Plastic surgery
Dr.Muslim Kandel 2019-20
1
Lecture one
Plastic and reconstructive surgery
General principles
The plastic surgery is correction of deformities due to congenital, post-traumatic
or post- operative , to restore and optimize function and shape. , the result depend
on tissues loss, rapidity of wound healing and scar formation
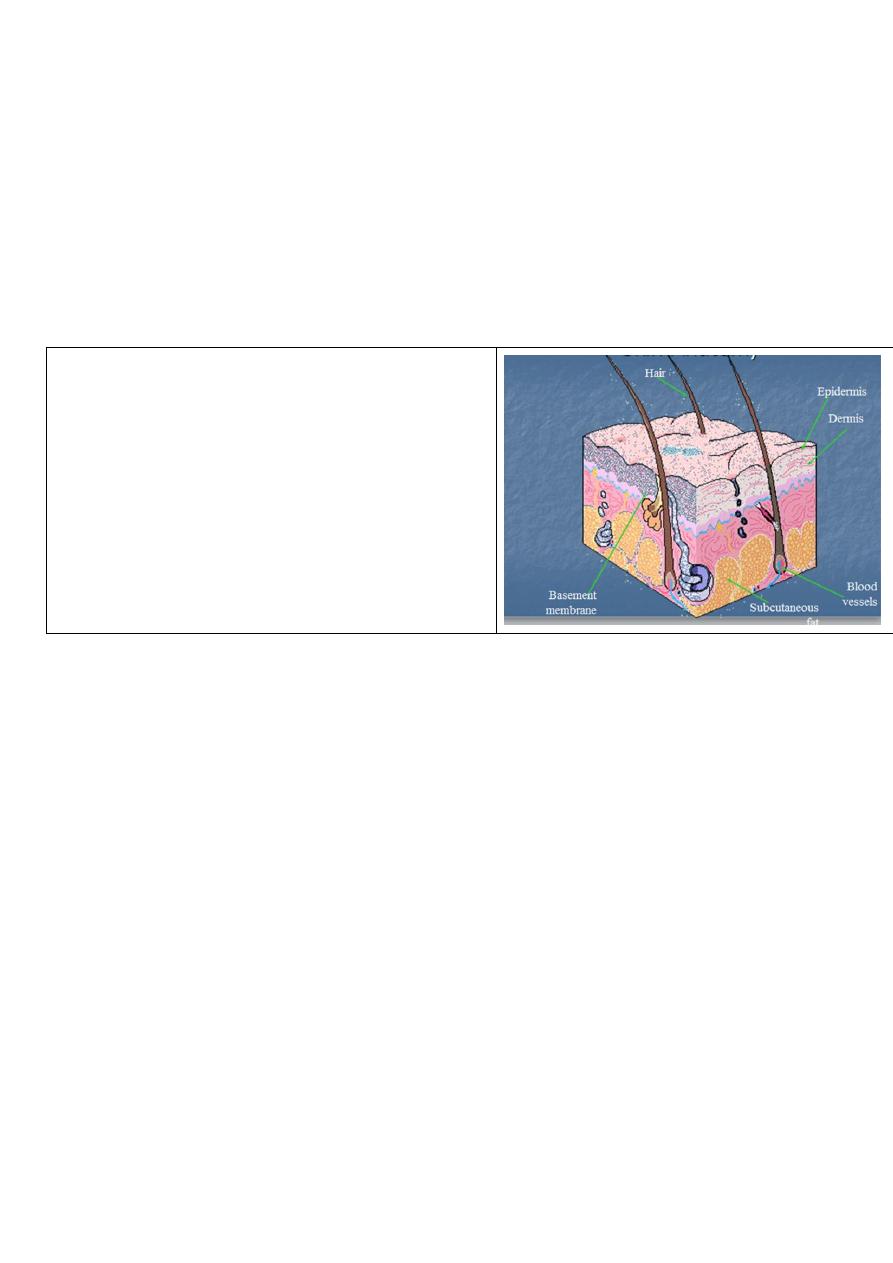
Anatomy of skin
skin is largest organ in body ranging from 0.22 m²
in new born to more than 2m² in the adult.
Functions of skin
1-It provided barrier to invasion by m.o
2-regulate of heat with environment
3-vitamin D synthesis by sun light
Layers of skin
It consists of epidermis and dermis.
1-Epidermis: is the outer layer
composed of keratinized stratified squamous epithelium, it divided into:
• Stratum germinatirum: which rest on dermis and generate the cell of stratum
corneum.
• Stratum corneum: This is the desquamating dead superficial layer.
2- dermis :- which is 20 times thicker than epidermis, it consists of non-cellular
connective tissues (collagen and elastic fibers) and ground substances. It divided into:
• papillary dermis (Upper & thin).
• • reticular dermis (Lower &thick) which extended form papillary dermis to
subcutaneous tissues.
Dermis contained skin appendages :-
sweat gland, blood vessels, lymphatics and pilosebaceous units
3-subcutenous layer
the skin is connected to the underlying bone and deep fascia by layer of areolar tissues
that varies in thickness,
it prominent in palm and sole, and absent in eyelid.
Plastic surgery
Dr.Muslim Kandel 2019-20
2
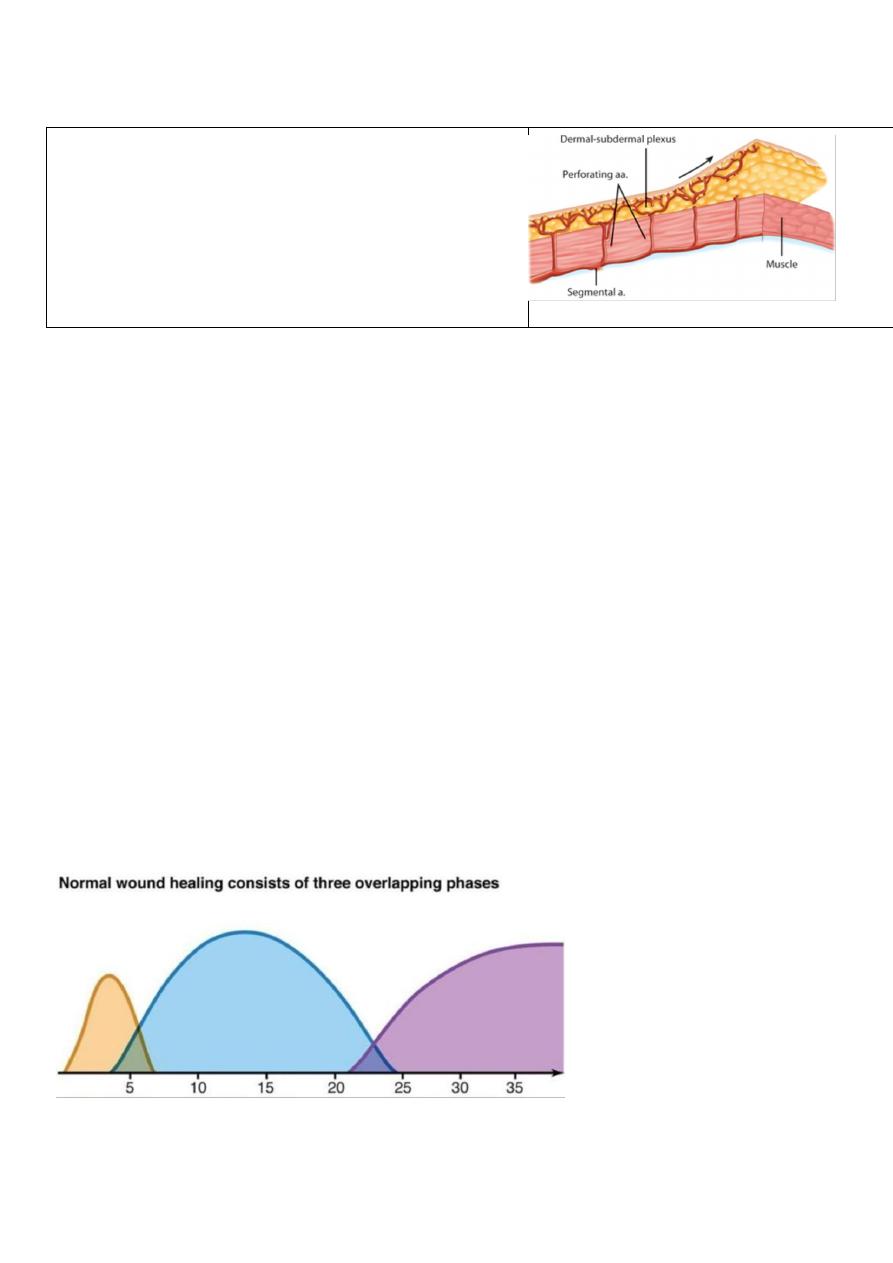
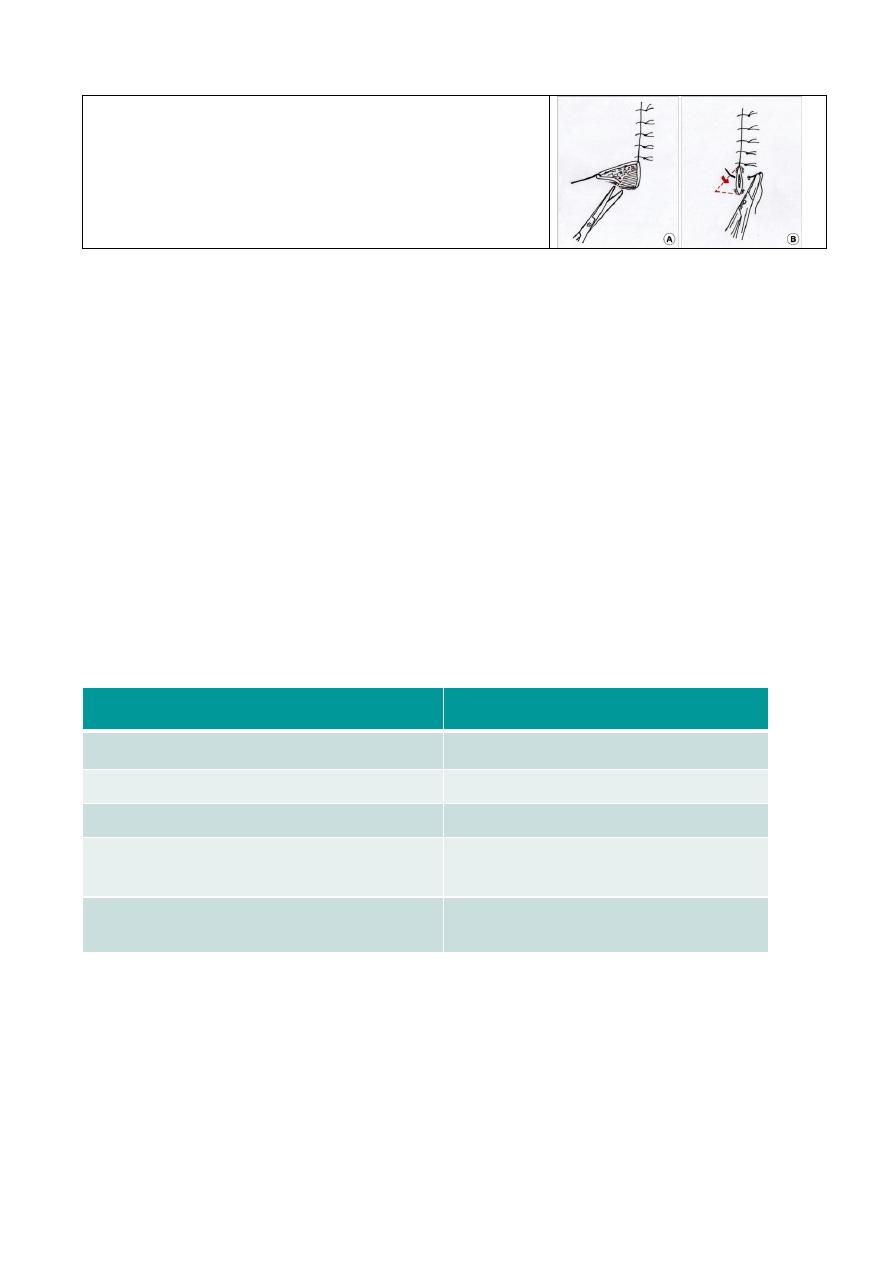
Blood supply of skin:
1-Major vessels: deep to muscle (musculocutaneous)
perforators which pass perpendicular through the
muscle and deep fascia dermosubdermal plexus which
supply the skin.
