
Antibiotics Dr. Ali Ismail pharmacology
1. Early 1900s: Paul Erlich -Concepts of Chemotherapy and selective
toxicity Salvarsan for Syphilis
2. Fleming (1928) and Florey and Chain (1939) – penicillin
3. 1935: Gehard Domagk - sulfa drugs
4. 1944: Waksman – streptomycin
Antimicrobials
: are chemical agents (synthetic/natural) used for the treatment
of infections by suppressing or destroying the causative microorganisms
(bacteria, mycobacteria, fungi, protozoa, or viruses).
Antibiotics
: are substances produced by various species of microorganisms (bacteria, fungi,
actinomycetes) that suppress the growth of other microorganisms.
Classification of antibacterial drugs
1-
Bacteriostatic agents: Agents that inhibit the growth of the microorganisms by producing
reversible changes. This delay in the growth will give the immune system the chance to get rid
of the microorganism.
Bactericidal agents: Agents that kill the microorganism.
(Being a bactericidal or a bacteriostatic agent depends on the mechanism of action of the
antibacterial agent and on its concentration.)
2- Spectrum
Narrow spectrum: The range of activity for agents that kill the micro-organism is small. It
affects 1-2 classes of microorganisms only. For example, Penicillin-G affects G+ve organisms
and Neisseriae.
Broad spectrum: The range of activity extends to many micro-organisms. For example,
Tetracyclines depress G+ve, Gve, Rickettsiae and Chlamydiae. Separation between narrow and
broad spectrum activity is not clear due to the emergence of many resistant strains due to the
overuse of these antibiotics. Broad spectrum antibiotics should be restricted to treatment of
specific infections caused by a few organisms or even a single species of organism. The
property of broad specification should not be confused with a free license for broad-
nonspecific use.
Classification according to chemical structure
• Beta-lactam ( penicillins and cephalosporins)
• Aminoglycosides
• Tetracyclins
• Chloramphenicol
• Macrolids
• Quinolines
• Sulfanomides
Classification according to mode of action
Mechanisms of antimicrobial drug action:
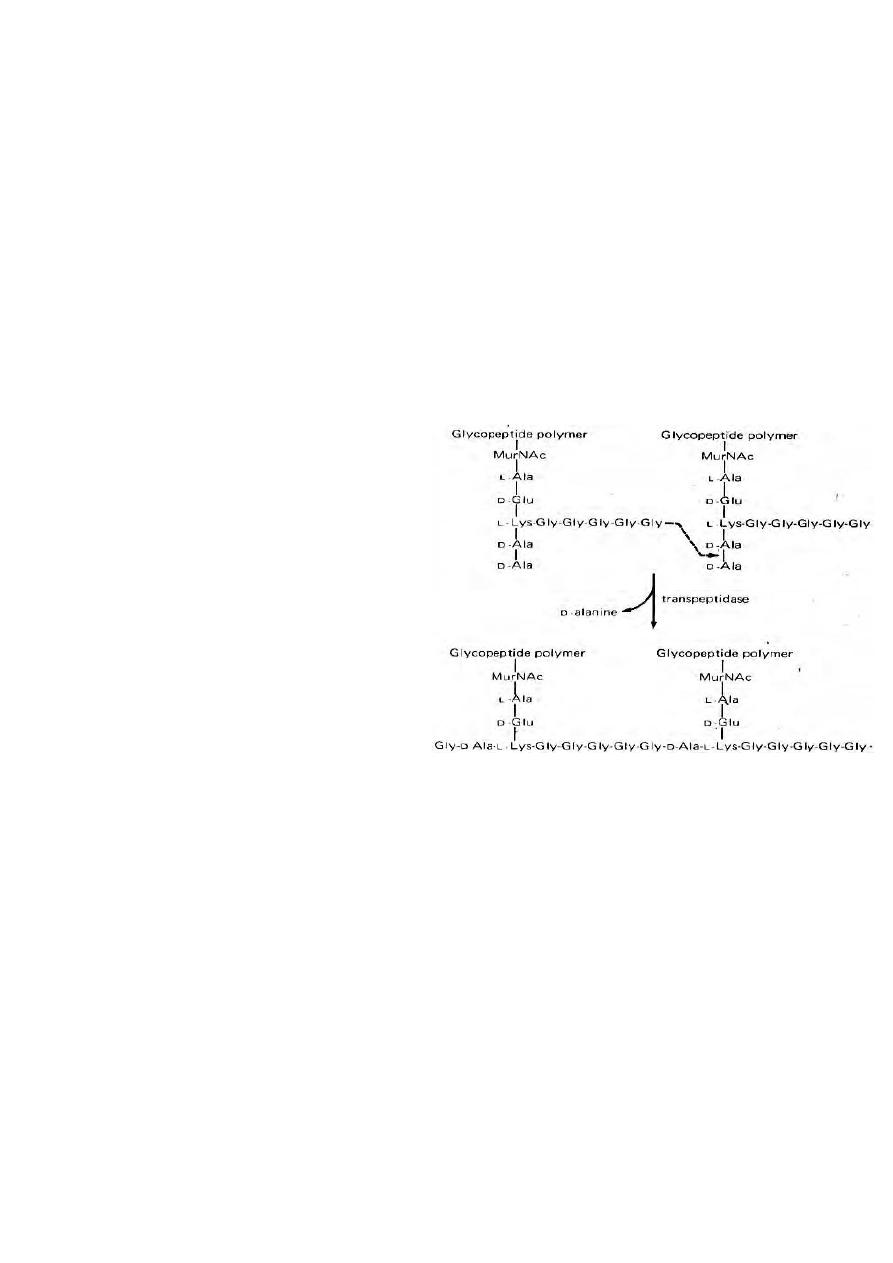
1.Inhibition of cell wall synthesis ( beta-
lactams)
Beta lactams contain β- ring which is an
analogue of D-alanyl-D-alanine on peptide
