I.
Proteinuria
II.Dr. Ali ALthabhawi
Protein uria
10% of children aged 8-12 years have
+ve test for Protienurea.
Ways of detection of Protienurea.
!1 - D i p s t i c k , q u a l i t a t i v e
assessment( albumin)
!trase (10-20mg/dl)
!+=30
!++(100)
!+++=(300)
!++++=1000-2000mg/dl.
2-Timed 12-24H urine collection for protein
Normally 150mg/day, or 4mg/m2/day
Abnormal=4-40mg/m2/hr
Nephrotic range more than 3.5g/day or more
than 40mg/m2/hr
3- URINARY PROTIE/ URINARY CREATINNE
(upro/ucre)
Normally less than 0.5 in child less than 2year
and less than 0.2 in child more than 2year
More than
2
suggest nephrotic range.

Transient Proteinuria
Approximately 10% of children who undergo random
urinalysis have proteinuria by a single dipstick
measurement, serial testing of the patient's
urine demonstrates resolution of the abnormality.
Defined contributing factors include a temperature >
38.3°C, exercise, dehydration, cold exposure, heart
failure, recent use of epinephrine, seizures, or stress.
Transient proteinuria usually does not exceed 1-2+ on
the dipstick. No evaluation or therapy is needed

Orthostatic (Postural) Proteinuria
Orthostatic proteinuria is the most common
cause of persistent proteinuria in school-age
children and adolescents, occurring in up to
60% of children with persistent proteinuria.
Children with this condition are asymptomatic,
and the conditionis discovered by routine
urinalysis.
Patients with orthostatic proteinuria
excrete normal or minimally increased
amounts of protein in the supine position.
In the upright position, urinary protein
excretion may be increased 10-fold, up to
1,000 mg/24 hr (1 g/24 hr).
Hematuria, hypertension,
hypoalbuminemia, edema, and renal
dysfunction are absent

Nephrotic synrome
2-3/100000
Disease of children (15 fold than adult)
! p r o t e i n u r i a a b o v e 4 0 m g / m ² / h r ( o r
1 g / k g / 2 4 h r ) o r u r i n a r y p r o t e i n
(mg/dl)/creatinine(mg/dl)more than 2
! Hypoalbuminamia(serum albumin <
2.5g/dl
! Oedema
! Hypercholesterolemia(serum cholesterol
> 200mg/dl,5.25mmol/l
The primary abnormality is protein urea .
Others features are secondary
" H y p o c a l c a e m i a ( i o n i z e d f r a c t i o n
normal),below 9.0mg/dl
" Hyponatremia(below 135mmol/l
" Hypercoagulabity
Etiology
90% Idiopathic( MCNS, related to
g l o m e r u l a r d i s e a s e s l i k e
m e m b r a n o u s n e p h r o p a t h y ,
membranoprolefretive)
10%secondary(systemic diseases
s u c h a s s y s t e m i c l u p u s
erythematosus, Henoch-Schonlein
purpura, malignancy (lymphoma and
leukemia), and infections (hepatitis,
HIV, and malaria)
Idiopathic nephrotic syndrome
8 5 % m i n i m a l c h a n g e d i s e a s e n e p h r o t i c
syndrome(MCNS)
"Most common type (due to circulating lymphokine).
"proliferation of a T- cell subclass.
"MCNS characteristically shows fusion of epithelial
foot process on electron microscopy
"95%steroid responder
10%Focal segmental G.sclerosis .
!Mesangial proliferation, increase in matrices, and
segmental sclerosis.
!20% steroid responder .
!May lead to end stage renal failure
5%Mesangial proliferative .
#Deffuse mesangial l cell proliferation, increase in
matrice.
