Genitourinary Prolapse
By
Prof.Dr.Bushra AL-Rubayae

Objectives:
• Definition.
• Risk factors & etiology.
• Clinical presentation.
• Management options.
• Preventive measures.

•Genital Prolapse:
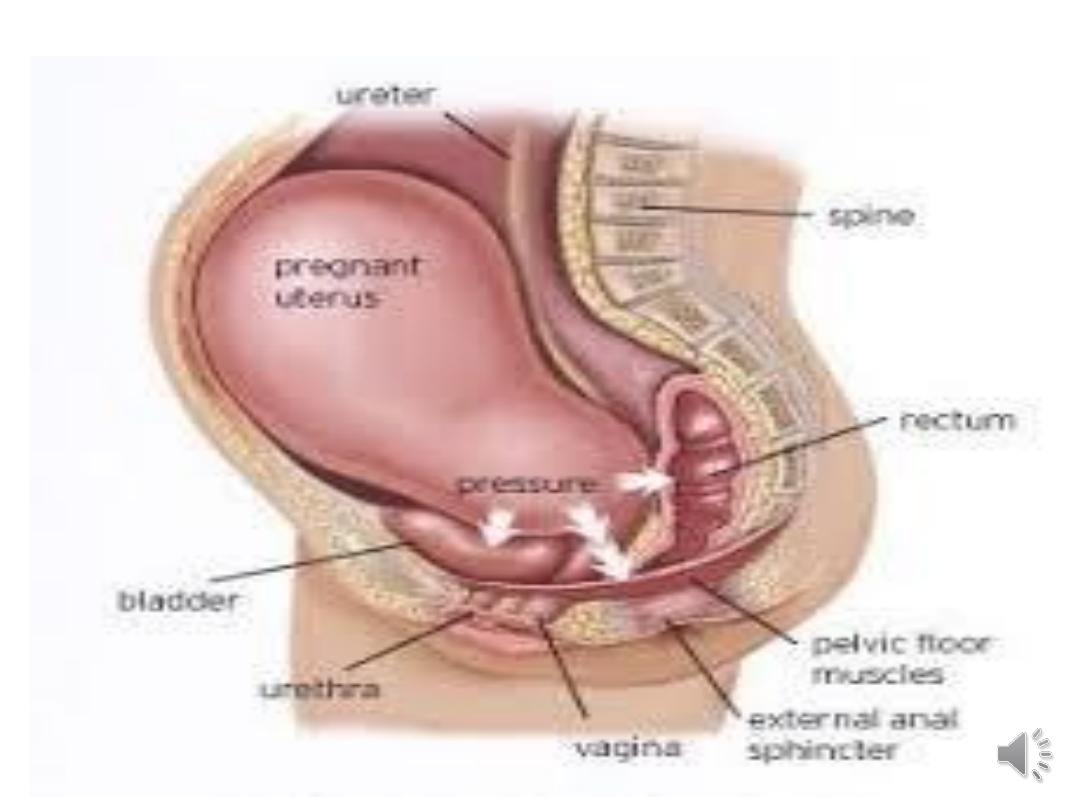
•It occurs when there is descent of one or more of
the pelvic organs including the uterus, bladder,
rectum, small or large bowel, or vaginal vault.
•The anterior and/or posterior vaginal walls, the
uterus and the vaginal vault can all be affected by
this descent.
Resulting in protrusion of the vaginal walls and/or the
uterus. It is usually accompanied by urinary, bowel, sexual,
