L5 Diabetes in children
Diabetes mellitus in children (type 1 DM ): L5Definition :Common chronic metabolic disease characterized by hyperglycemia as a cardinal biochemical features .
04 أيار، 20
2Etiological classification of DM
1-Type 1 DM (beta cell destruction )• Immune mediate
• Idiopathic
2-type 2DM (insulin resistance &deficiency )
• Typical
• Atypical )
04 أيار، 20
3
3-enetic defect of beta cell
• Mody (maturity onset diabetes of young )
• Wolfram syndrome (DDMOD diabetes mellitus ,diabetes insipidus optic atrophy &deafness)
• Mitochondrial DNA mutation
04 أيار، 20
4• Thiamine responsiveness megaloplastic anemia with diabetes
4-drug or chemical induced• L-asparginase
• Anti rejection .cyclosporine …..
• Phenytoin
• Diazoxide
• Beta blockers
• α interferone
5- disease of exocrine pancreas
• Cystic fibrosis
• Trauma to pancreas
• Pancreatitis
6-infection (CMV ,Rubella .HUS)
7-genetic syndromes
• Prader willi syndrome
• Downs syndrome
• Turner syndrome
• Klinefelter syndrome
8-Gestational diabetes
9-Neonatal diabetes
• Transient
• Permanent
04 أيار، 20
5
• Type 1 diabetes mellitus :
Insulin dependent or juvenile diabetes characterized by low or absent level of endogenously produced insulin & by dependence on exogenous insulin ; insulin act on movement of glucose into cells to subdue hepatic glucose production & halt movement of fatty acid from periphery to liver
04 أيار، 20
6the natural history include 4 stages :
• Preclinical Beta cell autoimmunity with progressive defect of insulin production• Clinical diabetes
• Transient remission ,honeymoon period