# 50% steroid responder
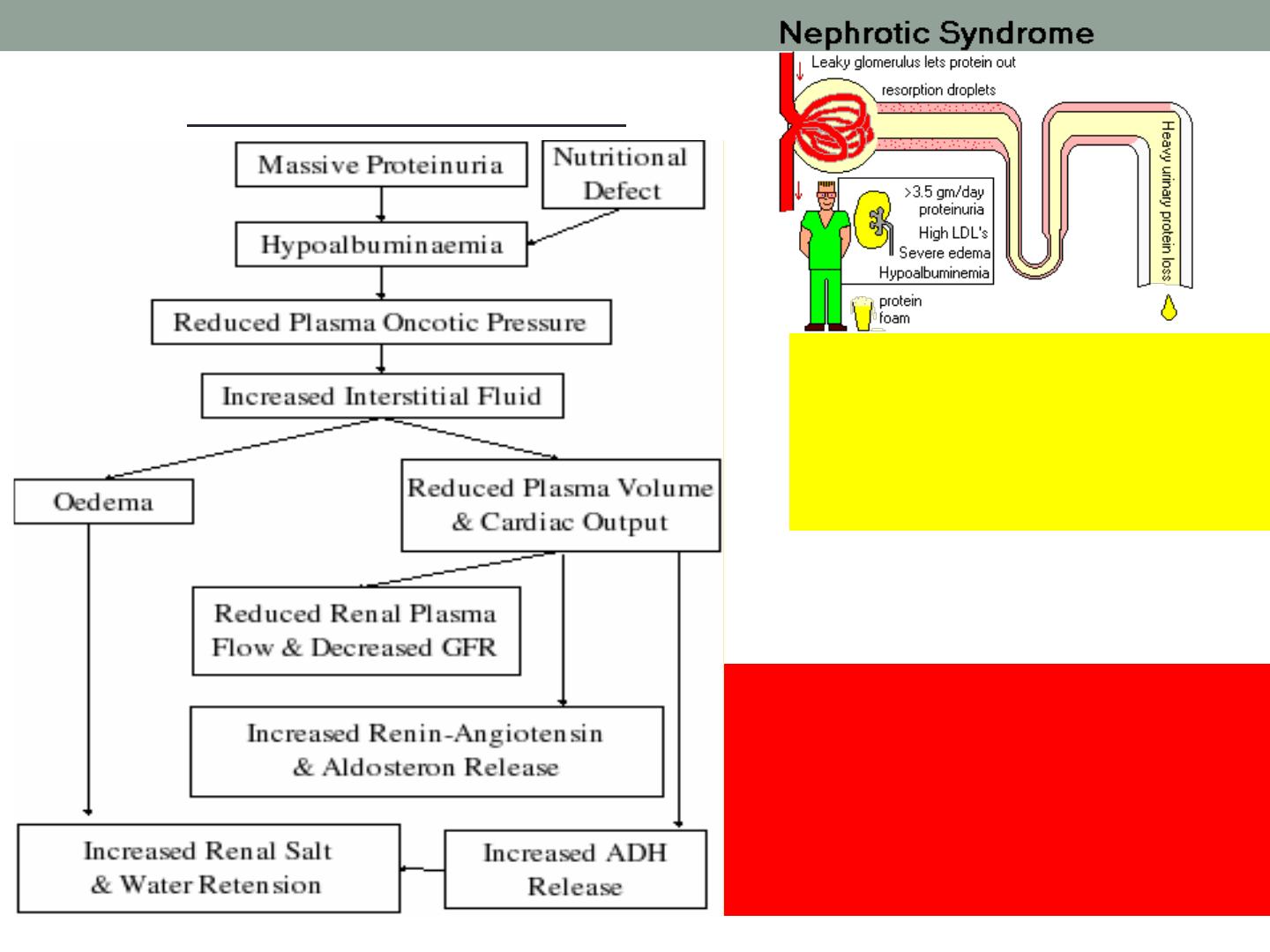
Pathophysiology
I n c r e a s e
p e r m e a b i l i t y o f
g l o m e r u l a r
capillary wall lead
to massive protein
u r e a a n d
hypoalbuminemia.
$Hyperlipidemia (cholesterol and
trigyceride) is due to
! Hypoalbuminamia may stimulate
hepatic synthesis of lipoprotein
! loss of lipoprotein lipase in urine
w h i c h i s r e s p o n s i b l e f o r
degradation of lipoptotien.