or local pelvic symptoms.
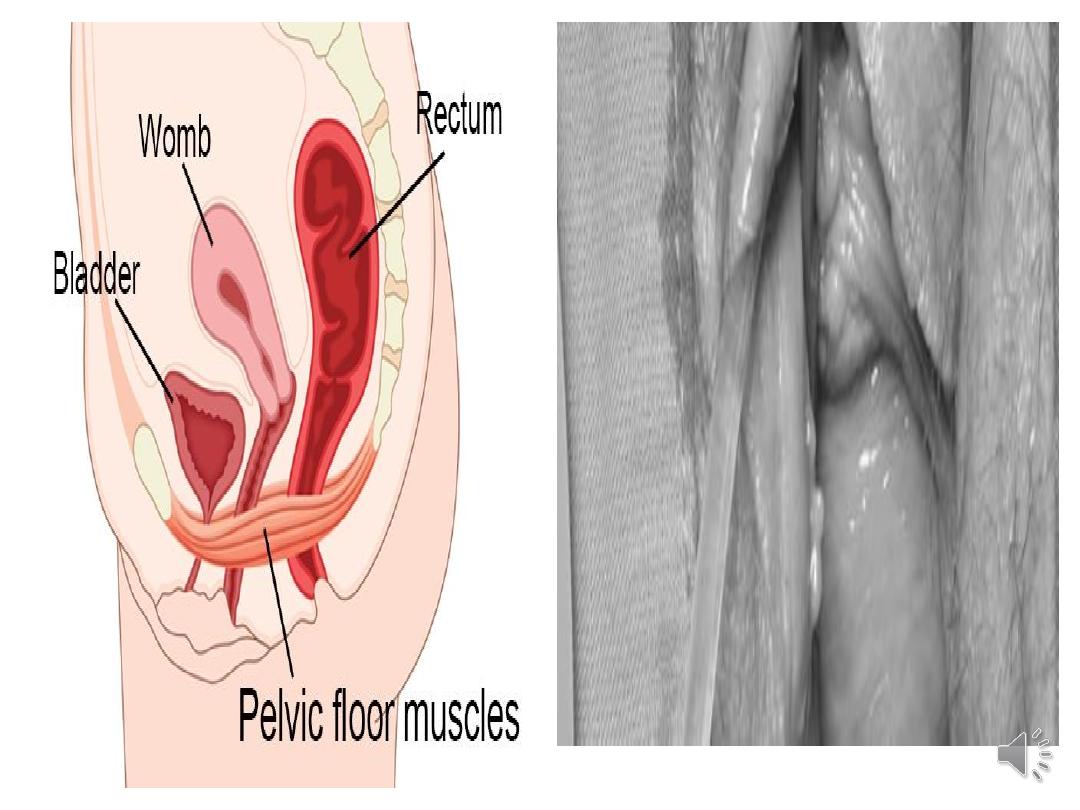
Patho-physiology:
•Pelvic organs mainly supported by the levator ani
muscles and the endopelvic fascia (a connective
tissue network connecting the organs to the
pelvic muscles and bones).
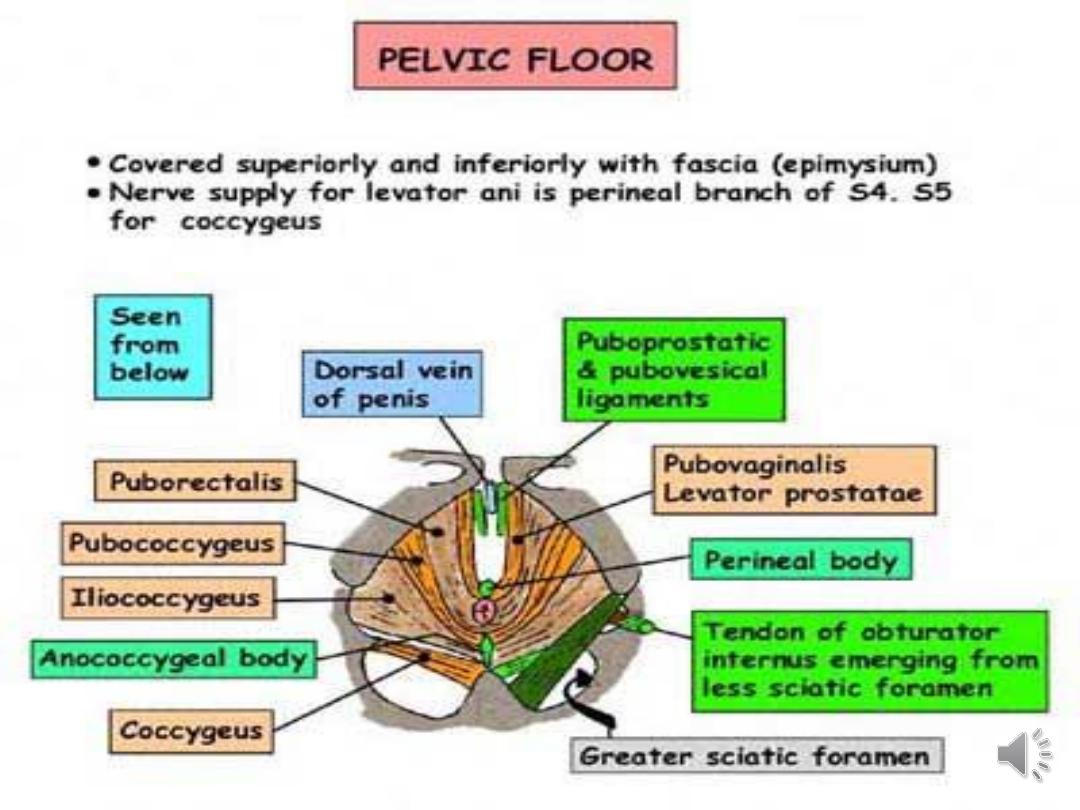
• Prolapse develops when the supporting structure is
weakened due to:
• direct muscle trauma, neuropathic injury,
disruption or stretching of tissue.
•Multifactorial causes for the damage is likely.
•The orientation and shape of bones of the pelvis
have a role in the pathogenesis of genital prolapse.

