
Urinary Incontinence in
Women
By
Prof. Dr. Bushra AL-Rubayae

Objectives:
• Physiological factors .
• Definition.
• Etiology & risk factors.
• Types.
• Presentation.
• Investigations.
• Treatment options.

Physiology of Micturtion:
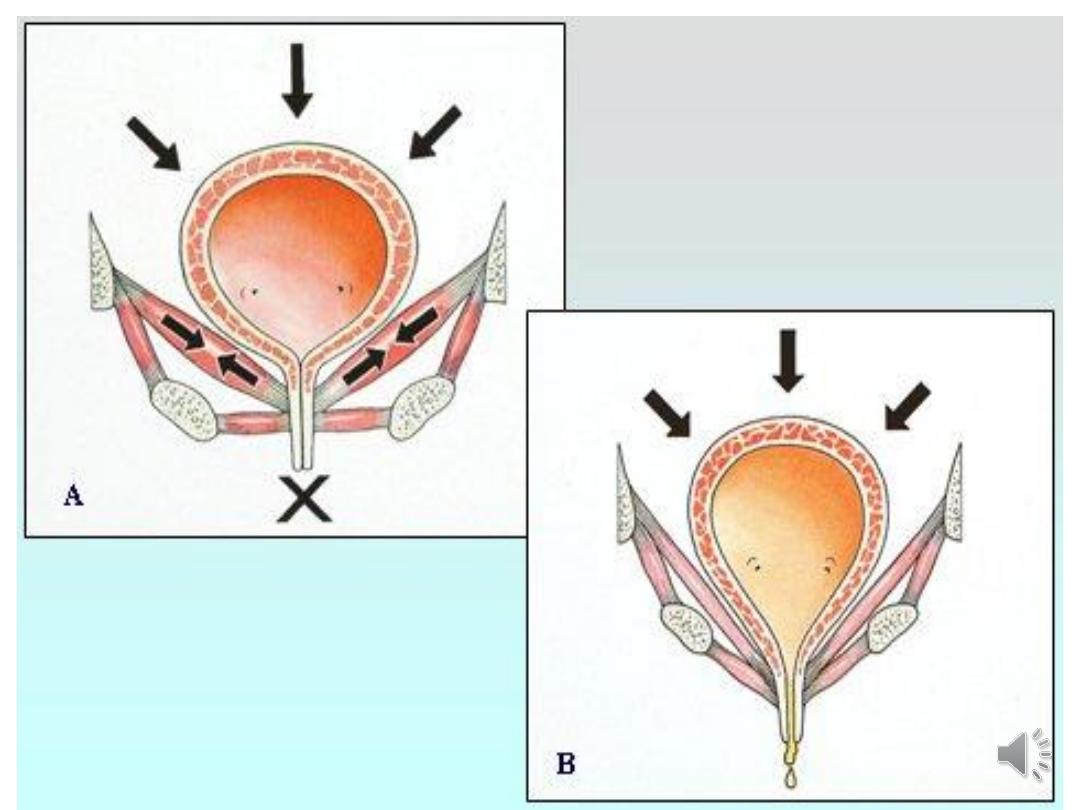
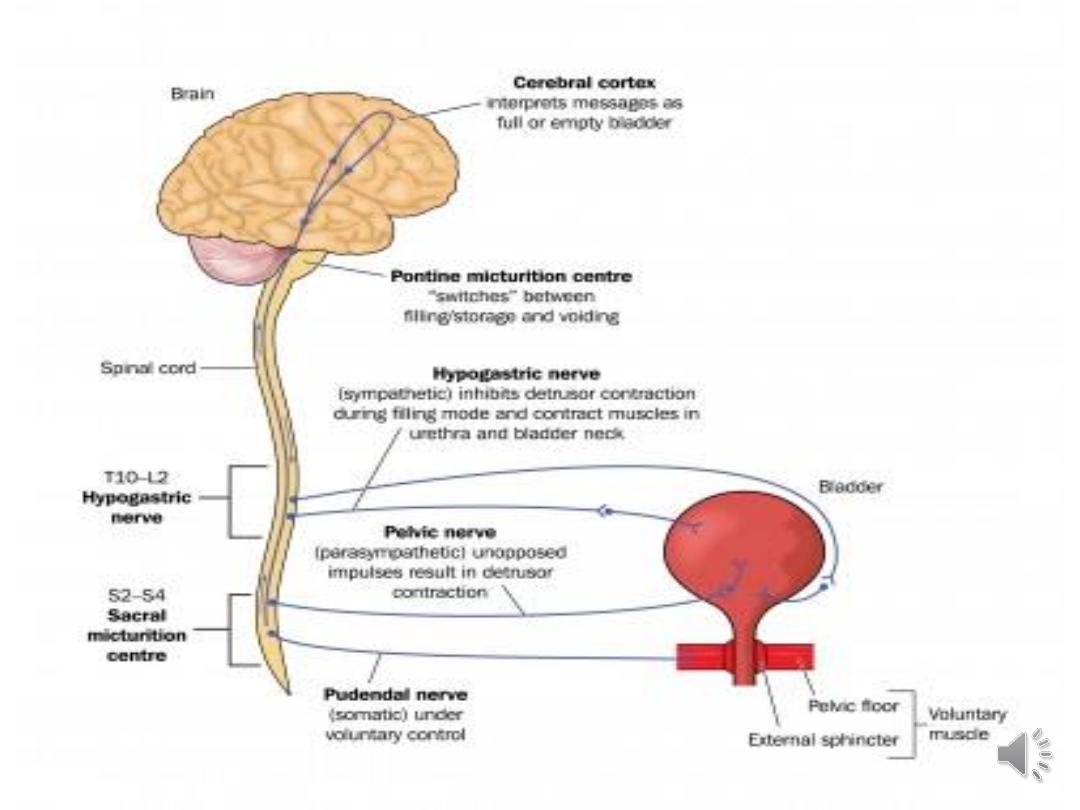
•Storage and voiding involves complex
interactions between the bladder, urethra,
urethral sphincter, and nervous system.
•The urinary bladder, capacity of 400 to 500
ml, serves to store or expel urine by
relaxation or contraction of the detrusor
muscle.