2-Direct cutaneous artery: superficial to muscles then
dermo-subdermal plexus
Priorities in plastic surgery
1. Healing
2. Function ( reconstruction )
3. Cosmetic ( less scar formation )
Wound
Wound is a breach in normal tissue continuum as a result of blunt or sharp
trauma may be accidental injury or surgical
wound healing is classically divided into three types: primary intention, delayed
primary intention, and secondary intention).
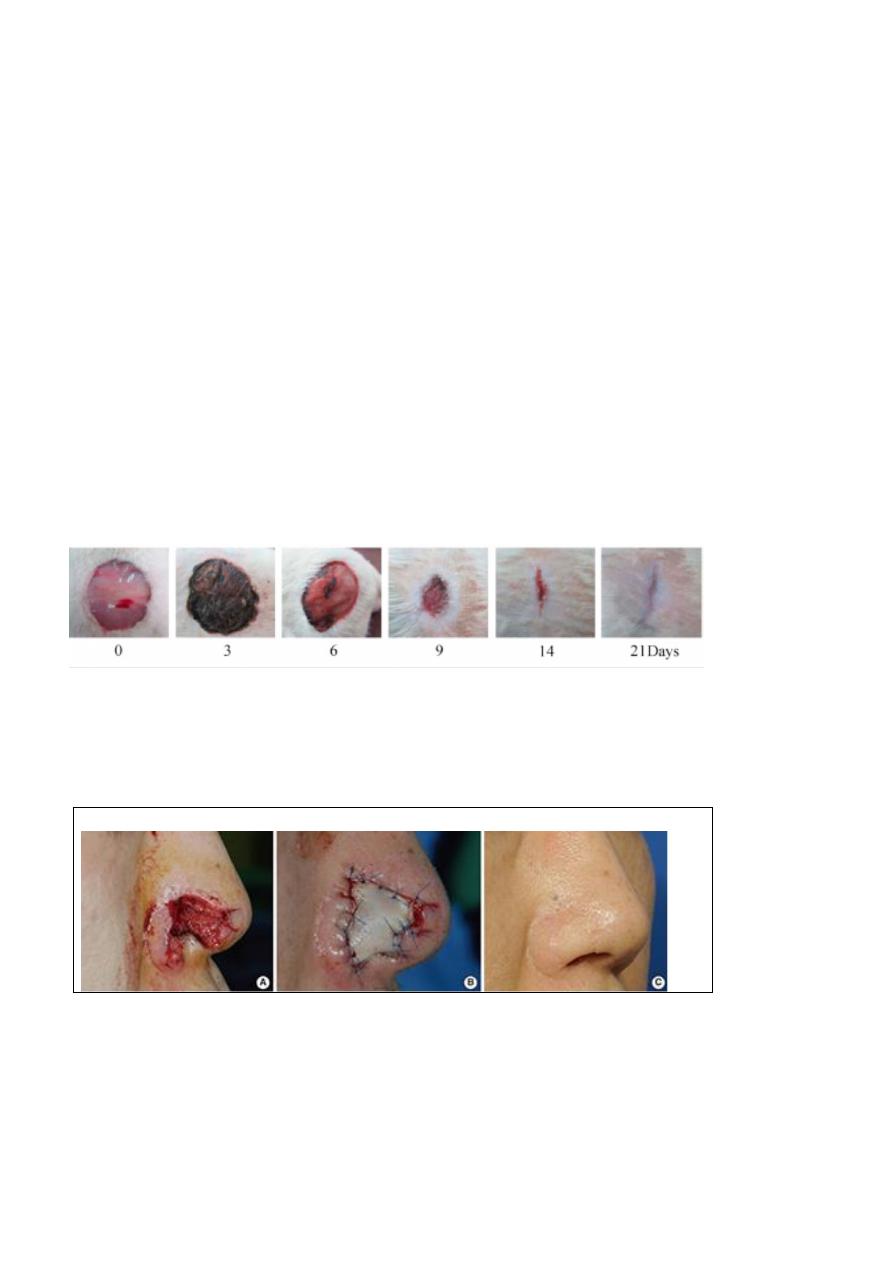
Phases of wound healing:
1-inflammatory phases: begin at time of injury and last 2-3 days, begin with
vasoconstriction to achieved hemostasis ,then vasodilatation with infiltration of
neutrophils,monocytes and limited number of lymphocytes
2-Proliferative phase: begin around day 3 and last through 3weeks during which
epithelization and collagen synthesis occur.
3-Remolding phase: during which increase in collagen production and breakdown,
continuous for 6 month-1 year. Wound strength increase as collagen reorganized and
vascularity decrease.
Plastic surgery
Dr.Muslim Kandel 2019-20
3
How the wound healing occur ?
(Methods of wound healing)
1- Primary intention
By epethelization from wound edges , i,e sharply incised wound , like surgical
wound , healed by primary intention.
-- little or no tissue is lost --very small scar
2- Delayed primary intention
In crushed contaminated wound , leave wound opened after wound cleansing
and debridement This delay allows inflammatory and immune processes to control
wound contamination.--- more scar tissue develops.
3- Secondary intention
Wounds heavily contaminated or with significant loss of tissue
They gradually become filled with 'granulation tissue' then closed by the processes of
contraction and epithelialization ,
Or the gap difficult to close so skin grafts or flaps are required to close the wound.
A graft
is a piece of tissue that is moved without its blood supply and relies on its
recipient bed to re-establish a blood supply.
A flap
is a piece of tissue that is moved maintaining its blood supply and is not reliant
on the recipient site for its vascularity
Factors affect wound healing
A) general :- Ca , DM , Malnutrition , jaundice , septecaemia . steroid
Vit. C deficiency , uremia
B) local :- poor blood supply (tension , atherosclerosis , ).infection , poor
alignment, foreign body , local X ray

Plastic surgery
Dr.Muslim Kandel 2019-20
4
Principles of wound closure
1-The Closure Depend on health of wound
When the wound is clean direct closure
by approximation its edge s
-- no everted or inverted
--without tension.
To be heal by primary intension
When the wound is lacerated delay closure
Preperation of wound for few days or weeks then either
-- delay primary suturing
-- healing by secondary intention ( graft , flap )
2-Wound preparation
- Wound cleansing and irrigation (washing) to remove foreign bodies and decrease the
numbers of bacteria.
- Wound debridement
is more conservative in the face than in other areas of the body because severely damaged
skin often survives because of the rich facial blood supply
Method of debridment:
• Mechanical: sharp or blunt excision of dead tissues.
• Gauze: repetitive application of moistened gauze.
• Chemical: topical enzyme application
3-avoiding excessive retraction and pressure on wound
by irrigation and moist pack should be used to prevent wound desiccation.
4-aseptic technique: such as hand scrubbing, using of sterile instrument
5-hemostasis: by electrocautery. , clamping , suturing or Topical hemostatic e.g. fibrin glue.
Because the bleeding can cause ischemia and hematoma which lead to infection .
6-antibiotics coverage which indicated for the fallowing:
• Acute wound with surrounding cellulitis with gross contaminated.
• Human or animal bit.
• Immunosuppressed or diabetic patient.
•Valvular heart disease to prevent endocarditis
7- The need for tetanus immunization depends on the nature of the wound and the patient's previous
immunization history.
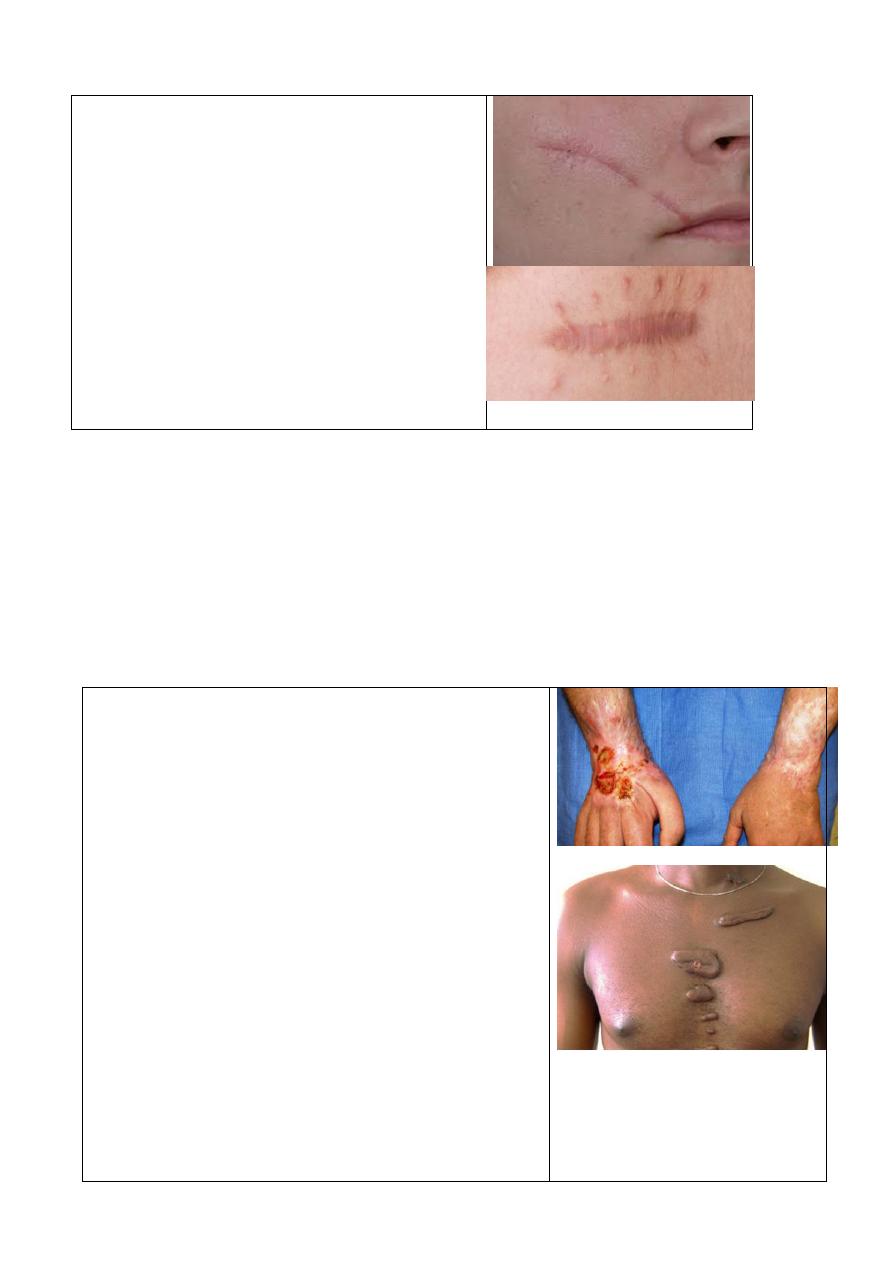
Scar
Scar is residual visible mark of wound , almost all wound result in scar
Which pass in 3 stages :-
I-
0-4 w fine nonncontrectil
II-
4-12 w thick hard contracted
III-
12w- 6 mounths soft white , relax
Plastic surgery
Dr.Muslim Kandel 2019-20
5
Factors affect scar
1- position (ie sternum )
2- age ( adult > child )
3- race ( nigroo> whites )
4- direction of wound (skin lines)
5- bad alignment of wound
6- Stability of wound ( joint)
7- Wound infection
8- Poor blood supply ( may cause necrosis
and slughing)
Types of scar
Leanear scar ( surgical )
Area scar (burn )
Complication of scar
1-Hypertrophy of scar ( which not extend beyond wound )
2-kiloid (continue enlarge after 6 mounths beyond wound )
3-contrection ( deformity, limitation of joint )
4-streching due to tension of stitches cause larger scar.
5-malignent changing (Marjolin ulcer in chronic unhealed scar of joint )
which is premalignent , should be excised )
6-hyperpigmentation or depegmentation
Surgical incision
To minimizes scar formation should be :--
1- the incisions should be placed within, or parallel
to, skin lines(Langer s lines)
2- In the face these are obvious at 'wrinkle lines' of
the muscles of facial expression. Placement of
incisions at junctions of hairline such as the eye brow
and forehead skin,
3- minimal skin tension
4- good depredment of wound and washing
5- good alignment of wound
6- use less irritant stitches ( nylon , PDS. Steel wire
) , subcutical maneuver better than interrupted ,
7 -fixation of wound specially at joint (splinting )
8- to reduce stitch marking, early removal of
stitches 3-5 days in face
While in abdomen ( 7-8 d )can be reinforced at this
time with skin tapes.
