1
L6 Dermatology D. Alaa
Disorders of Pigmentation
Causes of hypopigmentation
Infection: pityriasis versicolor
Postinflammmatory hypopigmentation: psoroiasis, diaper rash
Pityriasis alba: mild type of atopic dermatitis
Hereditary diseases: piebaldism and oculocutaneous albinism(OCA)
Chemical : rubber
Pharmacological: topical and intralesional steroids
Idiopathic: vitiligo
Vitiligo
It affect 0.5-2% of general population worldwide
Average age of onset is 20 years but any age can be inflicted by this disease
Characterized by absence or decrease of melanocytes reflected by absence or decreased DOPA-
positive melanocytes
Pathogenesis
Genetic:
Environmental:
Autoimmune theory:
Humoral immunity
: association with other auto-immune diseases in particular hypo and
hyper thyroidism in addition to Addison’s , DM etc…
Cellular immunity:
T cells that infiltrate perilesional epidermis are predominantly CD8 T
cells
Intrinsic defects of melanocytes theory:
They found there is a dilatation in rough endoplasmic
reticulum of melanocyes in perilesional skin
Defective free radical defense:
H2O2 overproduction in lesional skin leads to oxidative damage
of melanocytes
Neural theory:
especially in segmental vitiligo. They believe that neuropeptides released from
nerve endings cause decreased melanin production
Viral theory:
cytomegalovirus DNA has been identified in skin biopsy specimen of some patients
with vitiligo, causing damage to melanocytes

2
Clinical Presentation
Present as asymptomatic, non-scaly depigmented macules and patches
Affect mostly face (periorificial), hands, knees, elbows, ankle, nipple, anogenial
Can present as isolated localized patch of grey or white hair (poliosis) or as premature
diffuse graying of hair ( canities)
Classification
Localized
Unilateral (segmental): stop abruptly at the medline
Acrofacial: affect extremities and face
Generalized
Treatment
If less than 20% of BSA is affected by vitiligo:
Topical corticosteroids: first option
Topical immunosuppressant e.g. tacrolimus and topical pseudocatalase
Surgery: punch graft and cultured melanocytes for vitiligo unresponsive to topical Rx
If more than 20% of BSA is affected by vitiligo:
Narrowband UVB(311 nm): first choice
Psoralen plus phototherapy(PUVA): psoralen can be applied topically(topical PUVA) or
oral (oral PUVA) followed by exposure to artificial UV light or natural sunlight.
Excimer laser
Permanent depigmentation: e.g. monobenzyl ether of hydroquinone is used when vitiligo
involve more than 50% of BSA and unresponsive to phototherapy
Others: systemic anti-oxidant
Piebaldism
Autosomal dominant, cc by stable depigmented patches on anterior trunk, mid extremities,
forehead and frontal scalp(white forelock), sparing the back
Present at birth
The involved skin has no melanocytes
Treatment: topical steroid and phototherapy is not effective. Auto graft from normal skin is
successful
3
Oculocutaneous albinism(OCA)
Autosomal recessive group of diseases characterized by diffuse pigmentary dilution due to partial
or total absence of melanin in skin, hair follicles and eyes despite the normal number of
melanocytes in skin
Eyes may be affected by decreased visual acuity, nystagmus and photophobia
Those patient are at increased risk for skin cancer
Treatment is photoprotection, photoprotection and photoprotection
Causes of hyperpigmentation
Infection: Pityriasis versicolor
Drug-induced : amiodarone, minocycline
Postinflammatory hyperpigmentation: lichen planus and fixed drug eruption
Erythema ab igne: net-like hyperpigmentation due to long-term exposure to heat e.g. laptop
on the thighs
Idiopathic: melasma
Melasma
Synonyms: chloasma, mask of pregnancy
It is most prevalent among young to middle aged women
Hispanic, Asian, African or middle eastern descent are inflicted by this disease
Pathogenesis
Exposure to UV : improvement or disappearance of lesion in winter, involvement of sun-
exposed areas and sparing of philtrum
Genetic/ethnic predisposition : Mostly it is related to darker skin type
Hormones: OCP, pregnancy (appearnace or exacerbation)
Autoimmune thyroid diseases
Clinical features
Brown patches on the face, but may affect extensor forearm and central upper chest
May lighten or disappear after delivery in light skinned women
Treatment
Sun protection, sun protection and sun protection
Hydroquinone (tyrosinase inhibitor). Side effects: allergic and irritant contact dermatitis,
ochronosis
Others: Chemical peels: using salicylic acid and glycolic acid and laser
4
Ochronosis
There are two types;
1) Exogenous: due to prolonged application of hydroquinone, and products containing
mercury, resorcinol
2) Endogenous: Autosomal recessive due to mutation in homogentisic acid oxidase.