Confirmed risk factors:
•Increasing age:
risk doubles with each decade of life.
•Vaginal delivery.
•Increasing parity.
•Overweight (BMI 25-30) and
obesity
(BMI >30).
•Spina bifida
and spina bifida occulta.
•
Possible risk factors:
•
Intrapartum Factors (controversial and unproven):
•
Fetal
macrosomia
.
•
Prolonged second stage of labour.
•
Anal sphincter injury.
•
Epidural anaesthesia.
•
Use of forceps.
•
Use of oxytocin.

Age <25 years at first delivery.
•Race.
•Family history of prolapse.
•Constipation
.
•Connective tissue disorders, eg Marfan's
syndrome, Ehlers-Danlos syndrome.
•Previous hysterectomy
.

•Types of genitourinary prolapse
•Prolapse can occur in the anterior, middle, or
posterior compartment of the pelvis:
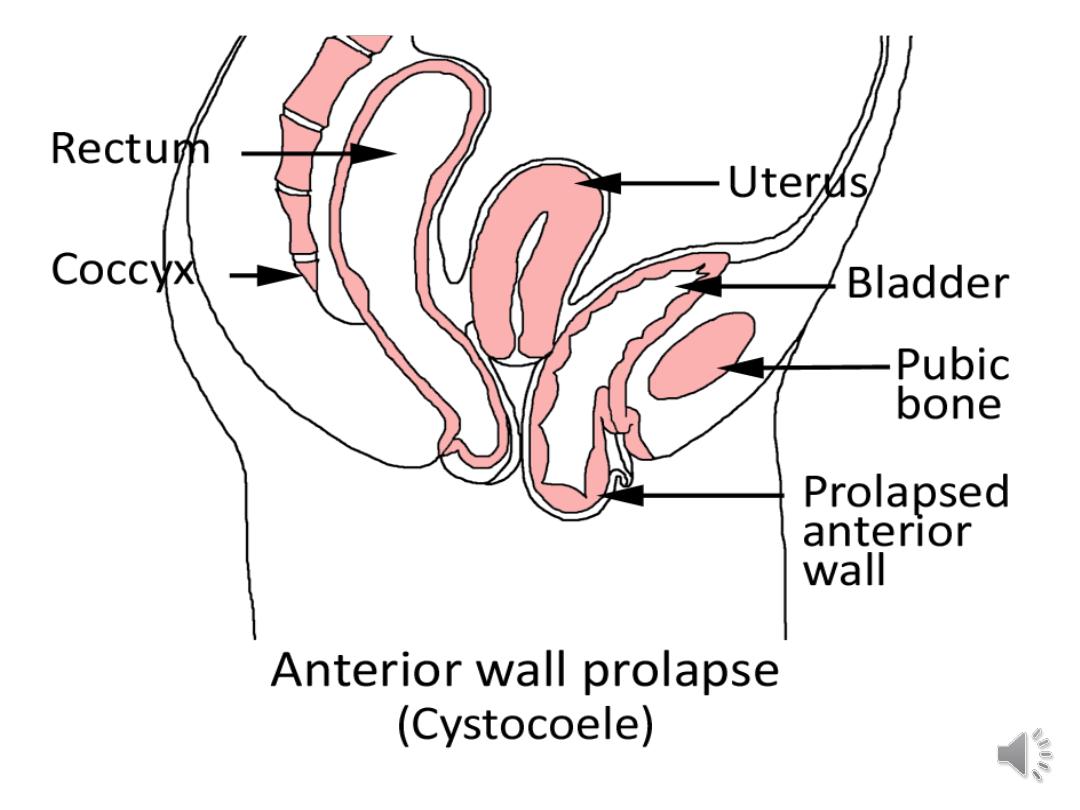
•Anterior compartment prolapse
•Urethrocele: prolapse of the urethra into the
vagina. Frequently associated with urinary stress
incontinence.

•Cystocele:
prolapse of the bladder into the vagina. A
large cystocele may cause increased urinary
frequency, frequent urinary infections and produce a
pressure sensation or mass at the introitus.
•Cystourethrocele: prolapse of both urethra and
bladder.

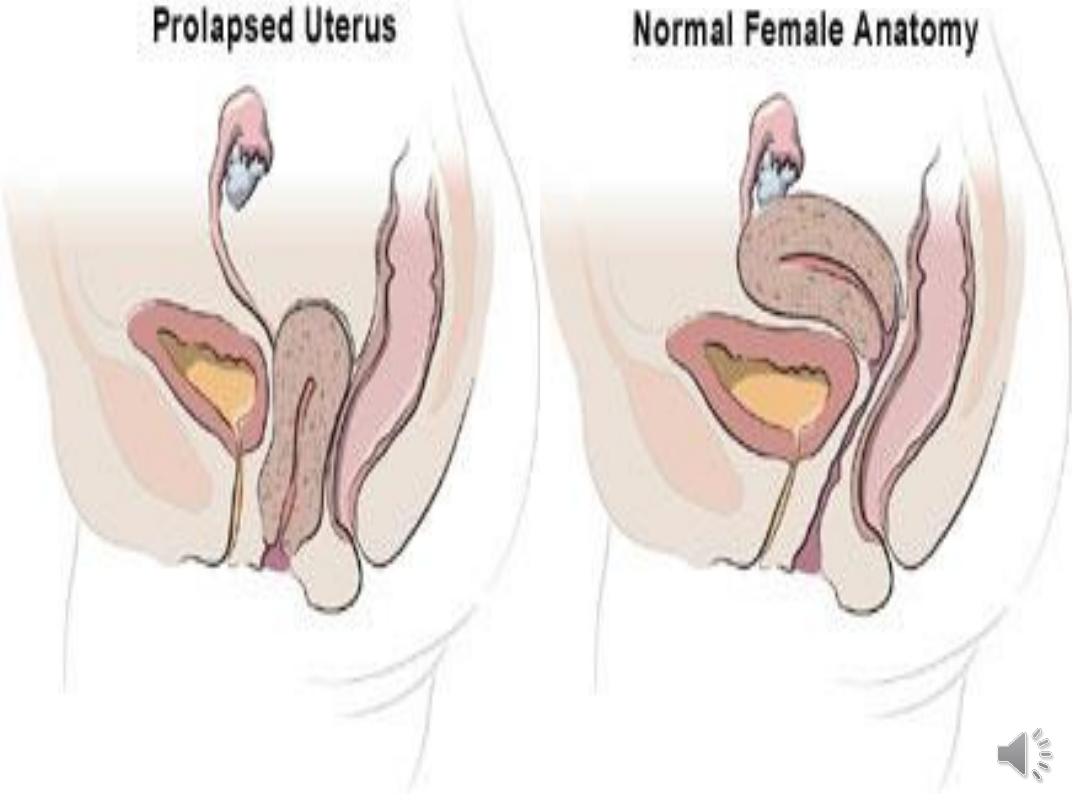
•Middle compartment prolapse
•Uterine prolapse: descent of the uterus into the
vagina.
•Vaginal vault prolapse: descent of the vaginal vault
post-hysterectomy. Often associated with
cystocoele, rectocele, and enterocele. With
complete inversion, the urethra, bladder, and distal
ureters may be included resulting in varying
degrees of retention and distal ureteric
obstruction.