Plastic surgery
Dr.Muslim Kandel 2019-20
6
9-avoid dog ears at the angles of wound ,so use
elliptical incision rather than rounded
Traumatic tattooing
Foreign bodies embedded in soft-tissue wounds which still permanently
Treatment is dermabrasion or excision.
Delayed removal of traumatic tattooing is difficult, if not impossible.
Keloid formation
Is an extreme overgrowth of scar tissues which continue after 6 m extend
beyond site of incision , due to inhibition of maturation of fibrous tissues for
unknown cause , so still continue formation and not subside , its regarded
type of fibroma. Usually occur at face , sternum , shoulder ( unlike
hypertrophic scar which occur at flexer surface )
Treatment : -
1-germent ( continue pressure )
2- intradermal injection of trimeselon
3- radiotherapy and scar revision in difficult cases
hypertrophy
Keloid
(1) Rarely familial
more familial
(2) develop soon after injury
up to a year later.
(3) may subside in time
rarely do
(4) more likely to cause contracture
over joint surface
rarely do
(5) no treatment necessary
i. Triamcinolone
ii. Excision – high recurrence rate
Soft-tissue coverage
By 2 methods
a- Graft :- Its transplantation of tissues which blood supply depend
completely on recipient area
b-Flap :- Its transplantation of tissues which blood supply depend on donor
vessels
Plastic surgery
Dr.Muslim Kandel 2019-20
7
lecture tow
skin substitution
A-
Skin grafts
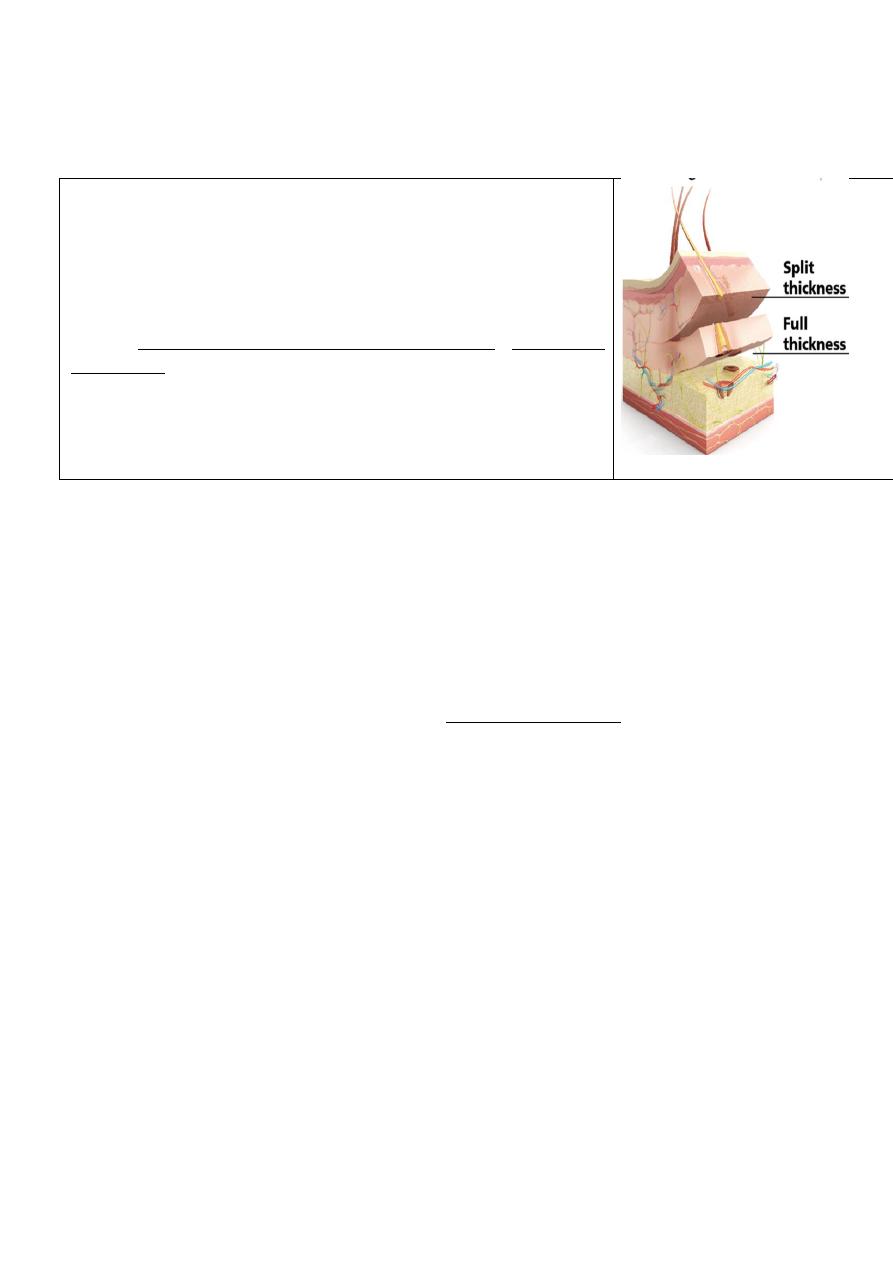
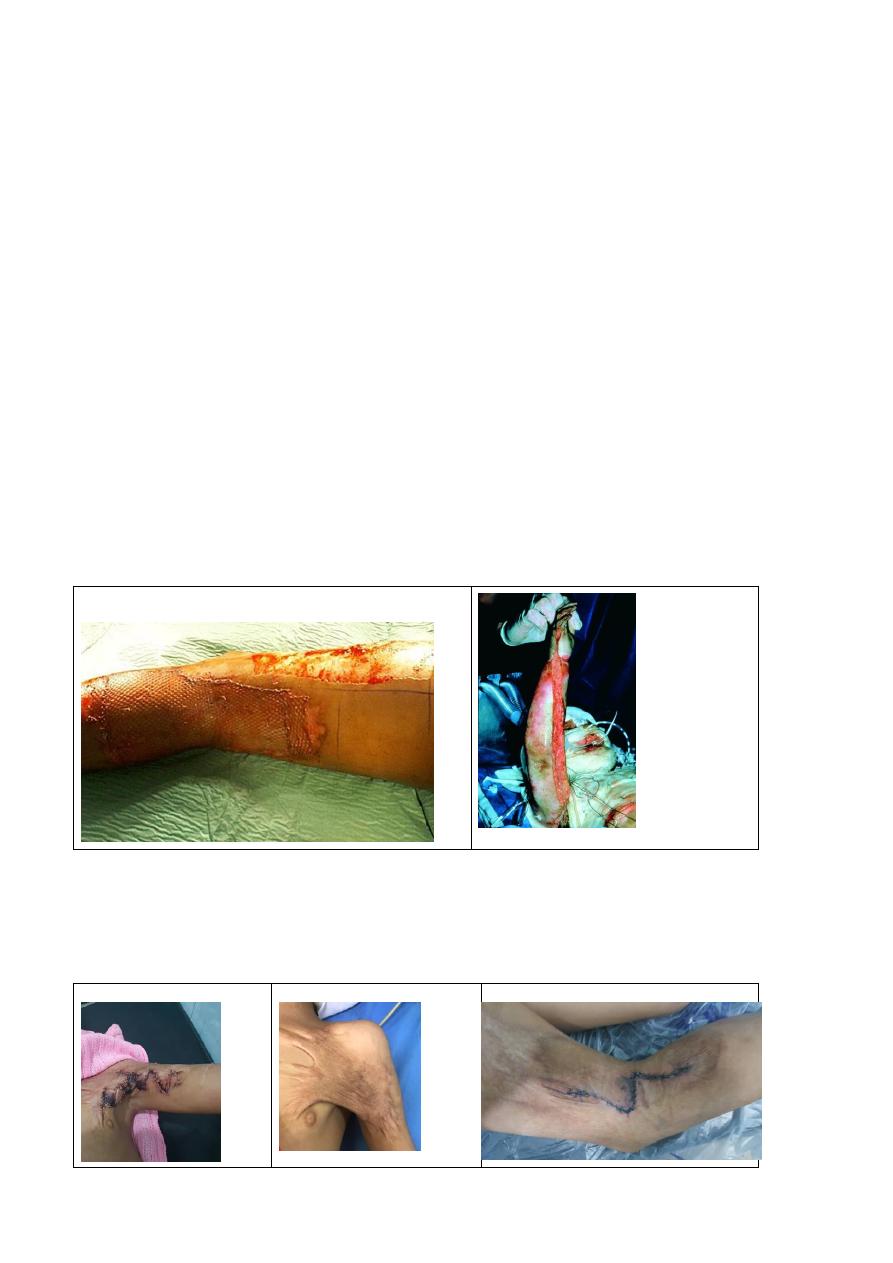
I - Partial-thickness skin grafts
consist of epidermis and a variable thickness of dermis. There
remains some dermis on the donor site that heals by
epithelialisation from the cut ends
donor site The thigh, is most frequently used as a donor site,
but almost anywhere else can be used.
using a skin graft knife (Hompy knife )or a power
dermatome. These consist of a blade and a guard that can be
adjusted to determine the thickness of the graft.
Partial-thickness grafts are used to resurface relatively large
areas of skin defect and are particularly useful in burns
II - Full-thickness grafts
consist of epidermis and all of the dermis; the donor site will not epithelialise and
must be closed, usually directly.
Suitable donor sites are postauricular, supraclavicular and groin.
Full-thickness grafts are most commonly used in repairing defects on the face
Grafts taken from above the clavicles retain the ability to blush and can provide a
very good color match for facial skin, whereas grafts from below the clavicles
will tend to look pale.
Full-thickness grafts are harvested using a scalpel and forceps, dissecting at a
level just below the dermis
.
Usual Donor site of full thickness skin graft:
1. Postauricular skin.
2. Upper eyelid.
3. Supraclavicular skin.
4. Flexural skin: the antecubital fossa and groin.
Usual Donor site of partial thickness of skin graft:
Any site can be used. But most commonly donor sites are:
1. The thigh and the upper limb.
2. The flexor aspect of the forearm.
3. The whole of reasonable plane of torso.
4. Other aspect of the forearm and lower leg, these site usually used when
above areas not available.
III- Composite grafts
Composite grafts consist of skin and some underlying tissue such as fat and
cartilage. Again, donor sites must be closed directly.
