Major Complications (sequel) of Cirrhosis
Portal Hypertension
Portal hypertension is defined as the elevation of the portal venous pressure gradient (HVPG) to >5 mmHg. Portal hypertension is caused by a combination of two hemodynamic processes:(1) increased intrahepatic resistance to the passage of blood flow through the liver due to cirrhosis and regenerative nodules
(2) increased splanchnic blood flow secondary to vasodilation within the splanchnic vascular bed.
The causes of portal hypertension
1)- Prehepatic causes of portal hypertension are those affecting the portal venous system before it enters the liver; they include:-Portal vein thrombosis.
Splenic vein thrombosis.
Massive splenomegaly (Banti's syndrome).
2)-Posthepatic causes encompass those affecting the hepatic veins and venous drainage to the heart; they include:-
Budd-Chiari syndrome.
Inferior vena caval webs.
Cardiac causes.
Restrictive cardiomyopathy
Constrictive pericarditis.
Severe congestive heart failure.
3)- Intrahepatic causes account for over 95% of cases of portal hypertension and are represented by the major forms of cirrhosis. This further subdivided into:-
Postsinusoidal causes include venoocclusive disease,
presinusoidal causes include congenital hepatic fibrosis and schistosomiasis.
Sinusoidal causes are related to cirrhosis from various causes.
Cirrhosis is the most common cause of portal hypertension is present in >60% of patients .
Clinical Features of portal hypertension
The frequent presentations of patients with portal hypertension are:-gastroesophageal varices with or without hemorrhage,
rectal varices cause rectal bleeding often mistaken for hemorrhoids
ascites,
hypersplenism, enlarged spleen with associated reduction in platelets and white blood cells on routine laboratory testing
caput medusa .the collateral vessels visible on anterior abdominal wall radiate from the umbilicus
Esophageal Varices
The most important clinical feature of portal hypertension is variceal bleeding, which commonly arises from esophageal varices located within 3-5 cm of the esophago-gastric junction, or from gastric varices.. Drugs that causing mucosal erosion, such as salicylates and other drugs (NSAIDs), can also precipitate bleeding. approximately 15% of cirrhotic per year develop varices, and it is estimated that the majority (90%) of patients with cirrhosis will develop varices over their lifetimes and about one-third of patients with varices will develop bleedingThere are several factors predict the risk of bleeding, including
the severity of cirrhosis (Child's class,);the height of wedged-hepatic vein pressure;
the certain endoscopic stigmata, including size of the varix; the location of the varix; red wale signs, hematocystic spots, diffuse erythema, bluish color, cherr red spots, or white-nipple spots.
Patients with tense ascites are also at increased risk for bleeding from varices
Diagnosis
endoscopic examination of the upper gastrointestinal tract to determine whether gastro-oesophageal varices are present and estimated the grads of varices .This establishes the presence of portal hypertension but not its cause.Ultrasonography often shows features of portal hypertension, such as splenomegaly and collateral vessels, and can sometimes indicate the cause, such as liver disease or portal vein thrombosis.
CT and MRI angiography can identify the extent of portal vein clot and are used to identify hepatic vein patency
interventional radiologic procedures the calculation of a wedged-to-free gradient, which is equivalent to the portal pressure. The average normal wedged-to-free gradient is 5 mmHg, and patients with a gradient >12 mmHg are at risk for variceal hemorrhage.
Management of acute varicel bleebing
1)-general measures.By restore the circulation with blood and plasma because the shock state reduce liver blood flow and cause further deterioration of liver function.
2)-initial control of Variceal hemorrhage.
Endoscopic homeostasis: either by
Seclerotherapy:by direct injection of 1-2ml of seclerosant or the alcohol.
Band ligation: in which a rubber ligature is place around the varix.
Pharmacological therapy.
This can be initiated as soon as Variceal hemorrhage ie suspected even before diagnostic endoscopy is performed. These drugs are vasopressin 0.1-0.4unit/minute and octreotide 50-100ug/hr are the most commonly used agents and control Variceal bleeding in 75%-80% of cases.
TIPSS (transjuguler intrahepatic port systemic stent shunting ) and balloon tamponad (This technique employs a Sengstaken-Blakemore tube possessing two balloons which exert pressure in the fundus of the stomach and in the lower oesophagus respectively) these maneuvers used when Variceal bleeding cannot controlled by above measures but the drawbacks of TIPSS are portal vein thrombosis, hepatic encephalopathy and stent occlusion while the ballooning may cause esophageal rupture.
Esophageal transaction.
Transection of the varices can be performed with a stapling gun, although this carries some risk of subsequent oesophageal stenosis. The operation is used when TIPSS is not available and when bleeding cannot be controlled by the other therapies described. The operative morbidity and mortality are considerable and the procedure is now rarely used
3)-preventing of recurrent Variceal bleeding.
B-blockers(propranolol 80-160 mg/day)b-blockers lead to reduce portal venous pressure lead to prevent recurrent Variceal bleeding.
Sclerotherapy or banding.
TIPSS.
Porto systemic shunt surgery.
-Non-selective porto-caval shunt.
-Spleno-renal shunt.
Liver transplantation.
Splenomegaly and Hypersplenism
Congestive splenomegaly is common in patients with portal hypertension. Clinical features include the presence of an enlarged spleen on physical examination and the development of thrombocytopenia and leukopenia in patients who have cirrhosis. Some patients will have fairly significant left-sided and left upper quadrant abdominal pain related to an enlarged and engorged spleen. Splenomegaly itself usually requires no specific treatment, although splenectomy can be successfully performed under very special circumstances.