•Enterocele: herniation of the pouch of
Douglas (including small intestine/omentum)
into the vagina.
• Can occur following pelvic surgery. Can be
difficult to differentiate clinically from
rectocele but a cough impulse can be felt in
enterocele on combined rectal and vaginal
examination.

•Posterior compartment prolapse
•Rectocele: prolapse of the rectum into the
vagina.
•Cysto-urethrocele is the most common type
of prolapse, followed by uterine prolapse
and then rectocele. Urethroceles are rare.


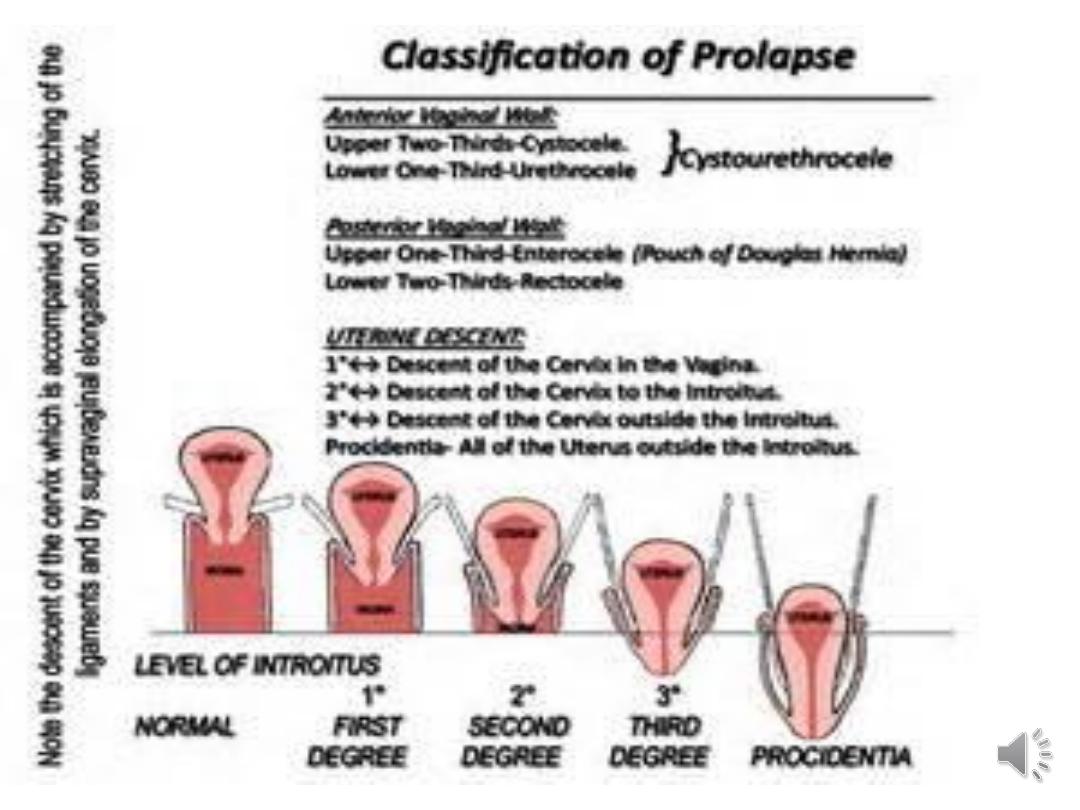
The degree of uterine descent can be graded
as:
•1st degree:
cervix visible when the perineum is
depressed -it is contained within the vagina.
•2nd degree:
cervix prolapsed through the introits with the
fundus remaining in the pelvis.
•3rd degree:
procidentia (complete prolapse) - entire
uterus is outside the introits.

Symptoms:
•It may be asymptomatic and an incidental
finding.
• Sometimes symptoms can severely affect
their quality of life.
•Symptoms are related to the site and type of
prolapse.
•Vaginal/general symptoms can be common to
all types of prolapse.
Vaginal/general symptoms(non urinary)
•Sensation of pressure, fullness or heaviness.
•Sensation of a bulge/protrusion or 'something
coming down'.
•Seeing or feeling a bulge/protrusion.
•Difficulty retaining tampons.
•Spotting (in the presence of ulceration of the
prolapse).