Plastic surgery
Dr.Muslim Kandel 2019-20
8
--Composite grafts carry the highest risk of failure .These grafts ‘ have to be
carefully designed to be as thin as possible Their maximum thickness can only be
a few millimetres;
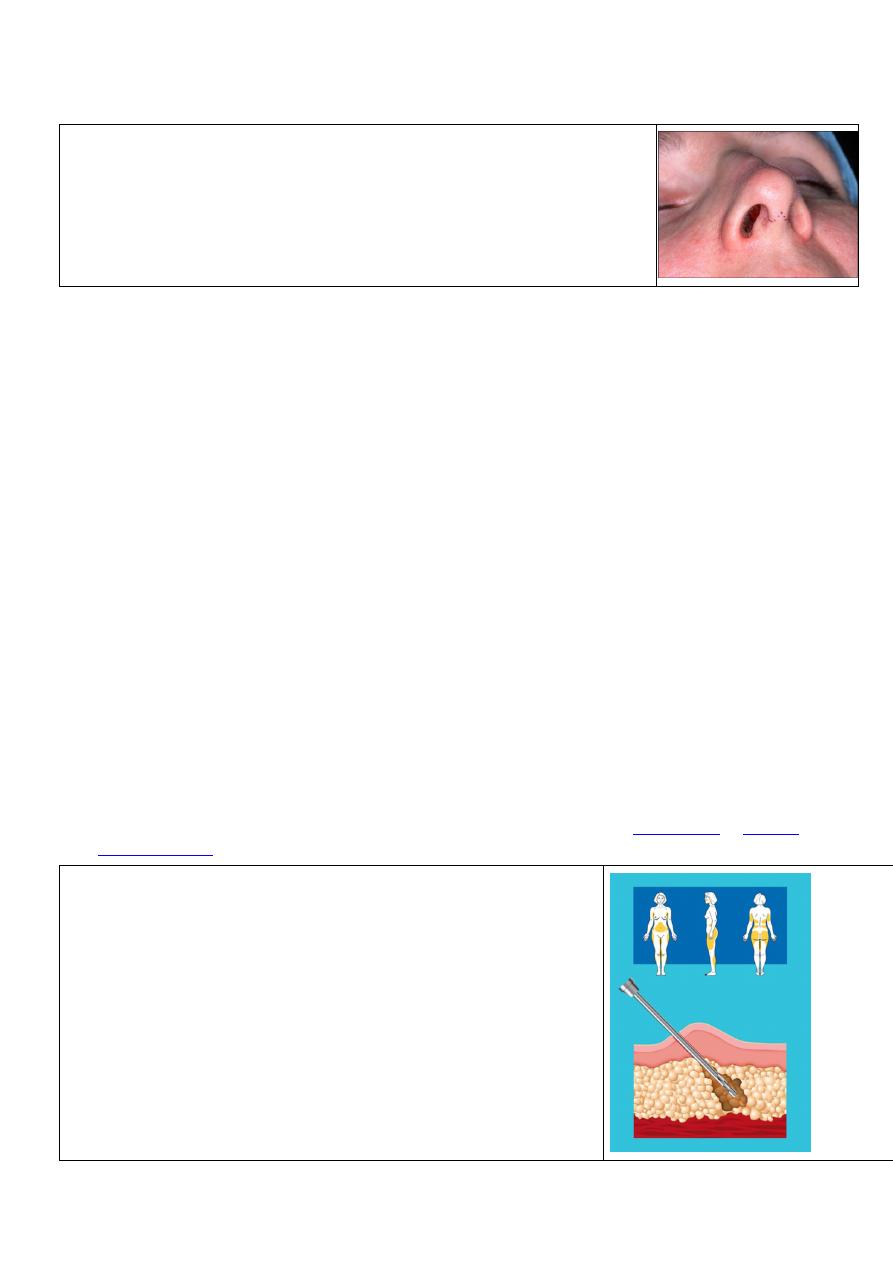
Portions of ear, skin and cartilage can be used to reconstruct nasal defects.
IV-Skin-graft substitutes
Cadaver skin, Various types of collagen sponge have also been used as temporary
skin substitutes
Human epithelial cells can be grown in tissue culture to produce coherent sheets
that can be transferred as a pure epithelial autograft or allograft
Contraindication of skin graft:
1. Deadly, heavy contaminated wound.
2. Area of poor vascular supply.
3. Tendon denuded of paratenon.
4. Muscle denuded of epimysium.
5. Cartilage denuded of perichondrium.
6. Bone denuded of periosteum.
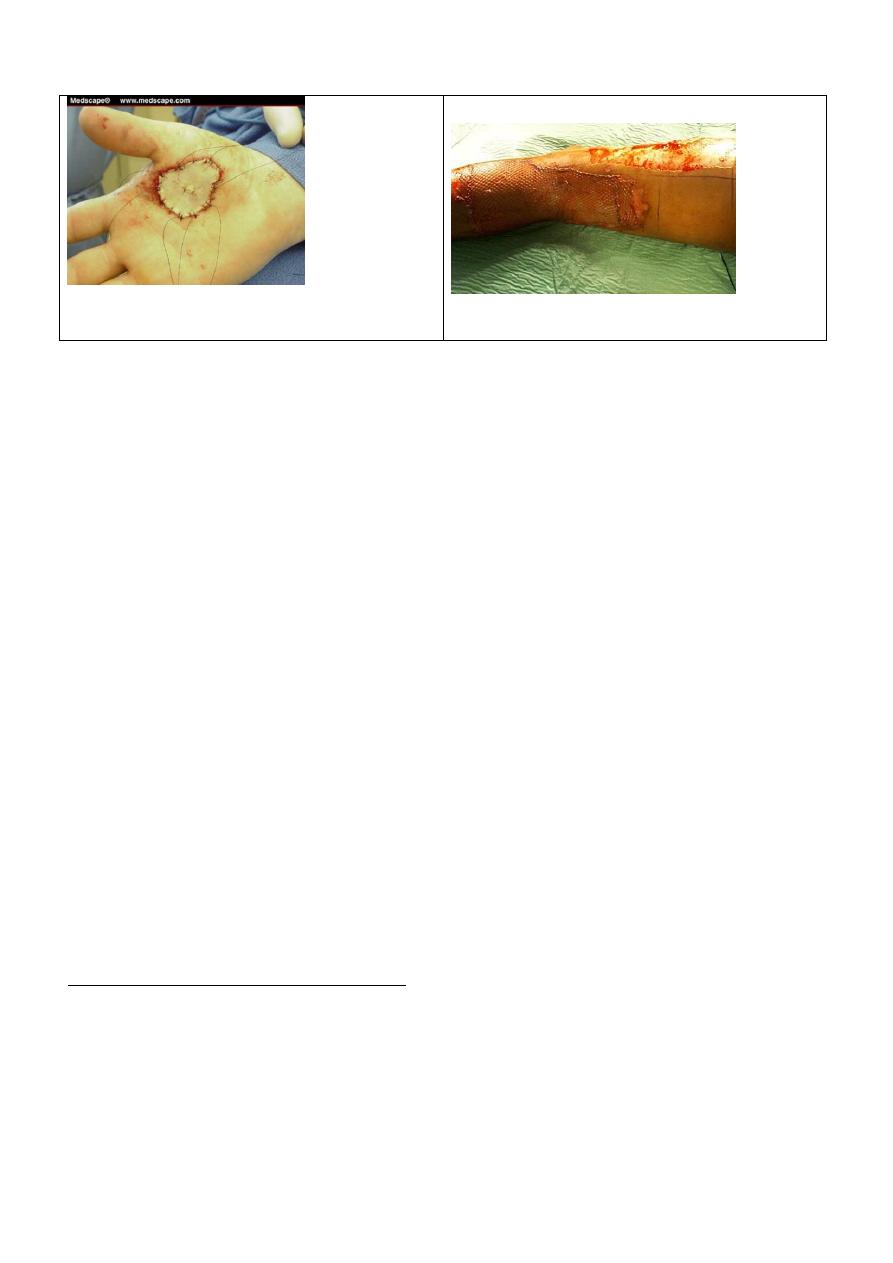
split thickness skin graft
Full thickness skin graft
1.Donor site healed
spontaneously.
1. Donor site should closed directly,
Since no epithelium appendage remain
for resurfacing
2. Good intake.
2. Intake less readily.
3. Have more 2ndry Contraction
3. Undergo less 2ndry contraction.
4. Less cosmetic result
4. Have better cosmetic result
5-used large area
5. Used small area
Cultured skin graft:
Used for coverage of large defect when autologus skin is small
t
t
o
o
p
p
r
r
o
o
d
d
u
u
c
c
e
e
c
c
o
o
h
h
e
e
r
r
e
e
n
n
t
t
s
s
h
h
e
e
e
e
t
t
s
s
t
t
h
h
a
a
t
t
c
c
a
a
n
n
b
b
e
e
t
t
r
r
a
a
n
n
s
s
f
f
e
e
r
r
r
r
e
e
d
d
a
a
s
s
a
a
p
p
u
u
r
r
e
e
e
e
p
p
i
i
t
t
h
h
e
e
l
l
i
i
a
a
l
l
a
a
u
u
t
t
o
o
g
g
r
r
a
a
f
f
t
t
o
o
r
r
a
a
l
l
l
l
o
o
g
g
r
r
a
a
f
f
t
t
supply for extensive third degree burn.
In vitro cultivation and serial culturing of keratinocytes make production of
viable epithelium sheet possible. Cultured epithelium alone, however dose not
provides mechanically and aesthetically satisfactory long term coverage.
Plastic surgery
Dr.Muslim Kandel 2019-20
9
Full thickness skin graft
Partial thickness skin graft
- Other tissues grafts
Other tissues can also be transferred as grafts.
--Bone grafts
The outer table of the skull, the ribs, and the iliac crest are preferred donor sites.
Acute bone grafting is never performed in the mandible, where it is accompanied by a
high incidence of infection
--Cartilage grafts are commonly used in nasal and ear reconstruction. Cartilage is an
avascular tissue; survival of transplanted chondrocytes depends entirely on diffusion of
nutrients
.
--Vessels, Nerve, tendon, , fascia and cornea are also all in common use.
To reduce failure rate of graft should be :-
1---Graft take is only possible at well-vascularised recipient sites.
So Grafts will not take on bare bone, bare tendon or cartilage, but can survive
on periosteum, and perichondrium.
2—fixation of The graft must remain adherent to the bed until it revascularises;
Meticulous care with suturing and dressings is essential. Where grafts are applied
over mobile areas appropriate splintage must be used.
3--- elevation of Limbs that have been grafted to reduce venous pressure during
the process of revascularisation.
4---Haemostasis at the recipient site must be good to prevent bleeding beneath the
graft resulting in its elevation by clot and failure of take.
5 -- avoid infection excessive contamination with bacteria will prevent take.
Streptococci at levels above 10 5 m.o/g of tissue will result in graft loss.
6-- do multiple small incisions at skin graft to increase area & drain any
serous fluid under graft
7--dressing of both recipient & doner areas , open dressing of graft after 5
days while donar after 2 weeks
8--- Skin grafts can be stored in a refrigerator at 4 0 C for 2 weeks for delayed
application.
Terminology
autograft
is tissue transferred from one location to another on the same patient.
Plastic surgery
Dr.Muslim Kandel 2019-20
10
isograft
is tissue transferred between two genetically identical individuals, such as
the first successful renal transplant that was between identical twins.
allograft
is tissue transferred between genetically different members of the same
species. Most solid organ tissue transplantation involves this type of transfer.
Rejection of the transplanted tissue will occur unless immunosuppressant drugs
are used.
xenograft
is tissue transferred from a donor of one species to a recipient of
another species. Xenografts are usually small amounts of tissue rendered acellular
before implantation to prevent rejection
B- Flaps
Flaps can consist of skin only, or be complex composites of skin, muscle, bone or
other tissues.
Classification:-
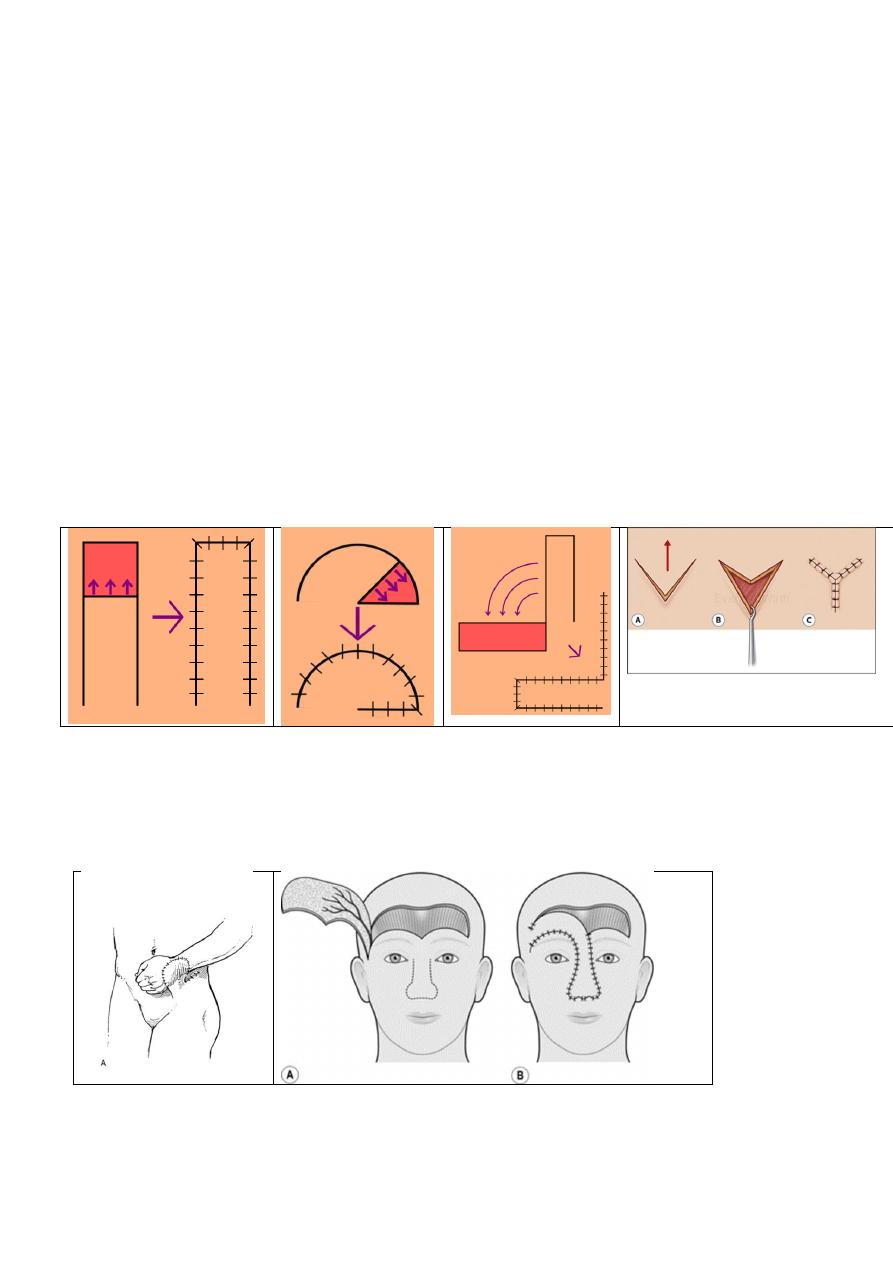
1- Random pattern flaps
Depend on subdermal plexus of blood vessels. These flaps are widely used for
local repair of adjacent defects, Z-plasty or V-Y plasty a combination of Z-
plasties can lengthen a contracture,
2-Axial pattern flaps
Skin flaps with a known direct superficial vascular pedicle passing along their
long axis are known as axial pattern flaps.