• Established diabetes
04 أيار، 20
7Its account about 10 % of cases of diabetes affecting >10 million people in the world ,over all incidence of type 1 DM varies from 0.7/100 000 /year [in Pakistan to 40/100 000/year In Finland. Girls and boys are equally effected ,no apparent correlation with socioeconomic status .
04 أيار، 20
8Age incidence ,2 peak group 5-7 yrs and time of puberty .there is a familial clustering inT1DM with prevalence in sibling approaching 6% but in general population is 0.4%in US .
HLA system mostly associated with DR3/4-DQ2/8
04 أيار، 20
9
Natural history of diabetes involve some or all of the following stages :
• Initiation of autoimmunity• Preclinical of autoimmunity with progressive loss of beta cell function
• Onset of clinical disease
• Transient remission
• Established disease
• Development of complications
04 أيار، 20
10Influence of high insulin vs low insulin on some metabolic processes in liver, muscle &adipose tissues :
High plasma insulin(postprandial state )
Low plasma insulin (fast state )
Liver
Glucose uptake
Glycogen synthesis .lipogenesis
Absence of ketognesis
Glucose production
Glycogenolysis
Gluconeogenesis
Muscles
Glucose uptake
Glucose oxidation
Glycogen synthesis
Protein synthesis
Absence of glucose uptake
Fatty acid &ketone oxidation
Glycogenlysis
ProteolysisAdipose tissues
Glucose uptake
Lipid synthesis
Absence of glucose uptake
Lipolysis & fatty acid release
04 أيار، 20
11
Diagnosis
Impaired glucose toleranceDiabetes mellitus
Fasting glucose 100-125mg/dl
Or