side chain of peptidoglycan à inhibits
transpeptidase from crosslinking
Peptidoglycan + binds penicillin binding
proteins à activation of autolysins
Bacitracin, Vancomycin, Cycloserine: Block peptidoglycan synthesis
2. Cell membrane function inhibitors (polypeptides):
Polymxin B: interact with phospholipids to increase permeability and decrease osmotic
integrity and leakage on intracellular components
3. Inhibition of protein synthesis ( tetracyclins, aminoglycosides, macrolids, chloramphenicol)
a) Tetracyclins: reversible binding to the 30s subunit of ribosome ànd inhibit binding of
aminoacyl tRNA to ribosome à inhibition of protein synthesis
b) Aminoglycosides: irreversible binding to the 30s subunit of ribosome and inhibit protein
synthesis and causes misreading of mRNA
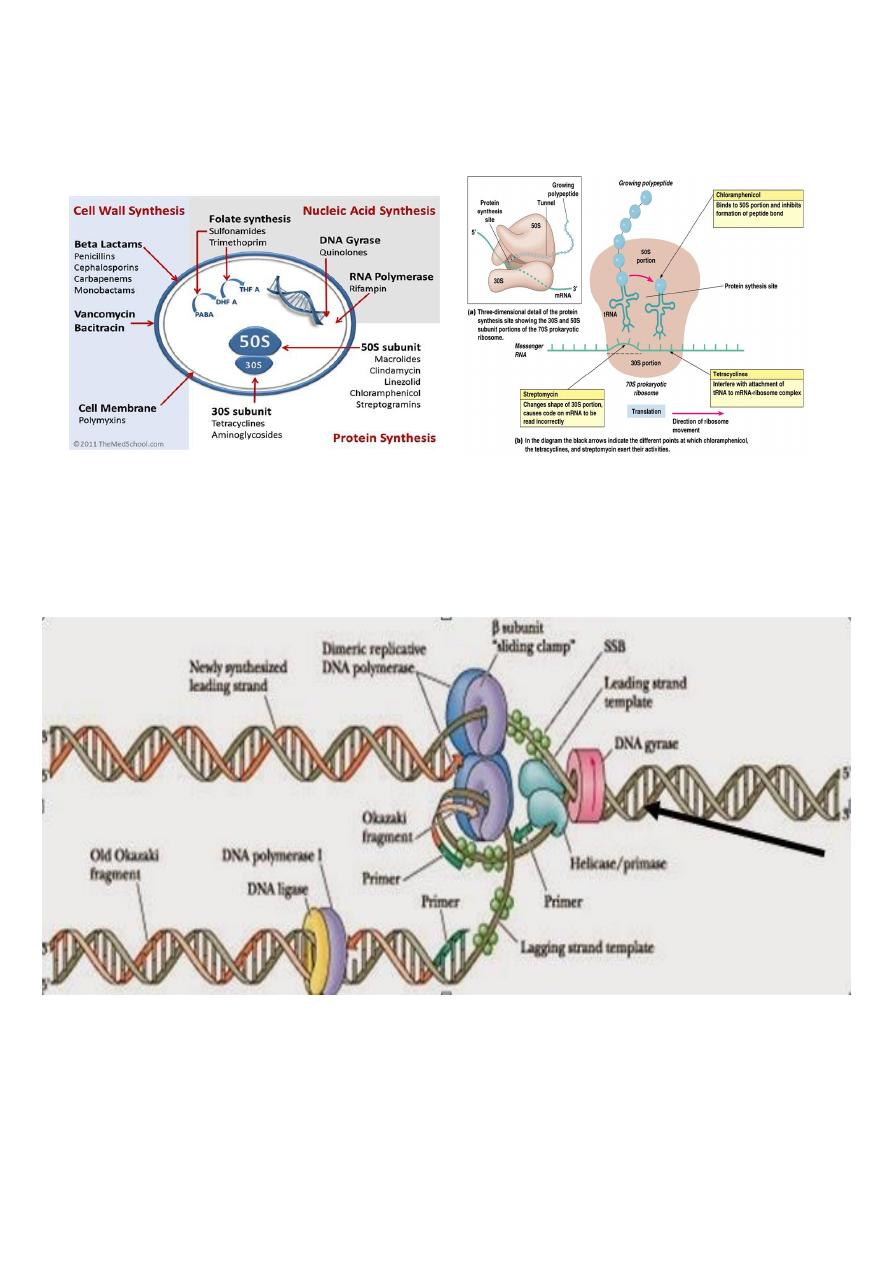
c) Macrolids: reversibly binds 50s subunit of the ribosome à inhibits translocation during
protein synthesis
d) Chloramphenicol: binds to 50s subunit of the ribosome à inhibits transpeptidation
during protein synthesis
4. Inhibition of nucleic acid synthesis ( quinolines, rifampicin)
a- Quinolines: inhibits DNA gyrase à inhibition of DNA replication.
b- Rifampicin: inhibits DNA- dependent RNA polymerase à inhibition of RNA synthesis
5. Antimetabolites ( sulfonamides, trimethoprim)
a- sulfonamides: competes with p-aminobenzoic acid for binding to the enzyme
dihydropteroate synthetase à no folic acid synthesis à no nitrogenous base synthesis
b-Trimethoprim: dihydrofolate reductase inhibitor

Using and avoiding antibacterial drugs
Antibacterials are valuable drugs if used appropriately. They are very effective in treating
infections if used in appropriate doses, at appropriate intervals and for the appropriate period
of time against sensitive microorganisms.
Anti-infective agents should be used only when:
a. A significant infection has been diagnosed or is strongly suspected.
b. An established indication for prophylactic therapy exists.
Abuse of these agents causes superinfections, cross-sensitivity and cross resistance, resulting
in inappropriate treatment and in consequent adverse reaction in addition to wastage of
money.
They should not be used in the following cases:
1. To treat all infections (e.g. viral infections or nonspecific inflammation).
