Multiple sclerosis
MS is not a common disease in Iraqi population but it is one of the burden on western countries .It is more common in the north of Iraq .
• MS is an inflammatory disease of the Central Nervous System (CNS) Predominantly affects the white matter tissue, which is responsible for transmitting communication signals both internally within the CNS and the nerves supplying the rest of the body.
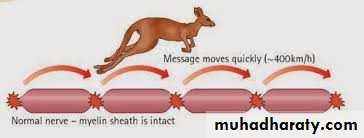
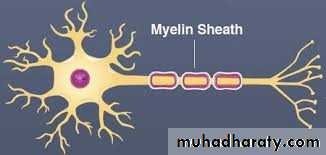
Surrounding and protecting the nerve fibers of the CNS is a fatty tissue called myelin, which helps nerve fibers conduct electrical impulses.
In MS, myelin is lost in multiple areas leaving scar tissue known as plaques or lesions.
Sometimes (not usual) the nerve fiber itself is damaged or broken Common cause of disability in young adults .
Pathogenesis:
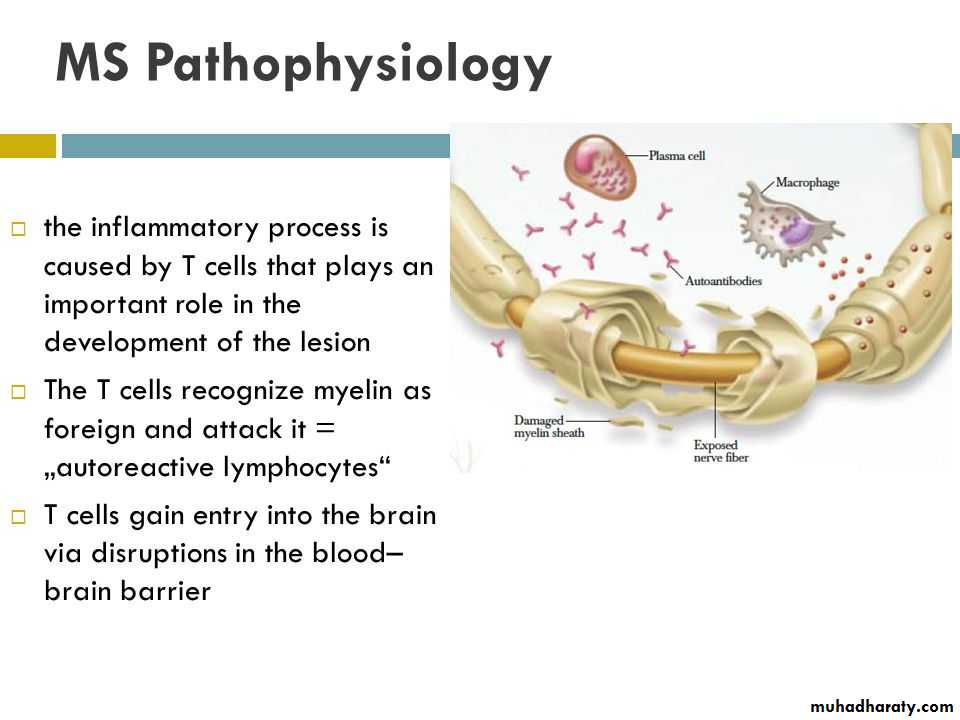
MS is an inflammatory process and Autoimmune mechanism play a major role in pathogenesis ,in which there is an abnormality due to abnormal function of macrophage,B-Cel1sandT- lymphocytes .Effect of demyelination and axonal damage.
Loss of myelin and axonal damage may lead to:Conduction block at the site of myelin or axonal loss
Slowed motor and sensory impulses in areas of disease activity, resulting in compromised sensation or movement .