Hypersplenism with the development of thrombocytopenia is a common feature of patients with cirrhosis and is usually the first indication of portal hypertension
Ascites
Definition Ascites is the accumulation of fluid within the peritoneal cavity. Overwhelmingly, the most common cause of ascites is portal hypertension related to cirrhosis; however, clinicians should remember that malignant or infectious causes of ascites can be present as well, and careful differentiation of these other causes are obviously important for patient care.Pathogenesis of cirrhotic Ascites.
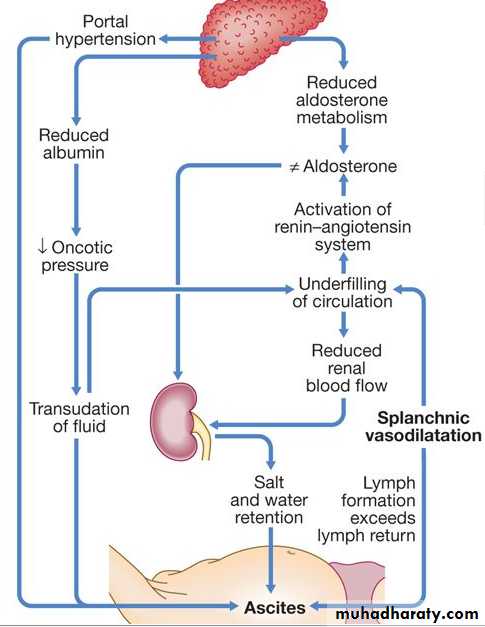
The pathogenesis of the development of ascites in liver disease is controversial, but is probably secondary to renal sodium and water retention. Several factors are involved.Sodium and water retention occur as a result of peripheral arterial vasodilatation and consequent reduction in the effective blood volume lead to activates various neurohumoral pressor systems such as the sympathetic nervous system and the renin-angiotensin system, thus promoting salt and water retention .
Portal hypertension exerts a local hydrostatic pressure and leads to increased hepatic and splanchnic production of lymph and transudation of fluid into the peritoneal cavity.
Low serum albumin (a consequence of poor synthetic liver function) may further contribute by a reduction in plasma oncotic pressure
Clinical features
Ascites cause abdominal distention with fullness in the flanks, shifting dullness on percussion and fluid thrill when Ascites is marked ,these signs are seen when ascetic fluid volume exceed a liter. distortion or eversion of the umbilicus, hernia , abdominal striae, diveration of the recti and occasionally meralga, paraesthetica and sacral edema. Pleural effusion can be found in 10% of patients usually in the right side.Investigation
•Ultrasonography is the best means of detecting ascites, particularly in the obese and those with small volumes of fluid.•Paracentesis (if necessary under ultrasonic guidance) can also be used to confirm the presence of ascites but is most useful for obtaining ascitic fluid for analysis. The appearance of ascitic fluid may point to the underlying cause .
Management
Sodium and water restriction Restriction of sodium intake to 100 mmol/day ('no added salt diet') is usually adequate. Drugs containing relatively large amounts of sodium and those promoting sodium retention, such as non-steroidal anti-inflammatory drugs, must be avoided Restriction of water intake to 1.0-1.5 L/day is necessary only if the plasma sodium falls below 125 mmol/L.
Diuretics Spironolactone (100-400 mg/day) is the drug of choice for long-term therapy because it is a powerful aldosterone antagonist. Some patients also require loop diuretics, such as furosemide, but these can cause fluid and electrolyte imbalance and renal dysfunction. Diuresis is improved if patients are rested in bed, perhaps because renal blood flow increases in the horizontal position.
Paracentesis The first-line treatment of refractory ascites is large-volume paracentesis with intravenous albumin replacement. Paracentesis to dryness or the removal of 3-5 L daily is safe, provided the circulation is supported with an intravenous colloid such as human albumin (6-8 g per litre of ascites removed, usually as 100 mL of 20% human albumin solution (HAS) for every 3 L of ascites drained) or another plasma expander.
Peritoneo-venous shunt (leveen shunt)
The peritoneo-venous shunt is a long tube with a non-return valve running subcutaneously from the peritoneum to the internal jugular vein in the neck; it allows ascitic fluid to pass directly into the systemic circulation. It is effective in ascites resistant to conventional treatment but complications, including infection, superior vena caval thrombosis, pulmonary oedema, bleeding from oesophageal varices andDIC, limit its use and insertion of these shunts is now rare.Transjugular intrahepatic portosystemic stent shunt (TIPSS)
TIPSS can relieve resistant ascites but does not prolong life. It can be used when liver function is reasonable or in patients awaiting liver transplantation.
Spontaneous bacterial peritonitis (SBP)
SBP; it is infection of ascetic fluid. The source of infection cannot usually be determined, but most organisms isolated from ascitic fluid or blood cultures are of enteric origin and Escherichia coli is the organism most frequently foundClinical features
This usually presents suddenly with abdominal pain, rebound tenderness, absent bowel sounds and fever in a patient with obvious features of cirrhosis and ascites. Abdominal signs are mild or absent in about one-third of patients, and in these patients hepatic encephalopathy and fever are the main features.
diagnosis
Diagnostic paracentesis may show cloudy fluid, and an ascites neutrophil count above 250 × 106/L almost invariably indicates infection.. Ascitic culture in blood culture bottles gives the highest yield of organisms. SBP needs to be differentiated from other intra-abdominal emergencies, and the finding of multiple organisms on culture should arouse suspicion of a perforated viscus
Treatment
Treatment should be started immediately with broad-spectrum antibiotics, such as cefotaxime. Recurrence of SBP is common but may be reduced with prophylactic quinolones such as norfloxacin (400 mg daily) or ciprofloxacin (250 mg 12-hourly) .