knee joint, showing some of the major
ligaments. The patella ligament is situated on the anterior aspect of
the knee joint, and is not visible is this diagram.
Movements
There are four main movements that the knee joint permits:
Extension:
Produced by the quadriceps femoris, which inserts into
the tibial tuberosity.
Flexion:
Produced by the hamstrings, gracilis, sartorius and
popliteus.
Lateral rotation:
Produced by the biceps femoris.
Medial rotation:
Produced by five muscles; semimembranosus,
semitendinosus, gracilis, sartorius and popliteus.
13
NB: Lateral and medial rotation can only occur when the knee is
flexed (if the knee is not flexed, the medial/lateral rotation occurs at
the hip joint).