2hrs plasma glucose during OGTT more or equal 140mg/dl but <200mg/dlSymptoms of diabetes +random plasma glucose more or equal to 200mg/dl
Or
Fasting (at least 8 hr )plasma glucose more or equal to 126mg/dl
or
2hrs plasma glucose during OGTT more or equal to 200mg/dl
Or HA1c >or equal to 6.5%
04 أيار، 20
12
DM should suspected in any child with polyuria & dehydration ,poor weight gain ,hyperglycemia ,glucosuria & ketonuria
Random serum sugar >200mg/dl with typical symptoms with or without ketonuria is diagnostic
04 أيار، 20
13
• Initial management of type1 DM
Most newly cases of DM are alert and able to eat and drink and can manage with subcutaneous insulin alone04 أيار، 20
14
iv fluid required if the child vomiting or dehydrated . intensive educational programme is needed for the parents and child to cover
• Basic understanding of pathophysiology ofDM
• Insulin injection technique &sites
• Diet , regular meal & snacks ,reduced refined CHO .healthy diet no >than 30% fat intake
04 أيار، 20
15• 4-match food intake with insulin &exercise
• 5-blood glucose monitoring
• 6-recognition and treatment of hypoglycemia
• 7-the psychological impact of lifelong condition with serious short & long term complications
04 أيار، 20
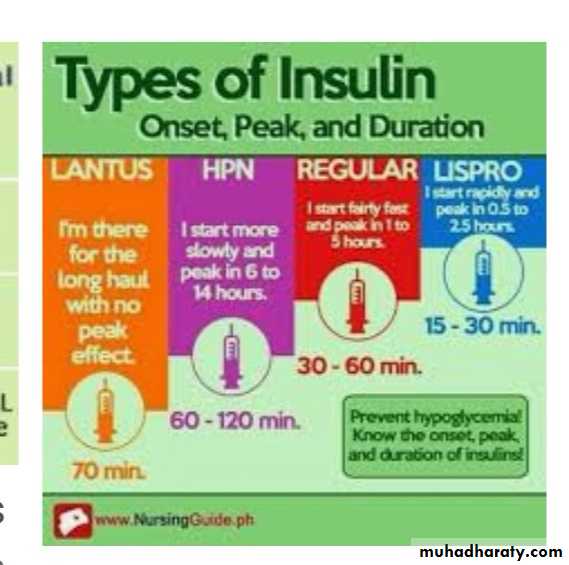
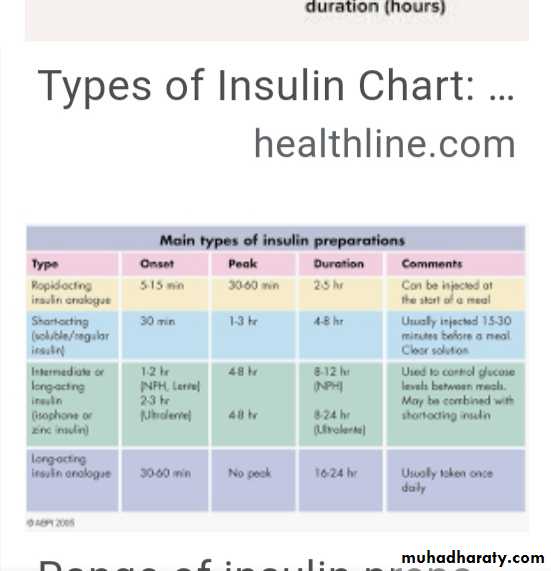
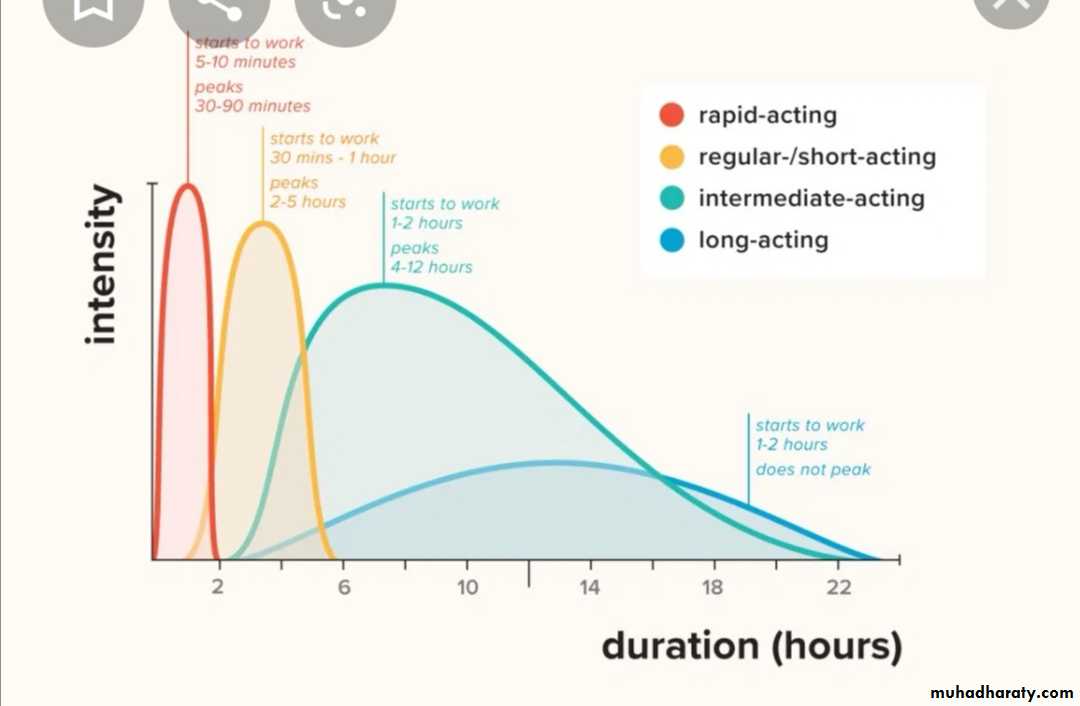
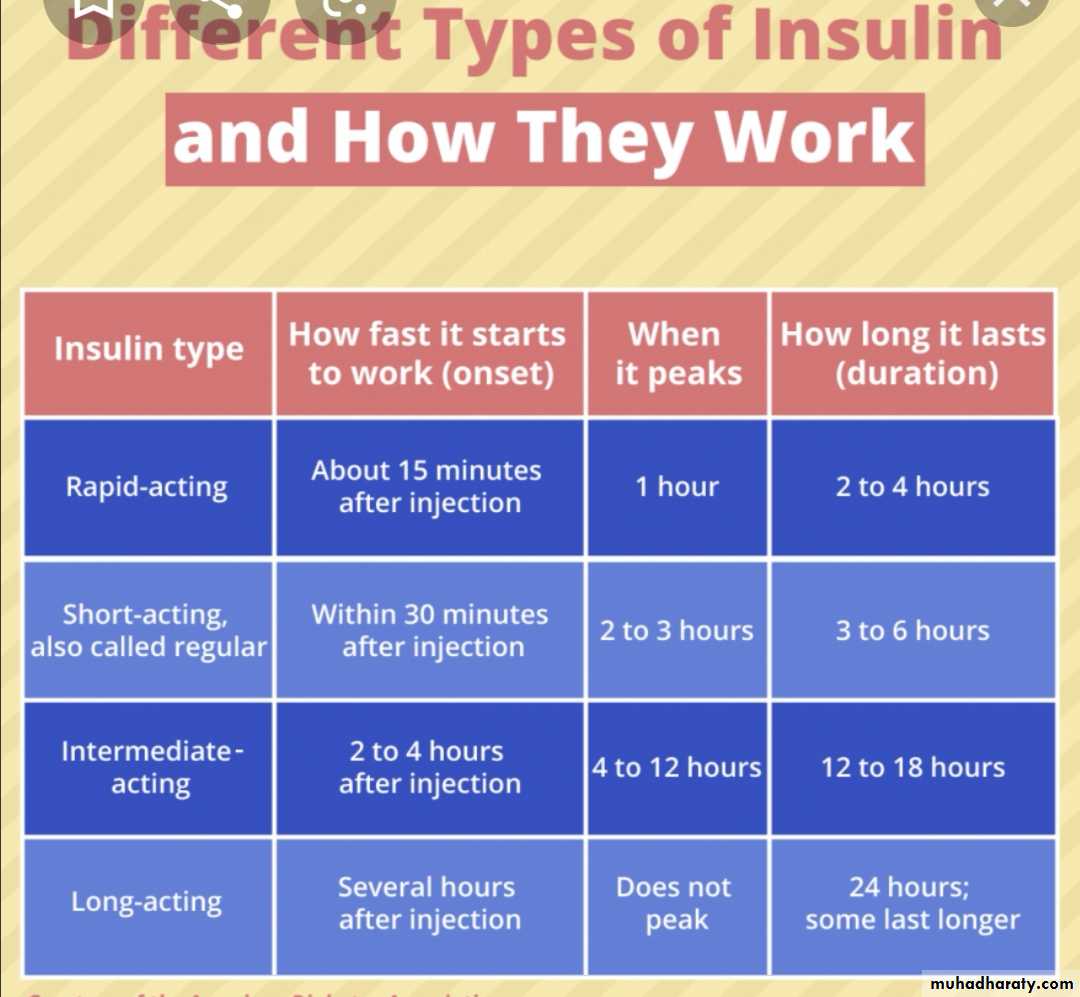
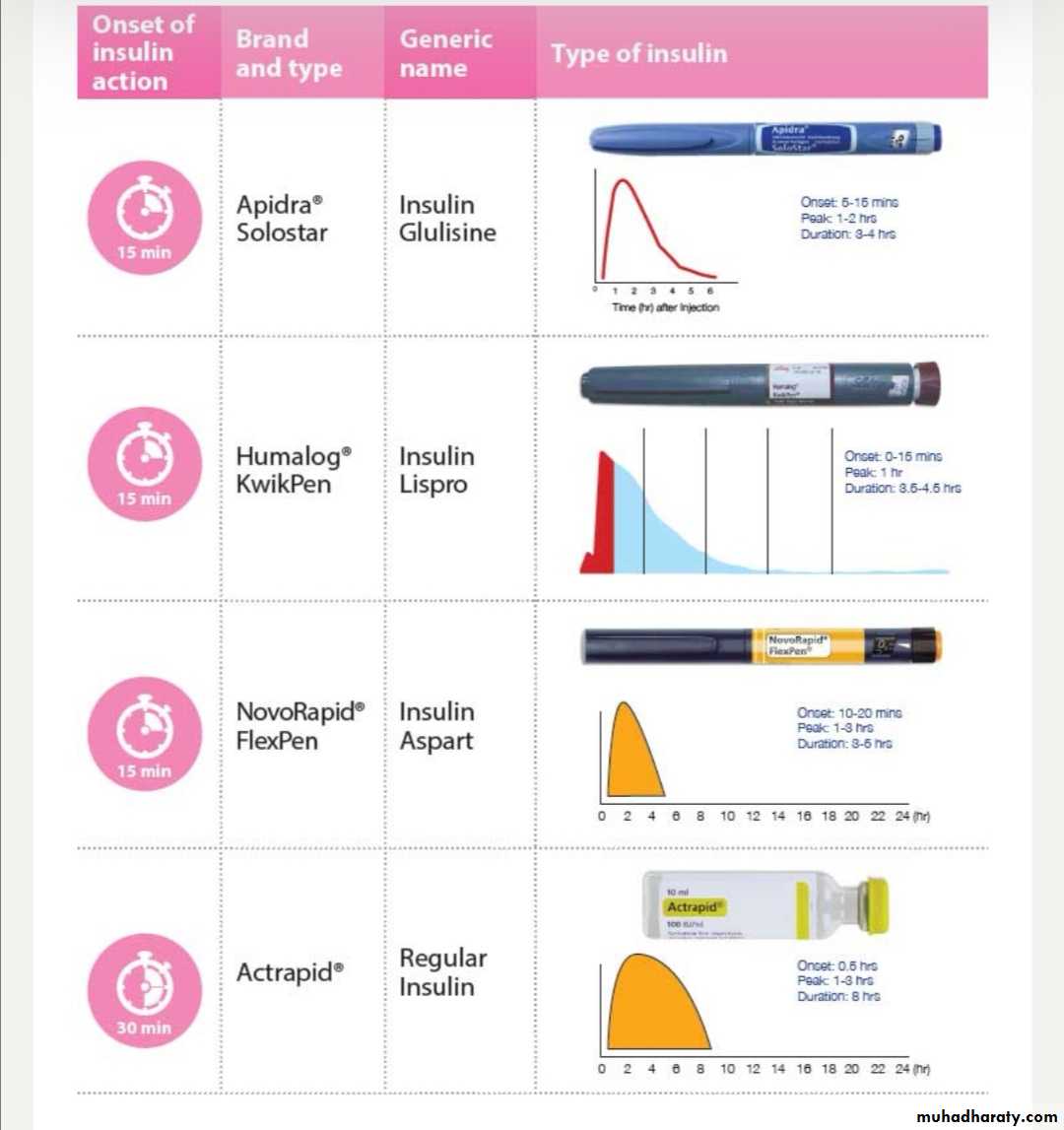
16• INSULIN THERAPY
• Most insulin used in Iraq for children is humen with concentration 100U/ml with different types includes• human insulin analogues . rapid acting like lispro &aspart within few minutes