The forehead flap , the deltopectoral flap and groin flap all share this vascular
pattern.
3- Muscle and musculocutaneous flaps
Many muscles also have perforating vessels passing from their substance into the
overlying
skin
enabling
musculocutaneous
flaps
to
be
designed.

Plastic surgery
Dr.Muslim Kandel 2019-20
11
Musculocutaneous flaps based on the latissimus dorsi and rectus abdominis
muscles are particularly useful in breast reconstruction.
Gluteus maximus and tensor fascia lata flaps are used for pressure-sore closure.
4- Free tissue transfer
The first successful microsurgical free tissue transfer was a toe transfer to
reconstruct the thumb.
5- Tissue expansion
a silicone balloon is placed beneath the planned donor site. The balloon is then
inflated by percutaneous injections of saline over several weeks in order to
increase the area of the expanded flap
Surgical managing of burn
Classification of burn
1- partial thickness burns which involve epidermal and Superficial dermal layer of skin
2- Deep dermal burns These have lost all adenexal structures.
3- Full-thickness burns which involve all layer of skin
Types of burn
I - Extreme thermal burn
1- by heat
A) Scalds Hot water or boiling water (100 C) or steam ,the severity of burn is depend on
temperature & duration of contact.
B ) Fat burns its more damaging than boiling water because has a much higher
temperature (180 0 C)
C ) Dry (Flame or fire) burns , may be associated with inhalation injury
2-Cold injury
--Frostbite is due to prolonged exposure to extreme cold weather , usually associated with
ischemic damage due to vasoconstriction
--liquid nitrogen LN2. nitrogen in a liquid state at an extremely low temperature , used in cryotherapy
II - Physical Burn
1- Electrical burns depend on – heating result & voltage:
--Low voltage (<1000 V) (240 V, 50 Hz) may induce cardiac arrest, but no deep tissue damage
---High -voltage burns (>1000 V) cause damage by two mechanisms:
1- flash from an arc 2- current transmission which causes deep damage
2- Friction burns induce a combination of heat and abrasion.
There is generally a superficial open wounds that may progress to full-thickness skin loss
3-Ionising radiation
X-irradiation may lead to tissue necrosis. The tissue necrosis may not develop immediately
III - Chemical burns
can causes
local effect Tissue damage depends on:-
--the strength ,the quantity of the agent & the duration of contact. , and sometime also have
systemic effects (e.g. liver and kidney damage with tannic, formic and picric acids).
Plastic surgery
Dr.Muslim Kandel 2019-20
12
Assessment of burn
a) of surface area of the burn (rule of nines) divided body into 11 areas (each one regard 9% of
TBSA) Head 1, chest 1, abdomen 1, each upper limb 1, back 2, each lower limb 2 =99%
+genitelia 1%
b) depth of burn
1- Superficial burns look red, painful, sometime blisters present
2- Deep burns may be blistered and have a blotchy red appearance
with no capillary return on pressure and absent sensation to pinprick.
3- Full-thickness burns have a white or charred appearance; sensation is absent
surgical intervention in burn:
Early intervention
1-Non burn surgery (for associated injuries) e.g. tracheostomy,( in case dyspnea due to
inhalation hot gases cause upper air way obstruction) fracture fixation. associated injury
2- Esharotomy: in circumferential burn ( when cause compartment syndrom ) the eshar
which formed from burn my cause increase pressure by odema which affect blood
supply of limb. So excised eschar (escharotomy) should done, to save limb from necrosis
which can be done without anesthesia in patient room.
3- Fasciotomy: done especially in case of electrical burn., same like eshar but for deep fascia
4- Excision and wound debridement and covered by skin graft •
--late intervention of burn are contracture , alopecia ,
after healing of burn wound with fibrosis , contraction of fibrous tissues may cause
deformity and limitation of joint , Marjolin ulcer & complicated scar may occur
so removal of scar and cover the defect by skin graft, flap , V-Y plasty , Z – plasty
Plastic surgery
Dr.Muslim Kandel 2019-20
13
Lecture three
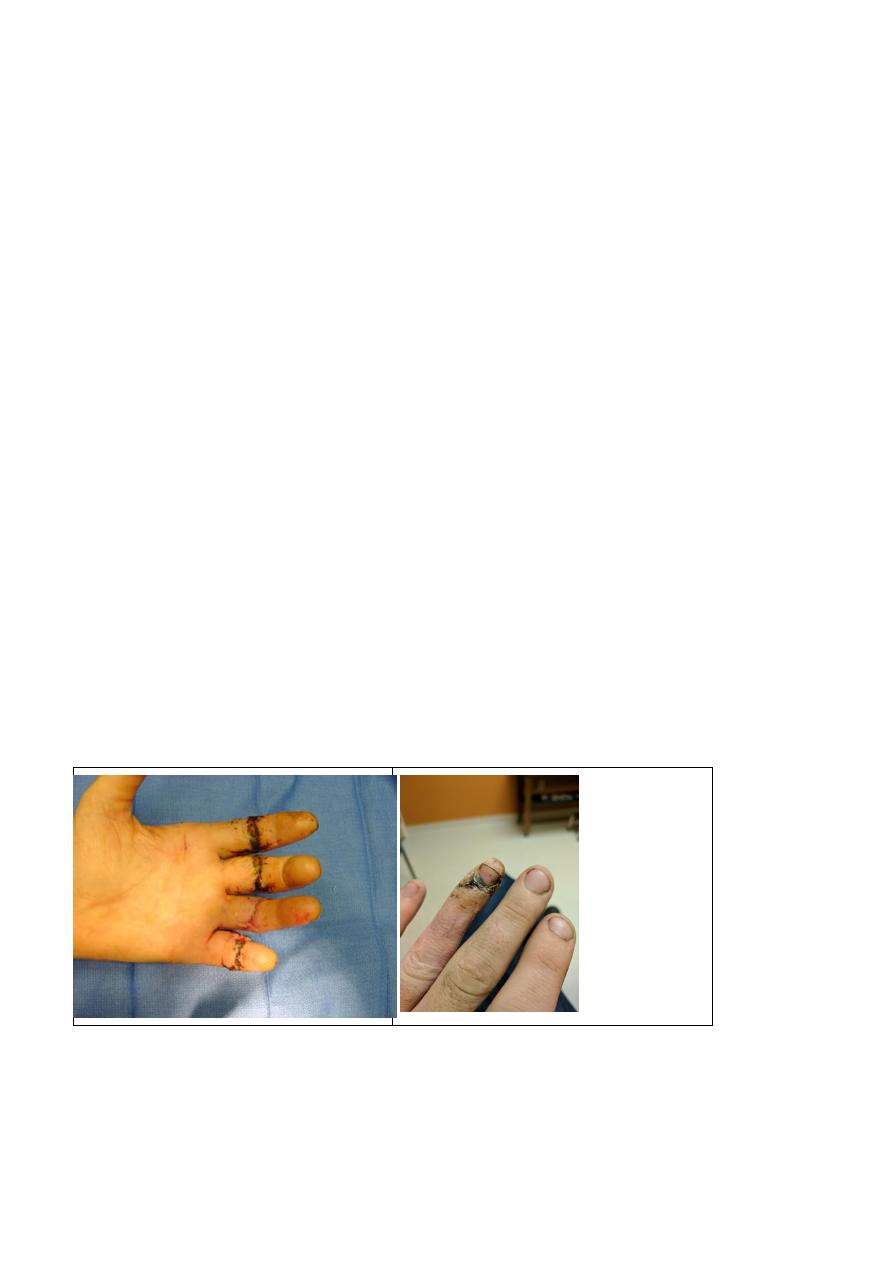
Hand injuries
--blunt trauma,
--sharp trauma (pentrating )
--Other injuries include nail injuries, finger injuries, finger infection
skilled hand surgeons can sometimes reattach the finger or thumb using microsurgery.
. Plastic surgeons and orthopedic surgeons receive significant training in hand surgery
care for hand injuries initially involves proper first aid techniques.
- Lacerations (cuts)
Apply pressure to the wound to stop bleeding.
wash dirt or debris from the wound.
daily dressing for secondary healing
- Fractures (broken bone) and dislocations Immobilize or splint the hand,
- Soft tissue injuries with tissues loss substitute the loosed tissues with graft or flap
-Treatment options of amputated part
cover the amputated body part, (finger or thumb) near ice to cool. Do not place body part in
direct contact with ice in order to prevent freezing.
3 options either -- replantation or-- amputation or -- Transimpantation
1--- replantation. The ideal reconstruction for an amputated thumb is replantation.
Amputation of many fingers at all levels except the most distal deserves an attempt at
replantation. From inspection of the parts it may be difficult to determine which will survive or
which will be the most functional.
multiple replanted fingers in the well-motivated patient usually function better than single
2--- amputation of single finger - V- shape, finger incision with resection of
head of metatarsal bone, approximation of adjacent finger ( which is hindered
by head of metatarsal ) give better shape & function

Plastic surgery
Dr.Muslim Kandel 2019-20
14
3-- transimpantation amputation of thumb , can use in some centers , big toe
transimpantation
Success in revascularizing of the amputated part depends to a large degree on the mechanism of
injury
-- in Clean, guillotine amputations success excess of 90 %
--While in crushing amputations, widens the zone of injury increasing the risk of vascular
thrombosis .and failure
Functional results are dependent on the mechanism of injury, rehaplitation , the age and
motivation of the patient. Young patients will regain more motion than old patients.
Which injuries require replantation:
1-all thumb amputations
2-multiple amputated digits
3-all children
4-all amputations proximal to the digits
5-single digits proximal to the FDS insertion
Strong contraindications:
1-significant associated injuries to the torso and head.