•Urinary symptoms
•Incontinence.
•Frequency.
•Urgency.
•Feeling of incomplete bladder emptying.
•Weak or prolonged urinary stream.
•The need to reduce the prolapse manually before
voiding.
•The need to change position to start or complete
voiding.

Coital difficulty
•Dyspareunia.
•Loss of vaginal sensation.
•Vaginal flatus.

Bowel symptoms
•Constipation/straining.
•Urgency of stool.
•Incontinence of flatus or stool.
•Incomplete evacuation.
•The need to apply digital pressure to the
perineum or posterior vaginal wall to enable
defecation (splinting).
•Digital evacuation necessary to pass a stool.

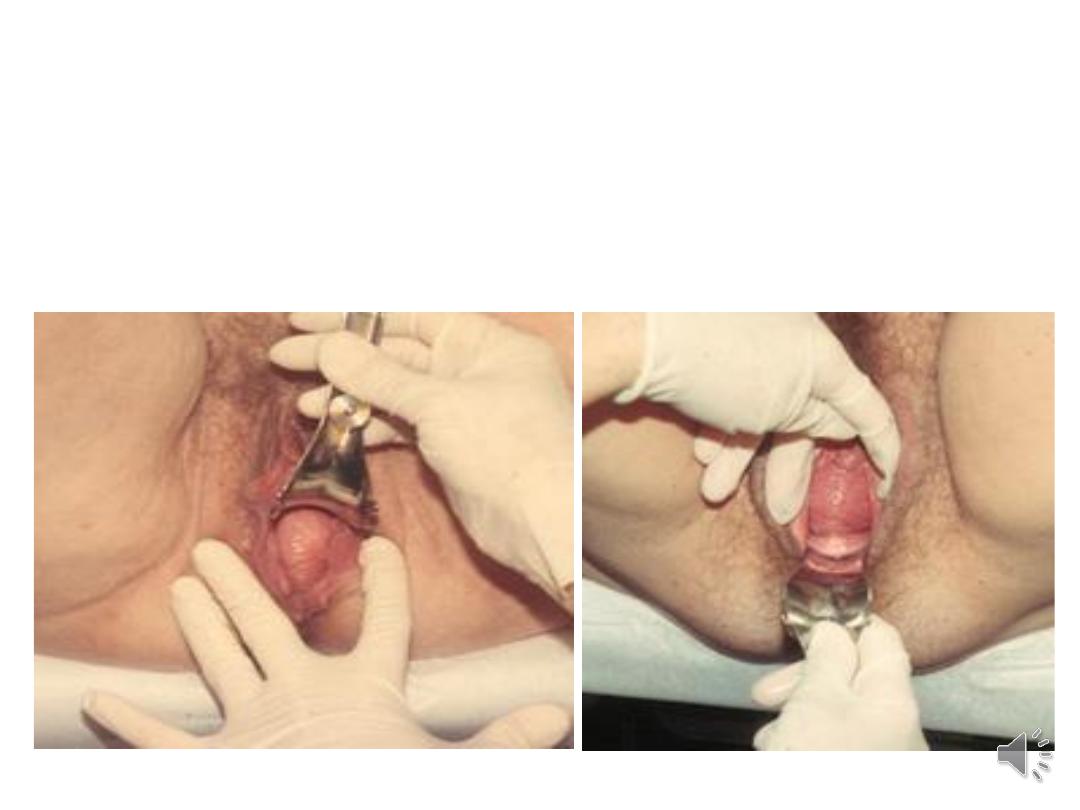
Examination:
•Examine the patient in both a standing and
left lateral position if possible.
•Use a Sims' speculum inserted along the
posterior vaginal wall to assess the anterior
wall and vaginal vault and vice versa. Ask the
patient to strain.
•Uterine descent can be assessed by gentle
traction with a vulsellum.

A bivalve speculum:
can also be used to identify the cervix or
vaginal vault.
Ask the patient to strain, and slowly remove
the speculum.
Look for the degree of descent of the
vaginal apex.
•Determine the parts of the vagina (anterior,
posterior or apical) that the prolapse affects.

Ulceration and hypertrophy of the cervix or
vaginal mucosa with concomitant bleeding may be
seen in women with prolapse that protrudes
beyond the hymen.
•A rectal examination can be helpful if there are
bowel symptoms

•Investigations:
Diagnosis is usually clinical and based on
history and examination.
•If there are urinary symptoms consider the
following:
•Urinalysis ± a mid-stream specimen of urine
(MSU).
•Post-void residual urine volume testing using a
catheter or bladder ultrasound scan.

•Urodynamic investigations:
•Cystometry.
•Urea and creatinine.
•Renal ultrasound scan.
•If there are bowel symptoms consider :
•Anal manometry
.

Management :
• It depends on :
• Age ,Fertility wishes, symptoms & severity.
• Associated factors.
• Options of treatment:
• Conservative treatment.
•
Watchful waiting.
•
Vaginal pessary insertion.
•
Surgery.