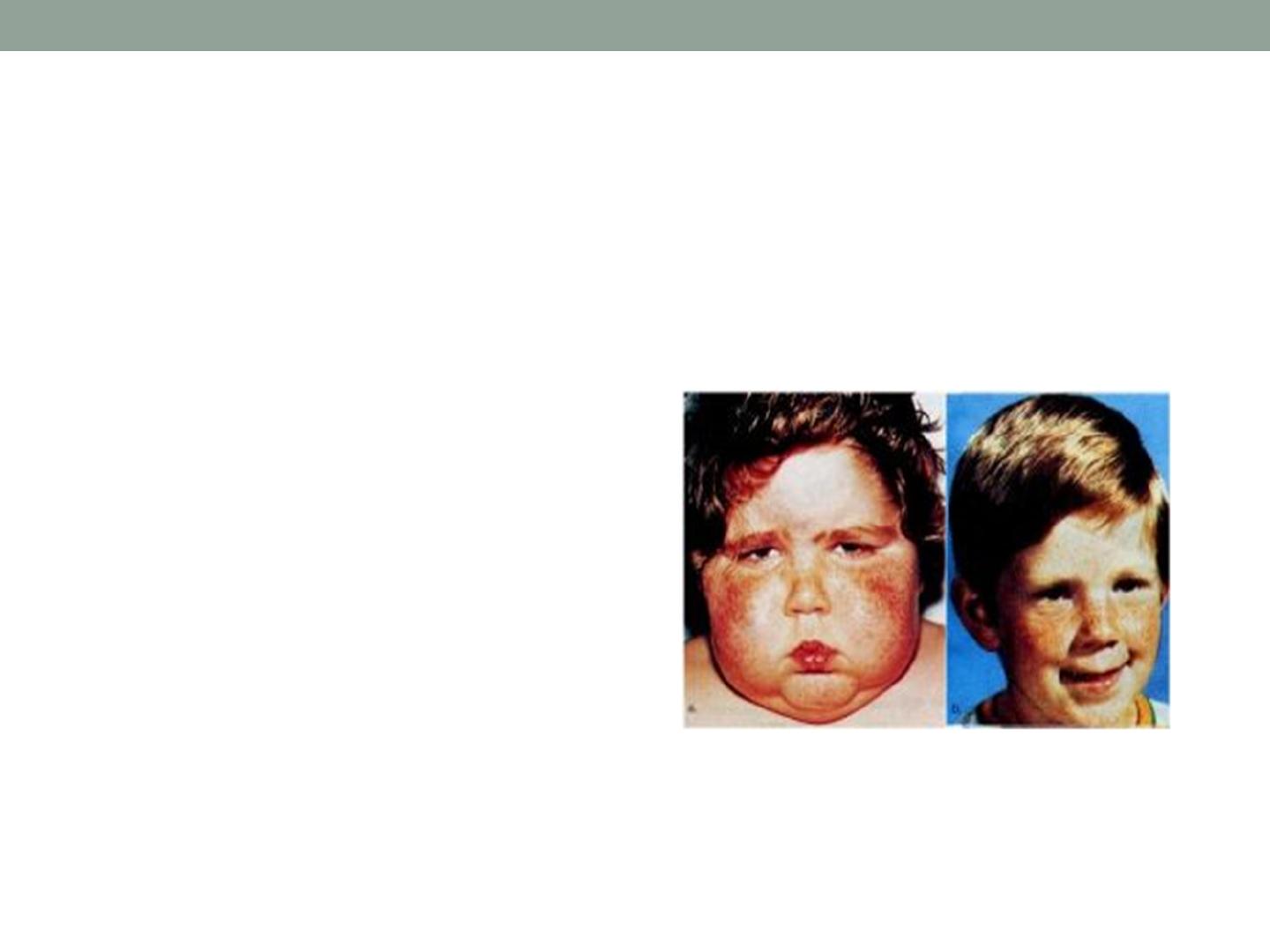
Minimal change disease nephrotic
syndrome(MCNS)
$
Clinical feature
!
Most common (2-6),rarely <6months.
!
The initial episode and subsequent relapse may flow minor
infection, occasionally related to insect bite.
!
Mild edema noted around the eye and then to lower
extremity ,may be misdiagnosed as allergic disorders. with
time edema become generalized with ascites, pleural
effusion and genital edema
!
Anorexia, irritability, abdominal pain, diarrhea are
common
!
Hypertension and grosse hematuria are uncommon
$
D.DX
$
Hepatic failure, congestive heart failure, acute or chronic GN,
protein malnutrition , protein loosing enteropathy
Diagnosis
URINE
!