Increased subjective fatigue (greater energy consumption)
pathophysiology
Both genetic and environment.Low near the equator and increase in temperate climate
Sunlight, Vitamin D,EBV
Familial 15%, monozygotic twins 30%
Polygenic
Immunological-T lymphocyte in CSF and increase immunoglobulin synthesis in CNS
Demographical factor
AgeOnset: 15 to 50 years of age (adult)
Peak onset: between 20 and 30 years of age
Onset rare before age 10 or after age 60
Gender
More Common in females
3: I female versus male
Race
Incidence higher in Caucasians
• Genetic factors
First- and second-degree relatives are at increased risk
Initial symptom
Double vision / blurred vision
Numbness/weakness in extremities
Instability while walking (ataxia)
Problems with bladder control
Heat intolerance
Note
All symptoms can be precipitated by heat (e.g. "after hot bath the patient complains of blurring of vision)
Sensory disturbance
Ascending numbness starting in feetBilateral hand numbness
Hemiparesthesia/dysesthesia
Generalized heat intolerance
Dorsal column signs
Loss of vibration or proprioception
Lhermitte's sign (on flexion of the neck feeling of electric activity passes between shoulders and arms sometimes to the legs)
Motor disturbance
Weakness (mono-, Para-, hemi- or quadraparesis)Increased spasticity
Dysarthria
Pathologic signs (Babinski, Chaddock and Hoffman)
(Chaddock sign: in lesions of the pyramidal tract, stimulation below the external malleolus causes extension of the great toe)
Visual disturbance
Unilateral or bilateral partial/complete internuclear ophthalmoplegia
Bilateral INO is highly suggestive of MS
CN VI paresis
Optic neuritis: (central scotoma, headache, change in color perception, retro orbital pain with eye movement)
We should differentiate between demyelinating optic neuritis due to MS from ischemic optic neuritis due to ischemia in elderly, HT, DM and IHD.
Ischemic papillitis usually causes sudden painless loss of vision, so if an elderly patient with sudden painless loss of vision in which there is attitudinal loss of vision, is highly suggestive of ischemic papillitis rather than demyelinating optic neuritis.
Cerebellar signs
NystagmusDysarthria
Tremor
Dysmetria
Titubation
Stance and gait
Common presenting symptom.
Optic neuritisRelapsing and remitting sensory symptoms
Subacute painless spinal cord lesion
Acute brain-stem syndrome
Subacute loss of function of upper limb (dorsal column deficit)
6th cranial nerve palsy
Afferent pupillary defect and optic atrophy (previous optic neuritis)
Lhermitte's symptom (tingling in spine or limbs on neck flexion)
Progressive non-compressive paraparesis
Partial Brown-Séquard syndrome
Internuclear ophthalmoplegia with ataxia
Postural ('rubral', 'Holmes') tremor
Trigeminal neuralgia under the age of 50
Recurrent facial palsy
Investigations
Demonstrate other sites of involvementImaging (MRI)
Visual evoked potentials
Other evoked potentials
Demonstrate inflammatory nature of lesion(s)
CSF examination
Cell count
Protein electrophoresis (Oligoclonal bands)
• Exclude other conditions
Chest X-ray
Serum angiotensin-converting enzyme (ACE)-sarcoidosis