•Management:
•No treatment is necessary if incidental
asymptomatic mild prolapse is found.
There is no evidence about how to treat these
women.
• Conservative treatment options:
• Lifestyle modification:
including treatment of cough, smoking
cessation, constipation and overweight and obesity.
• Pelvic floor muscle exercises:
There is no definite evidence for the benefit of
pelvic floor muscle exercises in the management of
uterine prolapse

• . It may be beneficial as primary therapy for early stages
of uterine prolapse.
• Vaginal oestrogen creams:
some advocate a trial of topical oestrogen cream for
4-6 weeks if prolapse is mild but there is no current
evidence of any benefit.

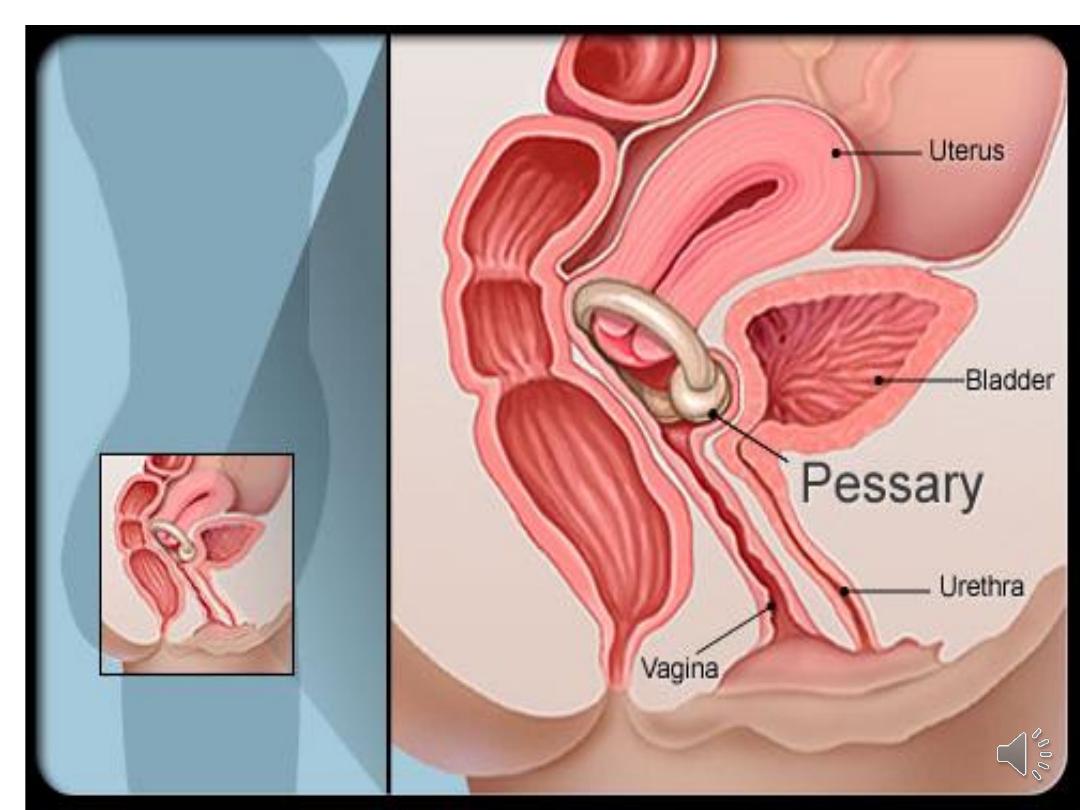
•Vaginal pessary insertion:
A good alternative to surgery.
•Inserted into the vagina to reduce the prolapse,
provide support and relieve pressure on the
bladder and bowel.
•Made of silicone or plastic.

Pessaries are effective:
•- As a test if symptoms due to prolapse.
•- If pregnancy planned.
•For short-term relief of prolapse prior to surgery.
•In the long term if surgery is not wanted or is
contra-indicated.
•Fitting a pessary:
•Ensure the patient's bladder and bowel are
empty
•Perform a
and estimate
the size of the vagina.
•The aim is to fit the largest pessary that does
not cause discomfort.
•Ask the patient after insertion to walk around,
bend and micturate to ensure that the pessary
is retained.

•Surgery
•Surgery is very effective.
•Indications for surgery are:
• failure of pessary.
• patient who wants definitive treatment.
•prolapse combined with urinary or faecal
incontinence.

•Urinary incontinenc
may be masked by prolapse
and can be precipitated by surgery.
•Some operations, eg colposuspension for a
cystourethrocele, may predispose to a prolapse in
another compartment.

•The choice of procedure will depend on:
• whether the woman is sexually active.
•Not complete family.
• the fitness of the patient.
• and surgeon's preference.

•Types of Surgery:
•Vaginal Operation:
•Ant., Post. Repair, Vag. Hysterectomy.
• TVT, TOT.
•Abdominal :
•Laparoscopic.
•Colpo-suspension, sling operations.
•Oblitrative:
•Advice Post operative:
•If the prolapse remains corrected and the patient
conceives, an elective
may be
advisable.
•Generally women should avoid heavy lifting after
surgery and avoid sexual intercourse for 6-8 weeks.