Protein in urine 3+ or 4+or proteinuria
above40mg/m²/hr (1g/kg/24hr)or urinary
protein(mg/dl)/creatinine(mg/dl) ratio of 2.0 or
more
!
Cellular cast which do not to occur in INS but
m a y w e l l o c c u r i n o t h e r
glomerlonephropathies(note that halyine or
waxy casts are common in INS
!
Micro .RBC in 10-20%.
BLOOD
"
Urea , creatinin and electrolytes(renal function usually
normal in INS(10-20%increase in BUN); may be
abnormal in other glomerlonephropathies
"
Albumin(less than2.5g/dl) and total serum protein was
low
"
Increase Serum cholesterol and triglyceride
"
Serum complement level C3,C4(low with mesangial
proliferative ,SLE., normal in INS)
"
Hepatitis B and C serology (Hep B is associated with
membranous nephritis, Hep C is associated with
mesangial proliferative.
"
Anti-nuculer antibody(ANA), Anti-double stranded .
RENAL BIOPSY
Children with features that make
MCNS less likely :
!
Gross hematuria.
!
Hypertension.
!
Renal insufficiency.
Hypocomplementemia.
!
Age <1 yr
or >12 yr
Definitions
"
Remission=urinary protein excretion less than
4mg/ m²/hour or trace of protein in urine dipstick, or
urinary protein (mg/dl)/creatinine(mg/dl)ratio of0.2
mg/dl for 3 consecutive days
"
Relapse=recurrence of proteinurea defined in INS
3-4+dipstick +edema.
"
Frequent relapse= 2 or more relapse in the first
6months of initial response OR more than 4
relapse in 12months
"
Corticosteroid dependence=2 consecutive
relapse while on steroid (every other day) or within
2 weeks of ceasing steroid
"
Corticosteroid resistance =failed response after
8weeks of 2mg/kg/day
Treatmen
t
Diuretics
!
Mild to moderate edema may be managed as
outpatients , low-sodium diet , oral diuretics????
!
severe symptomatic edema, including large pleural
effusions, ascites, or severe genital edema, should be
hospitalized. In addition to sodium restriction, fluid
r e s t r i c t i o n m a y b e n e c e s s a r y i f t h e c h i l d i s
hyponatremic
!
Swollen scrotum may be elevated with pillows to
enhance the removal of fluid by gravity.
!
Diuresis may be augmented by administration of
furosemide (1–2 mg/kg/dose IV q 12 hr).
Albumin
IV administration of 25% human
albumin (0.5 g/kg/dose q 6–12
hr administered over 1–2 hr)
followed by furosemide (1–2
m g / k g / d o s e I V ) i s o f t e n
necessary when fluid restriction
and parenteral diuretics are not
effective
Symptomatic volume overload,
with hypertension and heart
f a i l u r e , i s a p o t e n t i a l
c o m p l i c a t i o n o f p a r e n t e r a l
albumin therapy, particularly
with rapid infusions
.
PREDISOLON
60 mg/m
2
/day (2mg/kg)(maximum
daily dose, 80 mg) in a single daily
dose for 4-6 consecutive wk( low
relapse). About 80-90% of children
respond to steroid therapy (clinical
remission, diuresis, and urine
trace or negative for protein for 3
consecutive days) within 3 wk.
Then, the prednisone dose should be tapered
to 40 mg/m
2
/day(1.5mg/kg) given every other
day as a single daily dose for at least 4 wk.
The alternate-day dose is then slowly
tapered and discontinued over the next 1-
2 months (5mg /week).
(increase dose. Long duration =decrease
relapse 60-80% in past, now 30-40% )
The side effects of prolonged corticosteroid
administration must be kept in mind.

Treatment of relapse
Relapses should be treated with
60 mg/m
2
/day (80 mg daily max) in a
single(8.0 am) dose until the child
enters remission (urine trace or
negative for protein for 3 consecutive
days). The prednisone dose is then
changed to alternate-day dosing as
noted with initial therapy, and gradually
tapered over 4-8 wk.