Macular amyloidosis
Pruritic confluent or rippled hyperpigmented macules and patches
Mostly involve upper back and forearms
Women affected more than men
local friction from nylon brushes, towels and other rough materials contributes to the
production of this disease
Treatment
: breaking itch-scratch cycle , stopping friction e.g. brush use addition to use of
topical steroids plus keratolytics
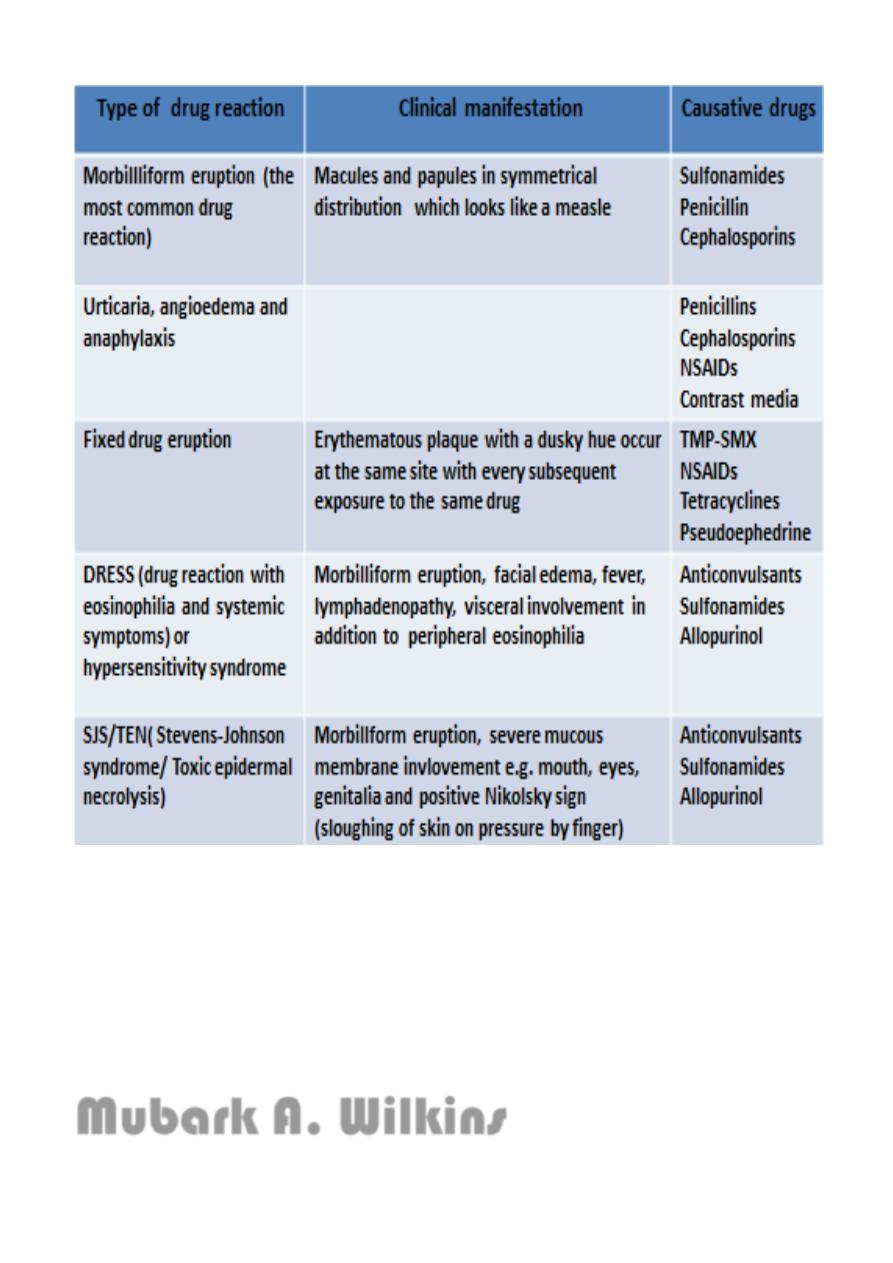
Drug Reactions
Epidemiology
The skin is one of the most common targets for adverse drug reactions
Women are more susceptible than men
Paradoxically, the incidence of most immunologically mediated drug eruptions is increased
in the setting of immunosuppression; for example, in patients with AIDS
The incidence of adverse reactions also increases with the age of the patient
Time interval between drug introduction and skin eruption because most of drug eruption
occurs within 1-3 weeks after initiation of new
Treatment
1. Withdrawal of suspect drug as soon as possible
2. If many drugs are incriminated, stop all non-essential drugs
3. If the suspect drug is essential, substitute with another that does not cross-react
4. For mild drug eruption, start topical steroid and for severe drug eruption such as SJS/TEN
and DRESS, start systemic steroids
Clinical type
5
Note
:
Stevens-Johnson syndrome: if less than 10% of body surface area is involved
Toxic epidermal necrolysis when more than 30% of body surface area is involved
Mubark A. Wilkins