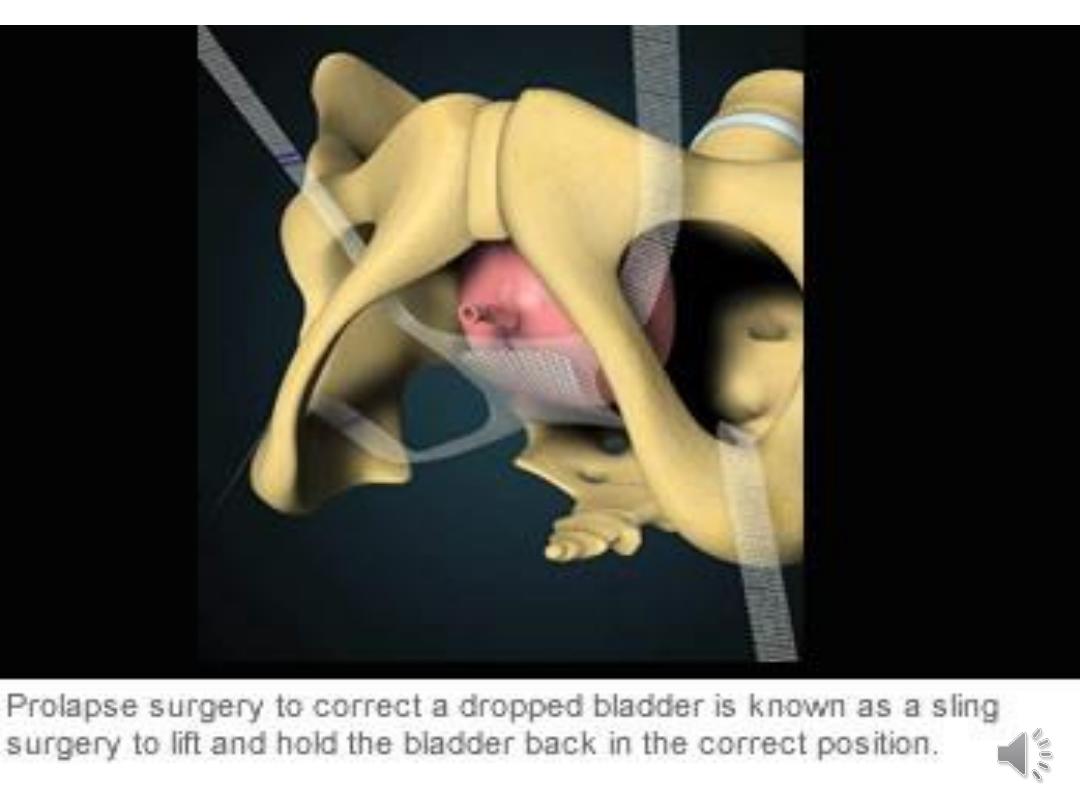
•Surgery for bladder/urethral prolapse
•Anterior colporrhaphy:
involves central plication of the fibro-
muscular layer of the anterior vaginal wall. Mesh
reinforcement may be used. Performed trans-
vaginally.
- Intra-operative complications are uncommon
but haemorrhage, haematoma, and cystotomy
may occur.

Colposuspension:
performed for urethral sphincter
incontinence associated with a cystourethrocele.
The paravaginal fascia on either side of
the bladder neck and the base of the bladder are
approximated to the pelvic side wall by sutures
placed through the ipsilateral iliopectineal
ligament.

•Surgery for uterine prolapse
•Hysterectomy:
a vaginal hysterectomy has the advantage
that no abdominal incision is needed, thereby
reducing pain and hospital stay. This can be
combined with anterior or posterior
colporrhaphy.

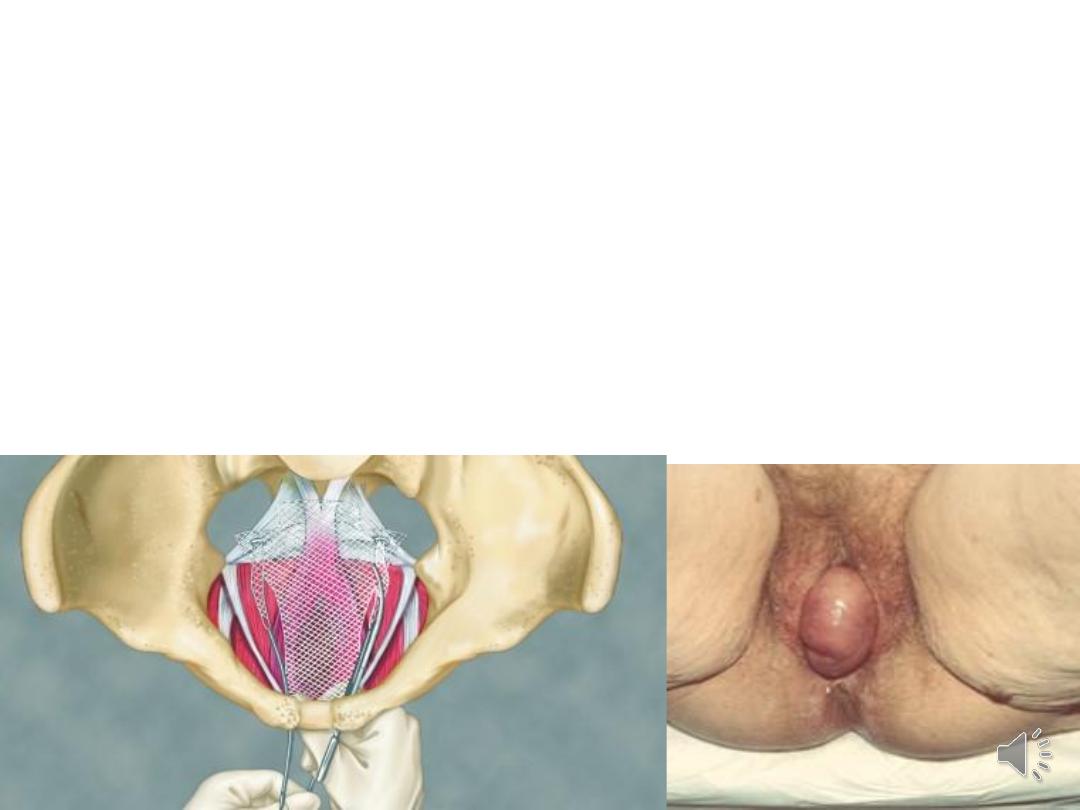
•Abdominal or laparoscopic sacrohysteropexy:
performed if the woman wishes to retain her
uterus. The uterus is attached to the anterior
longitudinal ligament over the sacrum. Mesh is
used to hold the uterus in place.