2. For minor infections (e.g. superficial bruises).
3. For cases need surgical opening and draining such as abscess
Superinfection (suprainfection): Is the appearance of both microbiological and clinical
evidence of a new infection with pathogenic microorganisms or fungi not sensitive to the used
drugs during antimicrobial treatment of a primary disease. The body's natural resistance is
compromised, making it more susceptible to secondary infections by more dangerous strains.

Bacterial resistance:
Antimicrobial agents are loosing their effectiveness because of the spread of drugresistant
strains. Therefore, there might come a time when such agents are no longer useful to combat
diseases.
Mechanisms of resistance to antibiotics
1. Production of enzymes that inactivate the drug (eg. β -lactamase, which inactivates beta
lactam antibiotics; acetyl transferases, which inactivate chloramphenicol; kinases and other
enzymes, which inactivate aminoglycosides.
2. Alteration of the drug-binding site: this occurs with penicillins, aminoglycosides and
erythromycin.
3. Reduction of drug uptake by the bacterium: eg. Tetracyclines
4. Alteration of enzymes: eg. Dihydrofolate reductase becomes insensitive to trimethoprim.
Reasons for antibiotic resistance
1. Misuse of antibiotics selects for resistance mutants. Misuse includes:
a. Using outdated, weakened antibiotics
b. Using antibiotics for viral infection like common cold and other inappropriate conditions
c. Use of antibiotics in animal feed
d. Failure to complete the prescribed regiment
Selecting anti-infective agent:
a. The spectrum of activity of the antiinfective agent: It should be active against
the causative pathogen. This can be known by carrying the susceptibility tests or by a
good clinical experience in treating a given syndrome that will help in suggesting a
potential effective agent.
b. Patient factors: These factors play a very important role in the selection of a specific anti-
infective agent, determination of the appropriate drug dosage and route of
administration,...etc. Those factors include:
1. History of drug allergy or adverse
reactions. Anaphylaxis or reactions due to immunoglobulin E (IgE) may be life
threatening when taking penicillins.