Serum B12
Antinuclear antibodies-SLE
Antiphospholipid antibodies
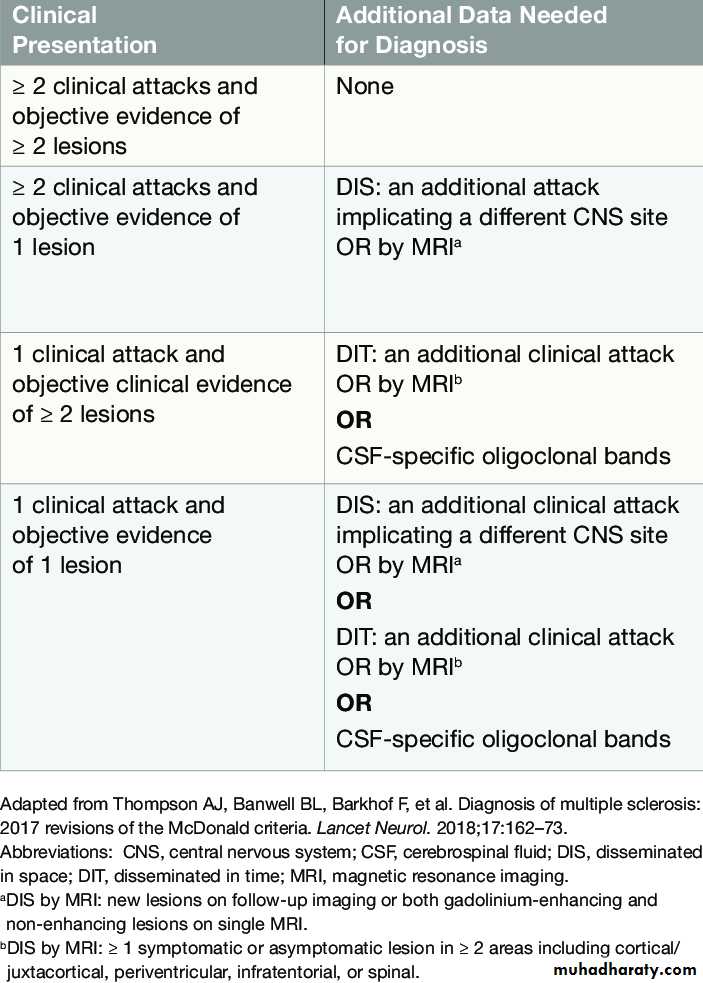
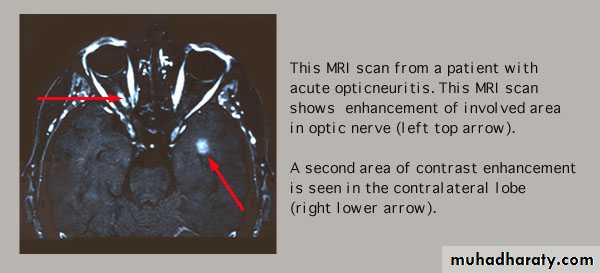
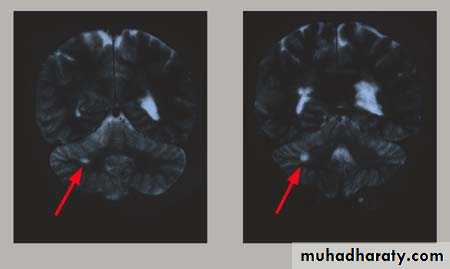
MRI FINDINGS
Patchy areas of white matter in paraventricular cerebral areasLesions in cerebellum/brainstem/ cervical and thoracic spinal cord
Gadolinium enhancement identifies active lesions
ABNORMAL MRI—OPTIC NERVE
ABNORMAL MRI--CEREBELLUM
CSF
Increased immunoglobulin concentration in >90% of patients.IgG index (CSF/serum) elevated
Oligoclonal bands—85%
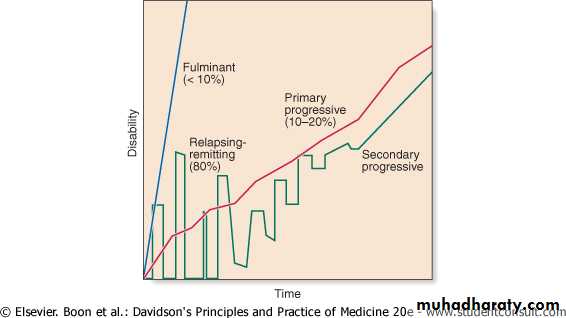
What is an Exacerbation?
Neurological attacks or aggravation of symptomsIndicative of a new immune attack on myelin
Should last at least 24 hours
Untreated attacks can last from weeks to months (resulting in slow recovery/residual effects)
Precipitating factors can be identified .
Precipitating Factors for Exacerbations could be:
Fever (most common), infections especially urinary tract infections without fever
Heat sensitivity
Emotional stress
Physical exertion
Fatigue
Treatment: the goal of Rx
Reduce (control) relapsesDelay disease progression
Delay disability
Alleviate symptoms
• Current therapy
Corticosteroids (in acute attack)
• Used in acute attack to hasten clinical recovery
• Methylprednisolone 1 gm\kg for 3-5 days
• Immunosuppressant and Immunomodulators
Interferon-beta ---Immune modulation --- widespread use for reducing relapse rate (RCT evidence).Glatiramer acetate --Immune modulation --Similar efficacy to interferon-beta (RCT evidence) .
Fingolimod --Immune modulation --Superior efficacy to interferon-beta in RCTs .
Monoclonal antibody to alpha4-integrin (natalizumab) --Immune modulation, Possibly more effective than other drugs.
Teriflunomide (AUBAGO).
Dimethyl fumarate (Tecfidera ).
Symptomatic therapy
Spasticity-physiotherpy,baclofen,tizanidine,benzodiazepine,dantrolen,Botulinm toxin type AFatigue- amantadine, Modafinil,SSRIs
Depression –SSRIs,TAD
Anxaiety-alprazolam
Ataxia –isoniazid, clonazepam
Dysthesia-carbamazepine,gabapentin
ACUTE DISSEMINATEDENCEPHALOMYELITIS
This is an acute, usually monophasic, demyelinating condition in which there are areas of demyelination widely disseminated throughout the brain and spinal cord.The disease occurs spontaneously .
May occurs a week or so after a viral infection, especially measles and chickenpox, or following vaccination, suggesting that it is immunologically mediated.
Clinical features
Headache, vomiting, pyrexia, confusion and meningism may be presenting features, often with focal or multifocal brain and spinal cord signs. Seizures or coma may occur.Investigations
MRI shows multiple high-signal areas in a pattern similar to that of multiple sclerosis, although often with larger areas of abnormality. The CSF may be normal or show an increase in protein and lymphocytes.
Management
The disease may be fatal in the acute stages but is otherwise self-limiting. Treatment with high-dose intravenous methylprednisolone, using the same regimen as for a relapse of multiple sclerosis, is recommended.