Sacrospinous fixation:
unilateral or bilateral fixation of the uterus to
the sacrospinous ligament. Performed via vaginal
route. Lower success rate than sacrohysteropexy.
Risk of injury to pudendal nerve and vessels and
sciatic nerve.
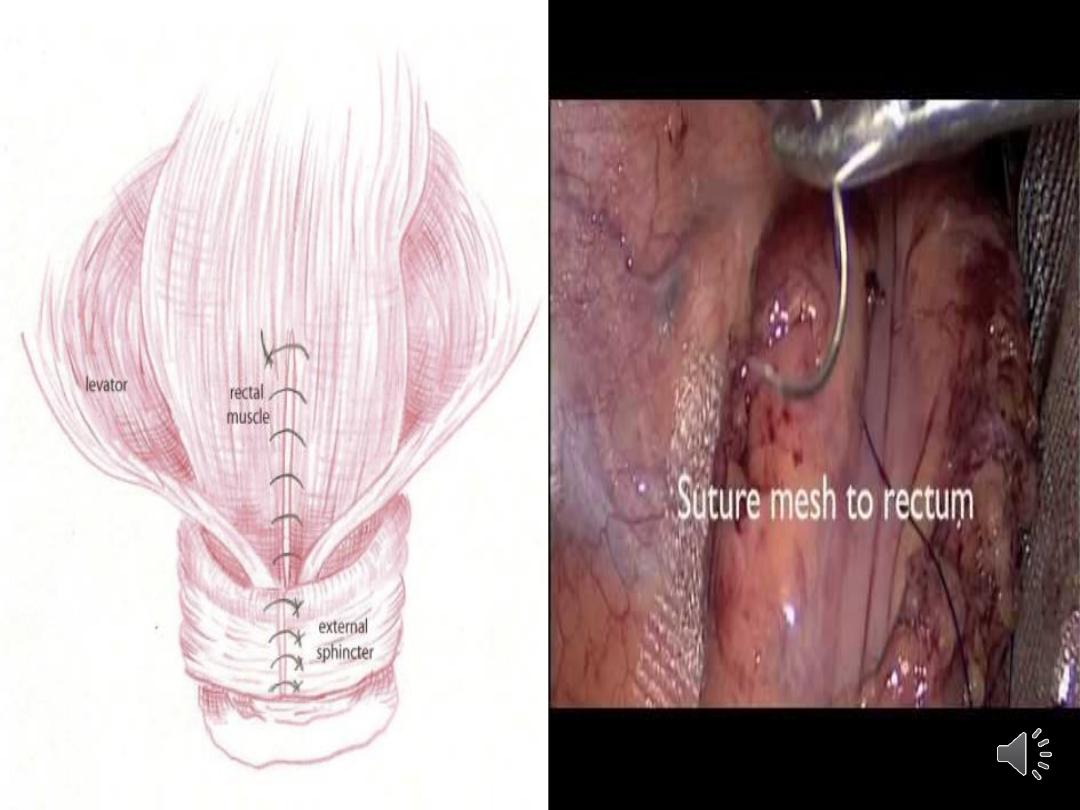
•Surgery for rectocele/enterocele
•Posterior colporrhaphy:
involves levator ani muscle plication or by
repair of discrete fascial defects. A mesh can be
used for additional support. Performed
transvaginally. Levator plication may lead to
dyspareunia.

•Obliterative surgery
•Corrects prolapse by moving the pelvic viscera back
into the pelvis and closing off the vaginal canal.
Known as colpocleisis.
•Vaginal intercourse is no longer possible.
•Advantages are that it is almost 100% effective in
treating prolapse and has a reduced perioperative
morbidity.
•Not commonly carried out in Europe.

Prevention:
•Possible preventative measures:
•Good intrapartum care:
including avoiding instrumental trauma and
prolonged labour.
•Pelvic floor exercises may prevent prolapse so
advised after childbirth.
•Smoking cessation.
•Weight loss if overweight or obese.
•Avoidance of heavy lifting occupations.
•Treatment of constipation throughout life.