2. Age: A drug’s pharmacokinetic properties vary widely in patients of different age groups.
3. Underlying disease: -A pre-existing kidney and liver disease, CNS disorder. Neuromuscular
disorders.
4. Immunological status: Patients with impaired immune system require a bactericidal agent
rather than a bacteriostatic one.
5. Pregnancy and lactation.
6. Genetic traits.
Combination therapy in special situations
- Extend the antimicrobial spectrum especially in Initial empiric therapy
-Mixed infections or severe infections:
-To prevent the emergence of resistance:
Duration of therapy:
Acute cases: Treatment of acute uncomplicated infections generally should continue until the
patient has been a febrile and asymptomatic for at least 72 hours (minimum 5 days in most
cases). Other cases as in Strep. throat (
Streptococcal
pharyngitis) should be treated for 7-10
days. Some infections require a proof of eradication by culture.
Chronic cases: Treatment of chronic infections (e.g., endocarditis, osteomyelitis) may require
a longer duration (4 to 6weeks), with a follow-up culture analysis afterwards.
Cell wall inhibitors:
Beta lactams (penicillins and cephalosporins)
Penicillins
:
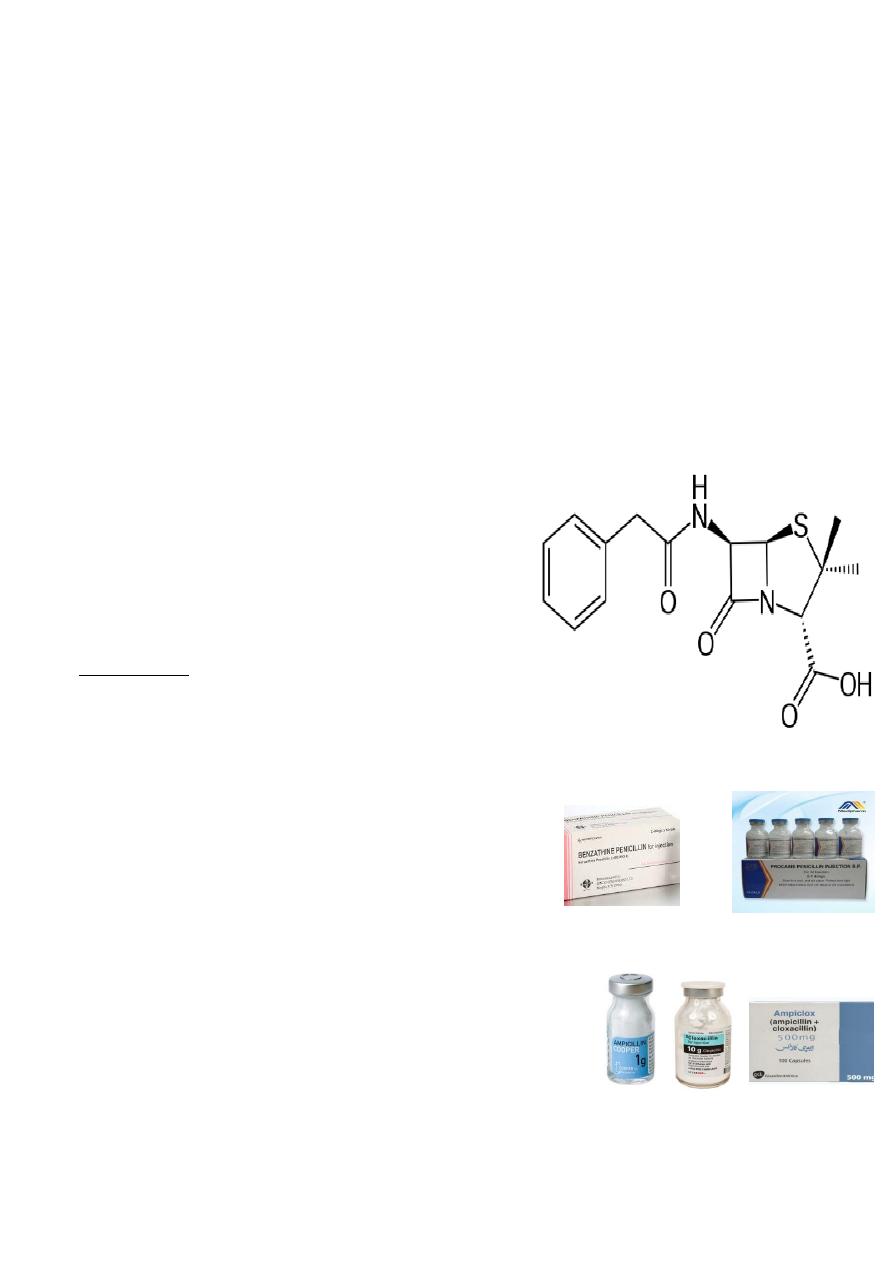
Chemical structure: Three components: A thiazolidine
ring, the β-lactam ring (
responsible for their activity
),
and a side chain (
determines in large part to
antibacterial spectrum and pharmacologic properties of
a particular penicillin)
Classification of Penicillins
Natural Penicillins
Penicillin G (benzylpenicillin)
Penicillin G benzathine,
phenoxymethyl penicillin)
Penicillinase-Resistant Penicillins
Methicillin, Cloxacillin, Oxacillin, Nafcillin, Dicloxacillin
Extended-Spectrum Penicillins
Ampicillin , Amoxicillin,
Anti-Pseudomonal Pencillins
Carbenicillin, Ticarcillin, Piperacillin
ß-Lactamase Combinations
Ampicillin- Cloxacillin
Amoxillin-clavulanic acid,
Ampicillin-sulbactam,
Ticarcillin-clavulanic acid
Natural penicillins:
Benzylpenicillin & Phenoxymethyl penicillin
These two are known as the natural penicillins. They are the first two penicillins that were
discovered and are still in use. Natural penicillins are narrow spectrum antibiotics and are only
active against facultative gram-positive cocci, rods and gram-negative cocci. Several
anaerobic gram-negative rods are sensitive to penicillin, with the notable exception of
Bacteroides fragilis
.
Benzyl penicillin