•The urinary sphincter, composed of an
internal component, a continuation of
detrusor smooth muscle that converges
to form a thickened bladder neck
controlled by the autonomic nervous
system.
• Somatically controlled external
component (striated muscle), must relax
to allow for the contracting bladder to
expel its load.

•Urinary incontinence (UI) :
any involuntary leakage of urine may occur as a
result of abnormalities of function of the lower
urinary tract or as a result of other illnesses.
•It’s common condition affect women of all ages,
with a wide range of severity.
• It influences the physical, psychological and social
wellbeing of affected individuals.
•In UK between 3 and 6 million may have urinary
incontinence.

Types of Urinary incontinence (UI) including:
•Stress UI
•Urgency UI
•Mixed UI
•Overactive bladder (OAB):
- OAB wet: occur with urge UI.
- OAB dry: occur without urge UI.

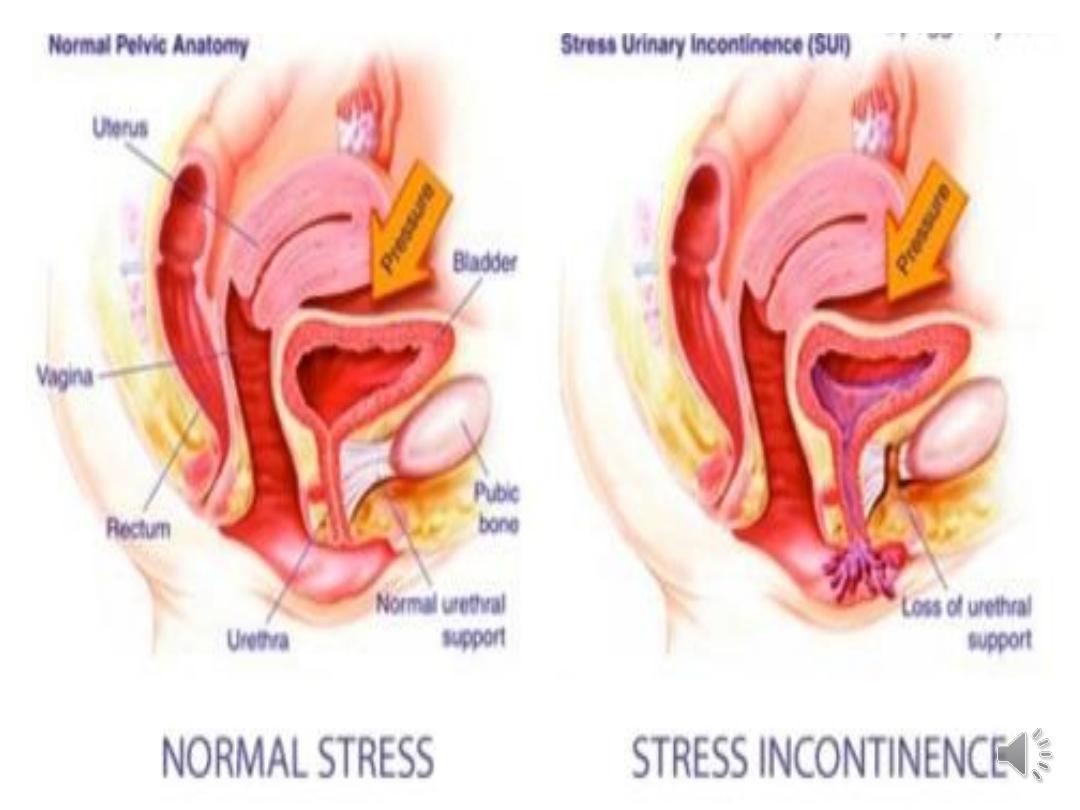
•Stress UI:
It’s involuntary urine leakage on effort or
exertion or on sneezing or coughing.
increase in intra abdominal pressure →
the bladder pressure exceeds urethral
pressure → Involuntary leakage of urine.

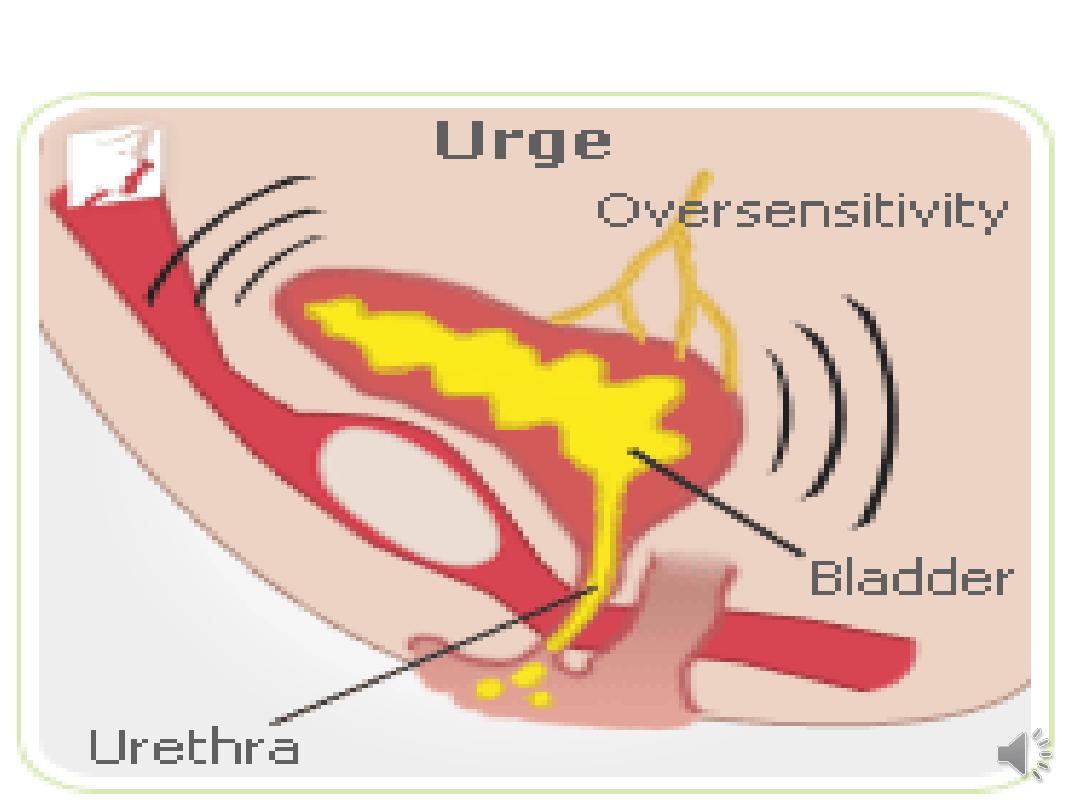
Urgency UI:
It’s involuntary urine leakage
accompanied or immediately preceded
by urgency (a sudden desire to urinate
that is difficult to delay).