• short acting soluble insulin onset 30-60 min. peak 2-4 hrs. duration up to 8 hrs. given 15-30 min.before meal
04 أيار، 20
17• intermediate acting insulin onset 1-2 hrs . peak 4-12 hrs( insulin with protamine )
• mixed short & intermediate 30/70 mixtard• very long acting insulin analogues e.g glargine (lantus)
teenager preferable to use bolus & basal (basal .lantus at night and short acting before each meal )
04 أيار، 20
18
04 أيار، 20
1904 أيار، 20
2004 أيار، 20
2104 أيار، 20
2204 أيار، 20
2304 أيار، 20
24Factors affecting blood glucose
Increase blood glucoseDecrease blood glucose
• omission of insulin
• refined food
• illness
• menstruation
• growth hormone
• corticosteroids
• sex hormones at puberty
• stress of an operation
• insulin
• exercise
• anxiety (marked )
• some drugs
•
04 أيار، 20
25
DIET : healthy diet recommended with high complex CHO &relatively low fat content ,diet should be high in fiber
04 أيار، 20
26• Diabetic ketoacidosis DKA :
End result of metabolic abnormalities result from sever deficiency of insulin or insulin ineffectiveness. It is occur in 20-40 % of children with newly diagnosed diabetes & DKA consider when serum sugar >300 mg .acidosis .+S/S of DM with ketosis .04 أيار، 20
27Classification of DKA
Normal
Mild
Moderate
Sever
Co2)meq/l venus
20-30
16-20
10-15
<10
pH venous
7.35-7.45
7.25-7.35
7.15-7.25
<7.15
Clinical
No changes
Only fatigue
Kussmaul ,oriented but sleepy
Kussmaul or depress respiration ,sleepy to coma
04 أيار، 20
28
Treatment
Time
Therapy
Comment
1st hr.