2-extensive injury to the affected limb or to amputated part (degloving, widespread crush)
3-severe chronic illness precluding transportation or prolonged surgery
Relative contraindications:
--Single digit amputation, esp distal to insertion of FDP
--avulsion injuries
--severe degloving injuries
--previous injury or surgery to the part
--extreme contamination
--lengthy warm ischaemia >8hrs (at 4 degrees C >30 hrs)
--age
poor rehabilitation potential
--
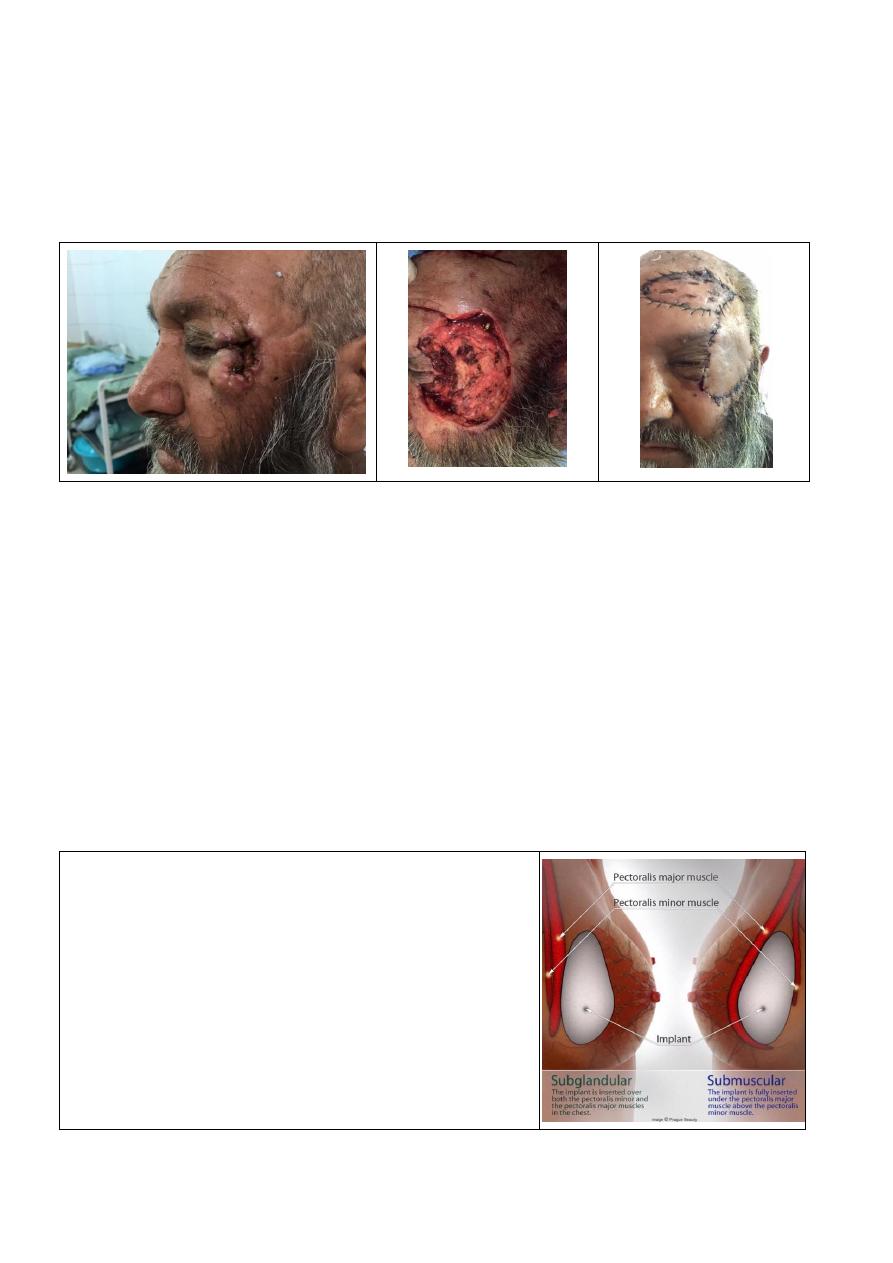
Facial reconstruction
Eyelid
Lower lid Loss of up to 25 per cent of the lid may be reconstructed by primary closure, which
must be carefully maintain lid function.
For defects affecting more than 50 per cent of the lower lid, the lateral incision may be
continued down to the preauricular area to rotate a large cheek flap.
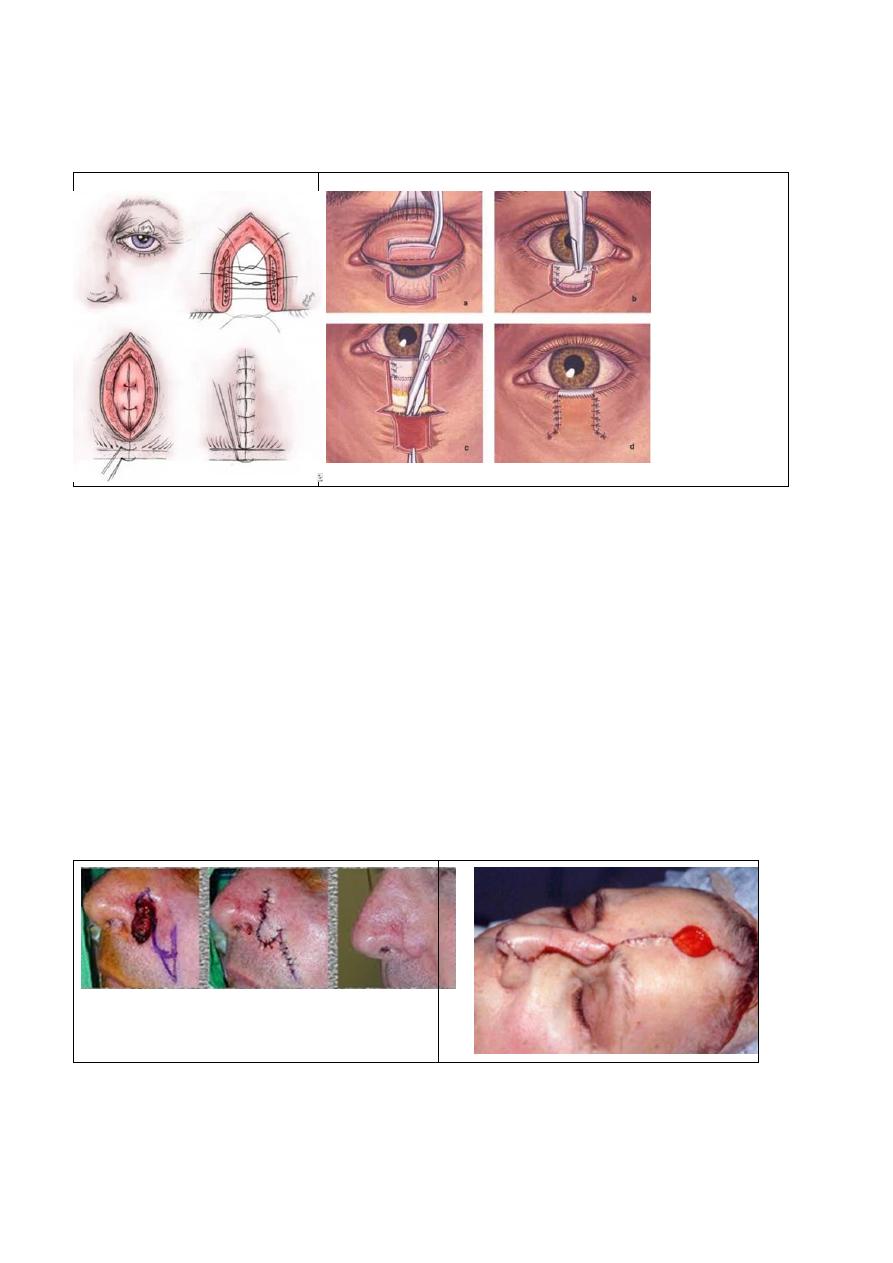
Plastic surgery
Dr.Muslim Kandel 2019-20
15
Upper-lid defects of up to 25 per cent may be closed similarly to lower-lid defects. For larger
defects, tissue is borrowed from the lower lid in the form of a cross-lid flap.
The lacrimal punctum of the lower lid should be preserved,
Nose(reconstruction )
A )Partial reconstruction
1- skin grafts for superficial defects
2-composite graft - graft from the concha of the ear can be used to replace any missing cartilage.
3-- a nasolabial flap.. The flap is based on the branchs of facial artery (angular br)
The flap can be used :-
superiorly to reconstruct defects on the cheek, sidewall or dorsum of the nose, alae, columella
and the lower eyelid.
Inferiorly to reconstruct defects in the upper lip, anterior floor of the mouth
B) Total or Subtotal reconstruction
forehead flap. This procedure is one of the oldest in plastic surgery. A flap based on the
supratrochlear vessels may be turned 180° to cover the nasal structures
Ear reconstruction
Reconstruction of all or part of the ear for either a congenital or a post-traumatic defect requires
a cartilage framework and a thin-flap skin cover. The best source of cartilage graft is the
confluence of the lower costal cartilages
,
some cases use prostheses for cosmetic purposes

Plastic surgery
Dr.Muslim Kandel 2019-20
16
Skin lesions
Benign skin lesions
I-Non-aggressive benign tumors
Papilloma
Fibroma
Lipoma
Neuroma types:
• Ganglioneuroma
• Neuroblastoina
• Neurilemmoma (syn. Schwannoma)
dermoid
Types
--Teratomatous -- sequestrated angular D, -- implantation D at wound , finger
-- congenital postanal
Treatment of benign tumors
All These benign lesions are usually excised as an elliptical incision, which allows a straight-line
closure , The orientation of the ellipse is dictated by wrinkle lines, lines of least tension , primary
closure is required to decrease scar formation
before treatment of angular dermoid should take skull X ray to exclude any connection
with intracreanial structures
II-Treatment of Aggressive benign tumors
Desmoid's tumors
or aggressive fibromatosis can arise from any fascial tissue.
* Surgical resection wide resection is the preferred treatment when it can be accomplished
with minimal morbidity. Positive margins is generally followed by recurrence.
*Irradiation is effective in controlling desmoid tumors if 60 Gy can be delivered.
*The hormonal with progesterone, tamoxifen, indomethacin, and ascorbic acid have all been
reported to induce remissions.
Atypical lipomas and atypical fibrous histiocytomas are generally located deep in the soft
tissue or muscle; they appear atypical histologically and although they do not metastasize they
tend to recur locally after resection, particularly if wide margins are not achieved.
Malignant tumours
1-Carcinomas arise from cells which are ectodermal or endodermal in origin, and they are
classified squamous, basal-celled or glandular (adenocarcinomas).
2-Sarcomas occur in connective tissues with structures of mesoblastic origin, fibrosarcoma,
osteosarcoma.
3-Germ cell tumours arise from germ cells (teratoma, seminoma,).
Management of malignant tumors
Basal-cell carcinoma
The lesions are best excised with intraoperative control of margins. by frozen section is advised.
Should be take save margin , to be sure that removal is complete. Tumor-positive margins after
excision do not invariably mean the lesion will recur, but repeat excision is usually recommended.
Plastic surgery
Dr.Muslim Kandel 2019-20
17
Squamous-cell carcinoma
because invasion into the subcutaneous tissue is possible, the resection should have a wider margin
than is required for basal-cell cancers. Intraoperative examination of the resection margins by frozen
section is advised.
Because of the increased risk of metastasis, the draining lymph nodes should be palpated for
enlargement. addition to the primary resection.
Melanoma
Melanoma is excised with a wider margin than squamous-cell carcinoma. A margin of 1.5 cm is
recommended on the face near vital features; a margin of 3 cm is recommended elsewhere.
-- adjunctive treatments irradiation, chemotherapy, and immunotherapy, none has been successful.
Early detection and complete initial surgical resection are the keys to caring for patients with
melanoma.