is the drug of choice in streptococcal, pneumococcal, gonococcal, and eningococcal infections.
It is also used in anthrax, diphtheria, gas gangrene, leptospirosis, syphilis, tetanus, yaws, and
in the treatment of lyme disease in children.
It is inactivated by the gastric fluids, and absorption from the gut is low; therefore it is given
by injection.
In addition to the use of Pen. G as sodium or potassium salts (soluble Pen. G), it is also
available in two other salts that are commonly used. They are:
a-
Procaine penicillin
: a sparingly soluble salt of benzylpenicillin. It is used in intramuscular
depot preparations that provide therapeutic tissue concentrations for up to 24 hrs. It is the
preferred choice for the treatment of syphilis, but neurosyphilis requires special consideration.
b-
Benzathine penicillin
:
a benzylpenicillin salt with a very low solubility, giving a prolonged
action after intramuscular injection. Its duration of action is 20 days.
Phenoxymethyl penicillin (Pen. V)
Has a similar antibacterial spectrum as Pen. G, but it is less active. It is gastric acid stable
so it is suitable for oral administration. It should not be used for serious infections because
absorption can be unpredictable and plasma concentrations are variable.
Indications:
Benzylpenicillin
mainly indicated for the treatment for:
throat infections
otitis media,

streptococcal endocarditis
meningococcal and pneumococcal meningitis (if caused by susceptible microorganism)
prophylactic agent after limb amputation.
Also it is used in combination with other agents if more than one organism are suspected.
Phenoxymethyl penicillin
is indicated principally for
respiratory tract infections in children, for Streptococcal tonsillitis and for continuing
treatment after one or more injections of Pen. G when clinical response has begun.
It should not be used for meningococcal or gonococcal infections.
It is used prophylactically against rheumatic fever following streptococcal infections.
Contraindications:
They are contraindicated in the case of hypersensitivity to any of the penicillins or
cephalosporins. Procaine penicillin is also contraindicated in the case of hypersensitivity to
procaine or any other “caine type” local anesthetic.
Penicillinase resistance penicillins (Antistaphylococcal penicillins)
Cloxacillin, dicloxacillin, flucloxacillin and methicillin
Most staphylococci are now resistant to benzylpenicillin because they produce penicillinases.