10-20ml/kg IV bolus 0.9%NaClor LR
Insulin drip at 0.05-0.1unit/lg/hr
Volume expansion ,NPO monitor I/O,use flow sheet prepare manitol 1g/kg at bed side if cerebral edema developed
2nd hr. until DKA resolution
0.45% Nacl plus continue insulin drip
20meq/l KPhos &20 meq/l K Ac….5%glucose if blood >250mg/dl
85ml/kg +maintenance -bolus
IV rate =
23 hr
If K <3meq give 0.5-1 meq as oral solution or increase iv K to 80meq/l
Maintenance =100ml/kg for 1st 10 kg+50ml/kg for 2nd 10 kg +25 ml/kg for remaining kg
Initial bolus fluid consider part of total fluid allowed & subtracted before calculating iv rate
04 أيار، 20
29Sample calculating for 30 kg child
1st hr 300 ml iv bolus 0.9% NaCl or LR
2nd & subsequent hrs= (85ml × 30)+1750ml -300ml =
23hr
= 175 ml
hrI/O input output, NPO nothing by mouth ,KAc potasium acetate ,kphos=potasium phosphate ….LR lactated Ringer..NaCl sodium chlodide
04 أيار، 20
30• Long term management of DM
Aim of long term management :• normal growth & development
• normal home & school life as possible
• good diabetic control through knowledge & technique
• encourage children to be self- reliant
• avoidance of hypoglycemia
04 أيار، 20
31Assesment of a child with DM summary
Assessment of diabetic control :
• any episode of hypoglycemia
• school absence
• interference with normal life
• HbA1C result
• Insulin regimen ---appropriate
• Diet –healthy diet
04 أيار، 20
32
General overview :
• Normal growth and pubertal development , ovoid obesity• Blood pressure checking
• Renal for microalbuminuria
• Eye ---cataract
• Feet –care
• Screening for celiac and thyroid disease
04 أيار، 20
33
Knowledge &psychological aspects
• Good understanding of diabetes
• Becoming self-reliant but appropriate supervision at home
• Taking exercise ,sport?
• Smoking ???
• Is hypo treatment readily available ?
•
04 أيار، 20
34
Ddiabetic lipohypertrophy
04 أيار، 2035
04 أيار، 20
36What shall I eat?
Breakfast
• a bowl of cereal with semi-skimmed milk
• wholegrain toast with spread and/or jam
• yogurt and fruit
• a cereal bar and a glass of milk.
04 أيار، 20
37Lunch
• a chicken or ham salad sandwich...• a small pasta salad...
• soup and a roll...
...with a piece of fruit and a yogurt.
04 أيار، 20
38Dinner
• salad• roast chicken with potatoes and
• vegetables
• beef stir fry, vegetables and rice
• chicken tortillas and salad
• salmon and noodles
• curry and rice
04 أيار، 20
39
• What sort of snacks do I need to eat?
.The healthiest snack choice is definitely a piece of fruit, but rice cakes, crackers, a couple of biscuits, a small bag of crisps, a cereal bar, or a yogurt are good snack choices too.
04 أيار، 20
40
• Foods to avoid for a type 1 diabetes diet include
sodas (both diet and regular),simple carbohydrates - processed/refined sugars (white bread, pastries, chips, cookies, pastas),
trans fats (anything with the word hydrogenated on the label), and high-fat animal products.