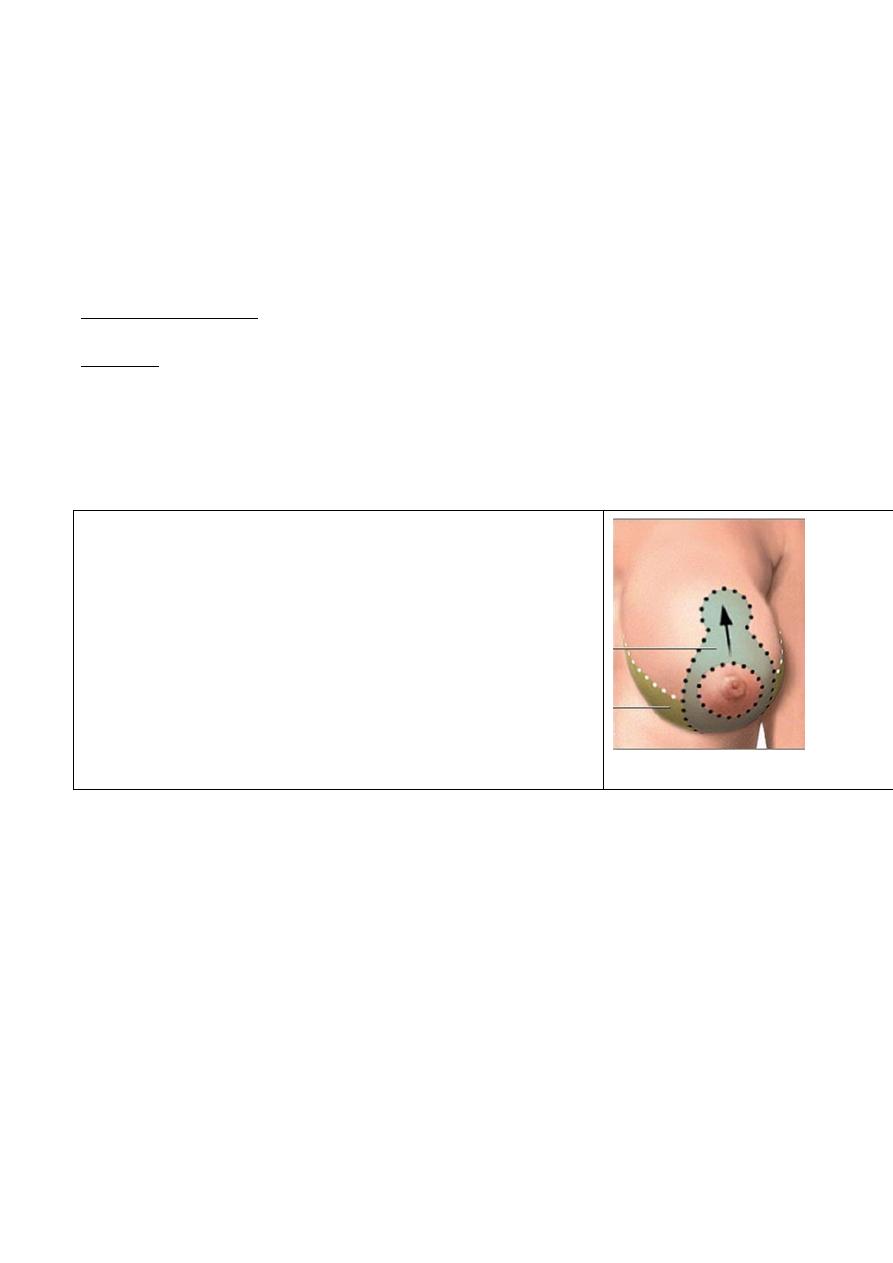
Breast surgery
1- Augmentation
increase the size, change the shape, and alter the texture of the breasts of a woman. by placement
of an implant behind the mammary tissue or behind the subjacent pectoral muscle.
The indications for the procedure are the cosmetic interests of the patient or marked asymmetry due
to dystrophy of one breast
The operation. The route of access is through an incision
either in the areola ,or just above the inframammary crease, or
within the axilla.
The a pocket carried down to a plane (for emplant ) either
under the pectoralis major and above the pectoralis minor
muscles (submuscular) over pectoralis major under breast
glands (subglandular ),
Implants used usually Silastic outer envelopes filled with
either a gel of the same material or with saline.
Plastic surgery
Dr.Muslim Kandel 2019-20
18
complications
1- the breast become rounder and firmer than desired because capsule contraction around the
implant,
2- decreased nipple sensation
,3- hematoma formation within the pocket,
4- a hypertrophied scar at the incision,
2-Reduction (
mastopexy)
reduction mammoplasty :- is procedure for reducing the size of large breasts either to alleviate
these symptoms and or to improve the appearance
mastopexy is procedure to correct breast ptosis is not indicated by medical cause or physical
reason, but by the self-image of the woman;
Large breasts may cause:-
1--neck and back pain,
2--grooving of the shoulders from the brassiere straps,
3-- intertrigo.
Operation is remove excess of 300 g per breast. The pattern for
breast reduction is best in a standing position before surgery. The
nipple, with a reduced diameter, is left as an island on the pedicle.
Medial and lateral segments of breast tissue and fat are removed.
A suction lipectomy may be performed to reduce axillary fat. The
flaps of breast so created are tailored to leave symmetric amounts of
tissue on both sides. The incisions are closed in several layers over
suction drains
complications include hematoma, decreased nipple sensation,
hypertrophied scars, asymmetry, and nipple loss due to ischemia.
Patient satisfaction with the change in breast shape and weight is
usually high.
3- Reconstruction
A breast reconstruction after mastectomy is not a necessity since adequate external prostheses are
available. However, the convenience and appearance of the reconstructed breast are superior.
The operation may be performed immediately after the mastectomy under the same anesthetic, or
at any time in the future.
The early immediate procedure has the advantage of saving a later operation and perhaps in
shoring up the patient's psyche. It should preserves more of the native breast skin ,
The delayed operation may give more time to decide which type of reconstruction, prevention of
complications ,may required postoperative radiation or chemotherapy.
---The early procedure is simplest breast reconstruction ,either use implant of transposed
myocutenous flap
the implant placed in a submuscular pocket, similar to augmentation. But in contrast to
augmentation, the pocket is created completely beneath muscle (pectoralis major, serratus
anterior, and rectus abdominis) to protect the implant from overlying flap necrosis and to
minimize scar capsule contraction. ,to early recognize any recurrence of tumor, also
d
d
o
o
n
n
e
e
i
i
n
n
2
2
s
s
t
t
e
e
p
p
s
s

Plastic surgery
Dr.Muslim Kandel 2019-20
19
1
1
-
-
u
u
s
s
e
e
i
i
m
m
p
p
l
l
a
a
n
n
t
t
e
e
x
x
p
p
a
a
n
n
d
d
e
e
r
r
(
(
w
w
h
h
i
i
c
c
h
h
i
i
s
s
i
i
n
n
j
j
e
e
c
c
t
t
f
f
l
l
u
u
i
i
d
d
g
g
r
r
a
a
d
d
u
u
a
a
l
l
l
l
y
y
t
t
o
o
p
p
r
r
o
o
d
d
u
u
c
c
e
e
a
a
p
p
p
p
r
r
o
o
p
p
r
r
i
i
a
a
t
t
e
e
p
p
o
o
c
c
k
k
e
e
t
t
f
f
o
o
r
r
i
i
m
m
p
p
l
l
a
a
n
n
t
t
)
)
2
2
-
-
r
r
e
e
m
m
o
o
v
v
a
a
l
l
o
o
f
f
e
e
x
x
p
p
a
a
n
n
d
d
e
e
r
r
a
a
n
n
d
d
i
i
n
n
s
s
e
e
r
r
t
t
t
t
h
h
e
e
i
i
m
m
p
p
l
l
a
a
n
n
t
t
The ellipse of skin resected in the mastectomy may be replaced by a transposed island
myocutaneous flap from latissimus dorsi with an implant placed under the pectoralis major.
Complications
1- A larger and more ptotic breast when compared with opposite breast
2- There is little functional deficit from the transposition of the muscle. The anterior fascia of the
rectus abdominis superior to the arcuate line is partially or completely resected, which results in
some laxity of the abdominal wall; this defect can be supported with a patch of synthetic mesh.
3- The blood loss from the rectus abdominis is an extensive
---The delayed procedure resected skin can also be 'replaced' by skin expansion before implant
placement. This procedure has the advantage of providing additional skin without requiring a new
donor site. At the initial operation a Silastic envelope with a subcutaneous filling portal is inserted.
After surgery, saline is injected through this portal at weekly or biweekly intervals.
1 to 3 months after the placing of the expander, a permanent implant is sited in the expanded
pocket, with some attempt to create an inframammary crease. If the opposite breast is large or
ptotic, final symmetry is enhanced by performing a mastopexy or breast reduction on that side.
This operation is done at the time of breast reconstruction, or at a later date to maximize symmetry.
4-Subcutaneous mastectomy
The breast tissue may be removed with preservation of the entire breast skin and nipple in . The
indications is removal of the breasts with premalignant disease. Also the treatment of benign
breast disease and gynecomastia
The operation is performed in a similar manner to breast reduction. The nipple is maintained
primarily by a superior pedicle and the breast is degloved through an incision in the inframammary
crease.
Gynecomastia
Hypertrophy of the male breast
Causes :-
1- Idiopathic In adolescence usually resolves spontaneously in several years.
2-hormonal ;- either increase of esterogen due to gonadal problems or tumours or non
gonadal diseases ( liver , lung , adrenal)
3- drug :- hormonal , cimitidin , digitalis
4- Klinfelter syndrome
5- breast tumour :- Unilateral breast enlargement in older men should be biopsied
because of the rare occurrence of male breast cancer.
Plastic surgery
Dr.Muslim Kandel 2019-20
20
Lecture four
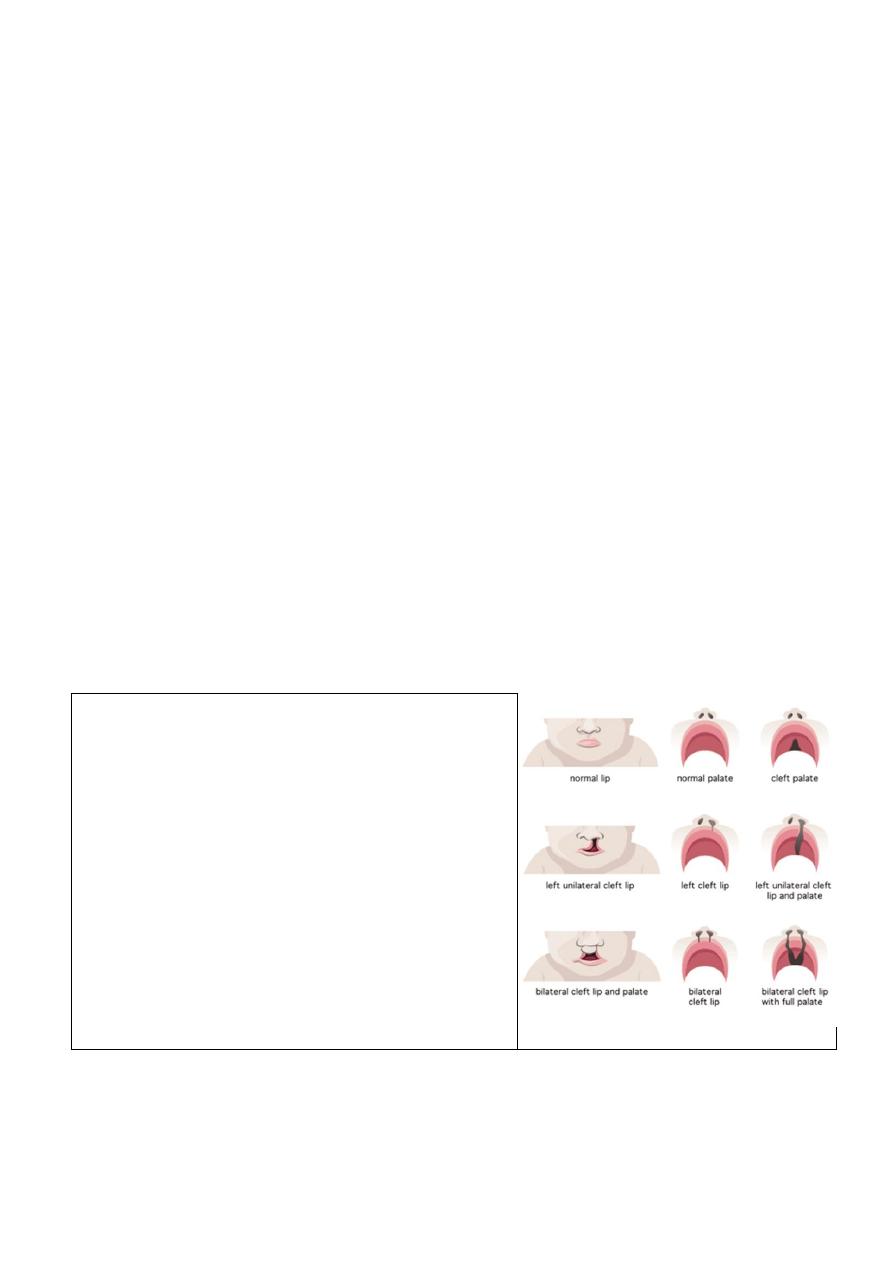
Cleft lip and palate
Anatomy & embryology of hard and soft palat
The roof of mouth cavity formed from Hard & soft palats
Hard Palate formed 2 Bones(Horizontal Bones:
1-Maxilla( Palatine Processes) 2-Palatine Bones
Soft Palate
Fibromuscular shelf attached like a shelf to posterior portion of hard palate
Normally, Five primitive tissue lobes grow in the 2nd and 3rd months of pregnancy
One Frontonasal Prominence grow downward
two Maxillar Prominence meet first lobe to form upper lip
two Mandibular Prominence fuse to form lower lip
But in babies with cleft lip and cleft palate, the fusion never takes place or occurs only part way,
leaving an opening (cleft
.