Other agents, cytotoxic drugs(CLAIM
)
C
cyclophosphamide(CPA:2-3mg/kg for 8-
12weeks),Chlorambucil 0.2mg/kg for 8-12 weeks),
Cyclosporine(CSA:2.5mg/kg12hourly for 12months
L
levamisole(2.5mg/kg daily for 6-12 months)
A
angiotensin-converting enzyme ACE inhibitors
I
immunization with pnuemoccocal vaccine
M
mycopgenolate mofetil 25mg/kg /day for 1year
CPA has significant side effect ,short term=bone
morrow suppretion.risk of viral infections such as
varicella,measles)long term (gonadal toxicity and
risk of malignancy)
C A S c a n c a u s e n e p h r o t o x i c o t y ,
hypertention,gingival hypertrophy and hirsutism

$A L L t h e a b o v e m e d i c a t i o n s a r e
indicated in the following
! Steroid resistant type
! Steroid dependent type(only if side
effect are unacceptable)
! Frequent relapse with hypertension
or thrombosis
! U n a c c e p t a b l e s t e r o i d s i d e
effect(weight gain, cushnoid facies
Antibiotics
Some unite treat all episodes of relapse
with prophylactic daily penicillin to ovoid
pnuemoccocal infection. Others not,
s o m e u s e t h i r d g e n e r a t i o n
cephalosporin ,however the use of
prophylactic antibiotic during relapse
remain controversial
Immunization
Live viral vaccine should be avoided in patient
taking steroid or other immune suppressive drug.
pnuemoccocal vaccine is recommended and
annual influenza vaccine.
Hypertension
"
Minority, treated by nifedipine and beta blocker
Diet
"
No added salt, no fluid restriction unless in very
edematous and diuretics is required ,high
biological value protein.
In hospital management
"
Fluid balance chart, twice daily weight, 4-horly chart
of vital sings.
Activity
"
No need for bed rest or restriction of activity.
Complications of NS
1- Infection
! Encapsulated bacteria(pnuemoccocal, haemphilus ) is
spontaneous bacterial peritonitis (SBP) , cellulites,
UTI,pneumonia due to many factors
! urinary loss of immunoglobulin
! loss of B factor of alternate activation path.
! loss of transferring
! Alter T- cell function
! Steroid and other immune suppressive therapy
! Mechanical factors such as edema and ascitis
! Malnutrition
! occurrence of (SBP)is 2-6%and The this risk is further
increased by decrease mesenteric blood flow and
increase coagulability causing micro infarction
! The (SBP) need high index of suspicion because the
clinical signs some times are masked by the steroid
(blood culture, peritoneal fluid culture then prompt
antibiotic)
2- Thromboembolism
!
NS associated with Hypercoagulabity (2-
5%) state due to
!
D u e t o i n c r e a s e p r o t h r o m b o t i c
activity(fibrinogen, thrombocytosis,
h a e m o c o n c e t r a t i o n a n d r e l a t i v e
immobilization ) and decrease fibrnolytic
factor(loss of antithombin III, and protien C,
S),
prophylactic anticoagulant not
r e c o m m e n d e d u n l e s s t h e y h a v e
previous thromboembolic event.
!
Over use of diuretics, and use of indwelling
catheter should be restricted.
3- Other complications
Site effect of drugs
(steroid),
(cytotoxic drugs
)
Prognosis
"
Majority of child with steroid responsive NS
had repeated relapse with time, decrease
relapse specially if not getting relapse in
the 1st 6months
"
steroid responsive NS not lead to
chronic renal failure, and not hereditary,
normal sterility in absence of prolonged
use of cyclophosphomide)
"
child during remission no need for testing
of Protienurea.
"
Steroid resistant NS poor prognosis
end stage renal failure dialysis and
renal transplant(30-50% getting the same
disease)
Secondary NS
10%
1-drugs(pencillamine, gold
2- membranoprolefretive NS
3-PSGN, LOPUS, HSP
4- infection malaria, Hepatitis
B,C, HIV
5- Malignancy H. lymphoma.
Congenital NS
!
In the 1st 3month most common type
!
Finnish type autosomal recessive ,increase alpha
feta protein, large placenta, marked edema,
prematurely, RDA, separation of cranial suture
!
Lead to end stage renal disease, no value of
steroid or cytotoxic
!
A C E i n h i b i t o r, e n d o m e t h a c i n e , u n i l a t e r a l
nephrectomy
!
Other form is due to infection(TORCH).