Cloxacillin and flucloxacillin
are not affected by such enzymes
, so they are effective in
infections caused by penicillin resistant staphylococci, but they are less potent than Pen. G
against penicillin sensitive microorganisms. and generally ineffective against
G-ve bacteria and methicillin resistant staphylococci.
The only difference between cloxacillin and flucloxacillin is that flucloxacillin has a higher
bioavailability than cloxacillin after oral administration. Another two examples.
Methicillin is toxic and didn’t used medicinally
These drugs used in combination with ampicillin: ampicillin with cloxacillin or flucloxacillin
and amoxicillin with cloxacillin.
Cloxacillin: prepared as capsules and suspension. Flucloxacillin: Not available in a separate
formulation, but as combination with ampicilin in capsules.
Indication:
Cloxacillin and flucloxacillin are indicated for the treatment of infections caused by
penicillinase producing Staphylococci. Methicillin is toxic and not used medicinally.

Extended-Spectrum Penicillins also called (aminopenicillins):
including ampicillin, amoxicillin
and (bacampicillin and pivampicillin), which are esters of ampicillin.
Aminopenicillins are active against some G+ve and G-ve organisms but inactivated by
penicillinases, including those produced by
Staphylococcus aureus,
and by common G-ve
bacilli such as
Escherichia coli
.
The majority of Staphylococci, 50% of
E. coli
strains and 15% of
Haemophilus influenzae
strains are now resistant.
Amoxicillin is a derivative of ampicillin that differs only by one hydroxyl group. Unlike
ampicillin it can be given 3 times daily without regard to food. Ampicilline is given 4 times
daily and its absorption affected by the presence of food in the stomach, so it should be taken
one hour before or two hours after the meal).
Indication:
They are principally indicated for the treatment of chronic bronchitis and mild ear infections,
both of which are usually due to
Streptococcus pneumoniae
and
Haemophilus influenzae.
They are also indicated for: urinary-tract infections, otitis media, sinusitis, chronic bronchitis,
invasive salmonellosis, and gonorrhea.
Amoxicillin is also used for typhoid fever and endocarditis prophylaxis.
Antipseudomonals
include both carboxypenicillins (carbenicillin and ticarcillin) and ureidopenicillins (piperacillin,
azlocillin, and mezlocillin).
Antipseudomonal penicillins are similar to the aminopenicillins in structure but have either a
carboxyl group or urea group instead of the amine.
The major advantage of carboxypenicillins is their activity against
Pseudomonas aeruginosa
(one of the major pathogens responsible for nosocomial pneumonia) and certain indole-
positive
Proteus
species that are resistant to aminopenicillins. Ticarcillin is stronger against
P.
aeruginosa
and
Enterobacter
species than carbenicillin.
Against anaerobes and Gram-positive organisms, carboxypenicillins generally have the same
spectrum of activity as penicillin G. However, they are substantially weaker in comparison with
penicillin G.

Ureidopenicillins have greater activity against
P. aeruginosa
compared to carbenicillin and
ticarcillin. Piperacillin is the most potent of the extended-spectrum penicillins against
Pseudomonas
. The spectrum of piperacillin and mezlocillin is extended to include
Klebsiella
,
Enterobacter
,
Citrobacter
.
All antipseudomonals are destroyed by β-lactamases.
The extended-spectrum penicillins are not used in the treatment of infections caused by
Gram-positive bacteria because penicillin G and aminopenicillins are more potent against
these organisms.
Antipseudomonals penicillins may be used in combination with Aminoglycosides.
Note:
The natural penicillins was originally used as units. International Unite= 0.6 microgram
(0.0006 milligram) of penicillin ( 1 mg = 1670 IU) . Synthetic and semisynthetic penicillins in mg
……….
Side effects of Penicillins:
- Hypersensitivity and anaphylactic shock
Hypersensitivity is one of the most important adverse reactions to penicillins. The frequency
of allergic reactions to all penicillins ranges from 0.7% to 10%. The manifestations of penicillin
allergy include maculopapular or morbilliform rash, fever, urticaria, exfoliative dermatitis,
swelling of the throat, difficulty breathing, eosinophilia, serum sickness, Stevens-Johnson
syndrome, and anaphylactic shock (0.004% to 0.015%)
- Pain in injection
- GI: diarrhea, nausea, vomiting, pseudo membranous colitis (rare).
-CNS: convulsive seizures.
-Skin: pruritus, urticaria, or other skin eruptions.
-Hematological: hemolytic anemia, thrombocytopenia, purpura, eosinophilia, leukopenia,
agranulocytosis.
-Others: superinfections