Risk factors :
No one knows exactly what causes clefts. Its believe due to factors from genetics or the
environment
The incidence of cleft lip and palate is one in 600 (1:600) live births,
1-famelial , family history of cleft lip and palate in which the first-degree relative
2-racial : - caucasian and Iceland have high incidence than nigros
3- Environmental factors during pregnancy include :
mother not getting enough nutrients, such as folic acid
Having DM before pregnancy.
Taking certain medicines, such as some for epilepsy,.
obesety during pregnancy.
Having certain infections during pregnancy, such as rubella (German measles).
The typical distribution
of cleft types is:
• cleft lip alone — 15 %
• cleft lip and palate ------45 %
• isolated cleft palate — 40 %.
Cleft lip/palate predominates in males whereas cleft
palate alone appears more common in females. In
unilateral cleft lip, the deformity affects the left side in
60 % of cases.
Effect upon function
1- sucking and eating more in clift palat
2- speech unable tomake conistant sound (k,g, p,b, ,d,t)
3- teeth
4- nose due to contamination with oral organisim
5- hearing problem due to repeated inf acut or chronic
Otitis Media
6- Airway Problems airway distress from tongue
becoming lodged in palatal defect
Antenatal diagnosis
An antenatal diagnosis of cleft lip, whether unilateral or bilateral, is possible by ultrasound scan after
18 weeks of gestation.
management
A craniofacial team is routinely used to treat this condition to provide patients with comprehensive
multi-disciplinary care from birth through adolescence.

Plastic surgery
Dr.Muslim Kandel 2019-20
21
1-Primary management (pre-surgical advice)
Feeding
they cannot create adequate negative intra-oral pr to be able to express the milk from the breast or
bottle , Simple measures, such as :- enlarging the hole in the teat, and position of feeding
. nursing the baby change positions of feeding untile you find one which works , nipple needs to
stay on the back of the tongue
For cleft plates difficult feeding so use cup and spoon feeding, and palatal obturator (a prosthetic
device made to fit the roof of the mouth covering the gap).
Airway
Intermittent airway obstruction is more frequent during sleep and feeding can be life threatening. and
managed by:-
--nursing the baby prone.
--nasopharyngeal intubation ’ to maintain the airway in more severe cases
Strapping
To reduce the distance of defect with growing
Latham appliance One of the new innovations of cleft lip and cleft palate repair is surgically
inserted by use of pins during the child's 4th or 5th month. After it is in place, the doctor, or parents,
turn a screw daily to bring the cleft together to assist with future lip and/or palate repair
2-The Surgical management
There have been many different surgical techniques and sequences advocated in cleft lip and palate
management.
--Cleft lip repair (Millard operation )is commonly performed between 3 and 6 months of age, (skin
flaps done then reconstruction of orbicularis oris )
-- cleft palate repair is frequently performed between 6 and 18 months, Cleft palate closure can be
achieved by one- or two-stage palatoplasty.V-Y plasty and 4 flaps
3-Secondary management
Following primary surgery, regular review by a multi-disciplinary team is essential. Many aspects of
cleft care require long-term review.
Hearing
should undergo regular audiological assessment before 12 months of age , if sensorineural hearing
loss is managed with a hearing aid,
Speech
Initial speech assessment should be performed early (18 months) and repeated regularly to ensure
that problems are identified early and managed appropriately.
•secondary palatal surgery:
— intravelar veloplasty (muscular reconstruction of soft palate);
— pharyngoplasty;
•speech-training devices.
Dental
delayed tooth development and delayed eruption of teeth; morphological abnormalities
Plastic surgery
Dr.Muslim Kandel 2019-20
22
All children with cleft lip and palate should undergo regular dental examination.
age
0
m
3
m
6
m
9
m
1
y
2
y
3
y
4
y
5
y
6
y
7
y
8
y
9
y
10
y
11
y
12
y
13
y
14
y
15
y
16
y
17
y
1
8
y
Repair cleft lip
Speech
therapy/Pharyngoplasty
Further cosmetic
corrections (Including
jawbone surgery)
Abdominal wall reconstruction(abdomenoplasty)
There are 2 types of abdomenoplasty
1- Large defect of abdominal wall reconstruction after:-
- Trauma
- infection( progressive bacterial synergestic gangrene
-after surgery for cancer, resection of fistulas,
2-Abdomenoplasty for pendulous abdomen Usually after multipregnancy , sever loss of Wt
(mini tummy tucks vs. full tummy tucks)
1- Large defect of abdominal wall
; Knowledge of the vascular anatomy of the abdominal wall allows the design of safe elective
incisions and of appropriate flaps.
should be asses the defect result from trauma or tumor removal, evaluate size of missing
tissues and donor vessels as well as planning for flap transfer depend on the zone defected
methods of reconstruction. Depend on the zone defected :-
Blood supply
territory
Zone
Deep epigastric arcade
Midcentral abdominal wall
above the umbilicus.
I
Epigastric arcade, superficial inferior epigastric,
superficial external pudendal and superficial
circumflex
Lower abdominal wall
below umbilicus.
II
Intercostal, subcostal, and lumbar arteries
Lateral abdominal wall..
III
2-Abdomenoplasty for pendulous abdomen
pendulous abdomen usually result after pregnancy , obesity

Plastic surgery
Dr.Muslim Kandel 2019-20
23
the transverse incision should be low down ,can change position of umbilicus by do island
flap , excise the excess of skin and fat
A good candidate for Abdominoplasty Surgery (Tummy Tucks):
1-Is close to their ideal body weight (within 30%)
2-Wants to remove specific areas of loose skin or fat that is diet- and exercise-resistant
3-Weight has been stable for 6 months or more
4-Has good skin tone and elasticity
5-Has realistic expectations , emotionally stable Understands the risks of surgery
Procedure:-
full tummy tuck involves an incision around the
umbilicus and across the lower abdomen, a mini tummy
tuck leaves the umbilicus intact and requires a smaller
incision.
Liposuction is sometimes employed and the fat is
removed from below the, umbilicus tightening muscles
from the umbilicus to the pubis.
complications:
1-Bleeding,Hematoma
2-Infection
3-Keloid
4-Puckered,skin
5-Seroma
6-Skin irregularities
7-Skin necrosis or skin death (more likely with smokers)
8-Slow.healing
9- wound dehecence
Cosmetic surgery
Cosmetic surgery is surgical procedures, , that are performed only for the improvement in
appearance from an acceptable 'normal' to a more 'coveted normal'.
Who is a Good Candidate?
People who have health conditions such as diabetes, hypertension, lung disease, heart disease,
high cholesterol, arthritis, emphysema, are malnourished, severely depressed, obese and/or
smokers are not generally good candidates for cosmetic surgery.
So the good candidates
1-ideal weight (within 30%),
2- non-smokers, if smoker should stop for at least 2 weeks prior to surgery and remain
smoke-free until at least 2 weeks after surgery,
3-, emotionally stable, with low stress, exercise and maintain a healthy lifestyle.
4-is important to have realistic expectations and not expect plastic surgery to change your life.
A good candidate also accepts the disadvantages of plastic surgery (cost, inconvenience,
discomfort, and medical risk
).
Rhinoplasty
Rhinoplasty is change irregularity of nasal contour ,or after nasal trauma (blunt, penetrating, blast)
Plastic surgery
Dr.Muslim Kandel 2019-20
24
-- performed after the nasal skeleton has matured in adolescence.
Types of rhinoplasty open rhinoplasty or closed rhinoplasty
In open rhinoplasty,
the surgeon makes a small, irregular incision to the columella( fleshy external
end of the nasal septum,).
In
closed
rhinoplasty,
surgeon
performs
incision
endonasally
(exclusivelywithin the nose), and does not cut the columella
Types of rhinoplasty – primary and secondary
primary rhinoplasty reconstructive, functional, or aesthetic corrective procedure.
The midline dorsal prominence osteotome for the bone and a scalpel for the cartilage. The medial
borders of the upper lateral cartilages may require resection as they also produce some dorsal
prominence.
septal deviation, which may interfere with nasal breathing and alter the timbre of the voice. the
mucoperichondrium is elevated from both sides of the septum through an incision in the
membranous septum
secondary rhinoplasty revision of a failed rhinoplasty, 5–20 % of rhinoplasty operations
The corrections usually "open approach", is more technically complicated, usually because the nasal
support structures either were deformed or destroyed in the primary rhinoplasty
Reconstruction rhinoplasty
Reconstruction rhinoplasty is indicated for the correction of defects and deformities caused by
Skin cancer. The most common cause for a nasal reconstruction melanoma and BCC
Traumatic nasal defect. Less common blunt (impact),penetrating and blast trauma.
Congenital deformities. Cleft lip and palat
.
Liposuction (lipoplasty)
is the surgical process by which a plastic surgeon removes very stubborn fat from a person's body ,
and sometime reinjected to another areas of body
Liposuction can be performed on many parts of the body including the stomach, hips, waist, thighs,
arms and also used frequently in conjunction with other operations such as a
, a
and
benefits of liposuction
1--plastic surgeon can removing fat from specific areas of
your body.
2-With liposuction, the normal result is immediate weight
loss, and a slimmer, more contoured shape are the changes
procedures and techniques used in liposuction
makes a very small incision in the skin, and inserts a tiny tube
(cannula) through the skin into the fat layer. The tube is
attached to a vacuum that sucks out the fat.
It may be using general anesthesia or local anesthesia,
Liquification methodes

Plastic surgery
Dr.Muslim Kandel 2019-20
25
- water assisted liposuction (WAL)
- ultrasound assisted liposuction (UAL)
- Laser-assisted liposuction(LAL)
loosening or partially liquefying the fat to make it easier to extract. through a small cannula.
If reinjected fat , so inserted in many test tubes , transfuge then injected in other areas
Side effects of liposection
1-Temporary swelling, bruising, soreness, and numbness.
2-Irritation and minor scarring around the incision sites.
3-Baggy or rippling skin. The skin will usually tighten and retract after a few months. But in some
people the skin may remain somewhat loose.
4-Permanent color changes in the skin.
5-Damage to the nerves and skin.
Serous complications
1-Excessive blood and fluid loss, leading to shock. (rare)
2-Fat clots or blood clots, (pulmonary embolism).
3-(pulmonary edema). This is most likely to occur when a large volume of fluid is injected into the
body.
4-Infection. In some cases, antibiotics may be given before or after liposuction
Blepharoplasty and brow lift
Excess skin in the upper and lower eyelids and periorbital fat can be corrected by a blepharoplasty
or a blepharoplasty combined with a brow lift. The lower lid may have excess or herniated
periorbital fat, even in a young person; this can be a familial characteristic that worsens with age.
Young people will occasionally have a lower-lid blepharoplasty to remove this excess tissue, which
will not reaccumulate until quite late in life. It is performed through a subciliary incision carried out
laterally into one of the laterally radiating wrinkles.
The incision can also be created through the conjunctival fornix. Through the subciliary incision
the skin and orbicularis oculi muscle are elevated as a single flap.
Botox
Botox injections are a diluted form of botulism which paralyzes or weakens the muscles that form
wrinkles. Botox is the most popular non-surgical cosmetic procedure performed
What kind of wrinkles do Botox injections treat?
Botox can safely and successfully treat wrinkles that are caused by muscle contraction. These include
frown lines, forehead creases, crows feet, and neck bands
Results are normally seen within a few days. The results should last 3-4 months
Face lift
Excess facial skin and fat, particularly in the lower face, can be removed or reduced by a face-lift
procedure. Two symmetric incisions are made from the scalp to the preauricular skin to the
postauricular sulcus and into the posterior scalp to allow the elevation of bilateral cheek flaps, which

Plastic surgery
Dr.Muslim Kandel 2019-20
26
are then advanced posteriorly to resect an ellipse of facial and scalp skin and tighten the facial tissues
along a vector parallel to the jawline.
A submental incision may be made specifically to excise submental fat and to excise or suture the
medial borders of the platysma muscle. The supraplatysmal fat within the neck may be removed by
direct excision or by suction lipectomy.