•Mixed UI:
It is involuntary urine leakage associated
with both urgency and exertion, effort,
sneezing or coughing.

Overactive bladder (OAB)
• It’s defined as urgency that occurs with or without
urgency UI and usually with frequency and
nocturia.
• 'OAB wet:
OAB that occurs with urge UI .
OAB dry:
OAB that occurs without urge UI .

•Risk Factors:
•Post-Vaginal delivery:
•30% of women become incontinent after
first vaginal delivery
•Episiotomy is not protective
•Caesarean delivery may be partially
protective
Post menopause:
Post Operative:

•Other risk factors: Obesity, Functional
and Cognitive impairment, Family
history, Constipation, Smoking, Genito-
urinary prolapse

DIAGNOSIS:
History:
•Severity and quantity of urine lost and frequency
of incontinence episodes
•Duration of the complaint .
•Triggering factors or events ( cough, sneeze,
lifting, bending, feeling of urgency)
•Associated frequency, urgency, dysuria &UTI.

•Any associated faecal incontinence or pelvic
organ prolapse
•Obstetrical history: difficult deliveries, grand
multiparty, forceps , and large babies.
•History of hysterectomy , or pelvic floor
surgery.

•Lifestyle issues as smoking or caffeine abuse.
•Any medications.
Medical problems :Chronic cough
•Chronic obstructive pulmonary disease (COPD)
•Congestive heart failure
•Diabetes mellitus
•Connective tissue disorders
•Postmenopausal hypo-estrogenism.
•Urinary tract stones

•Physical Examination:
• Height, weight, Bp, PR. Obesity is a contributor
to SUI influence therapy.
•RS, CVS Exam.
•Abd. Exam.
• the flank and costo-vertebral angles tenderness,
or the presence of surgical scars.
•Pelvic exam. Type of UI.
• Assessment of pelvic floor muscles and prolapse.
•Neurologic examination.

•Investigations:
•Urine testing:
- MSU,C&S.
Symptoms of UTI with leucocytes &nitrate.
Symptoms of UTI with no leucocytes&nitrate.
No symptoms of UTI with leucocytes &nitrate

U/S for Assessment of residual urine:
• residual urine normally less than 50 mls.:
• Indications:
-symptoms of voiding problems.
-recurrent UTI.
- Palpable bladder after voiding.

• Bladder diaries:
assessed at least for 3 days.
• Pad test.
Not recommended in routine assessment.
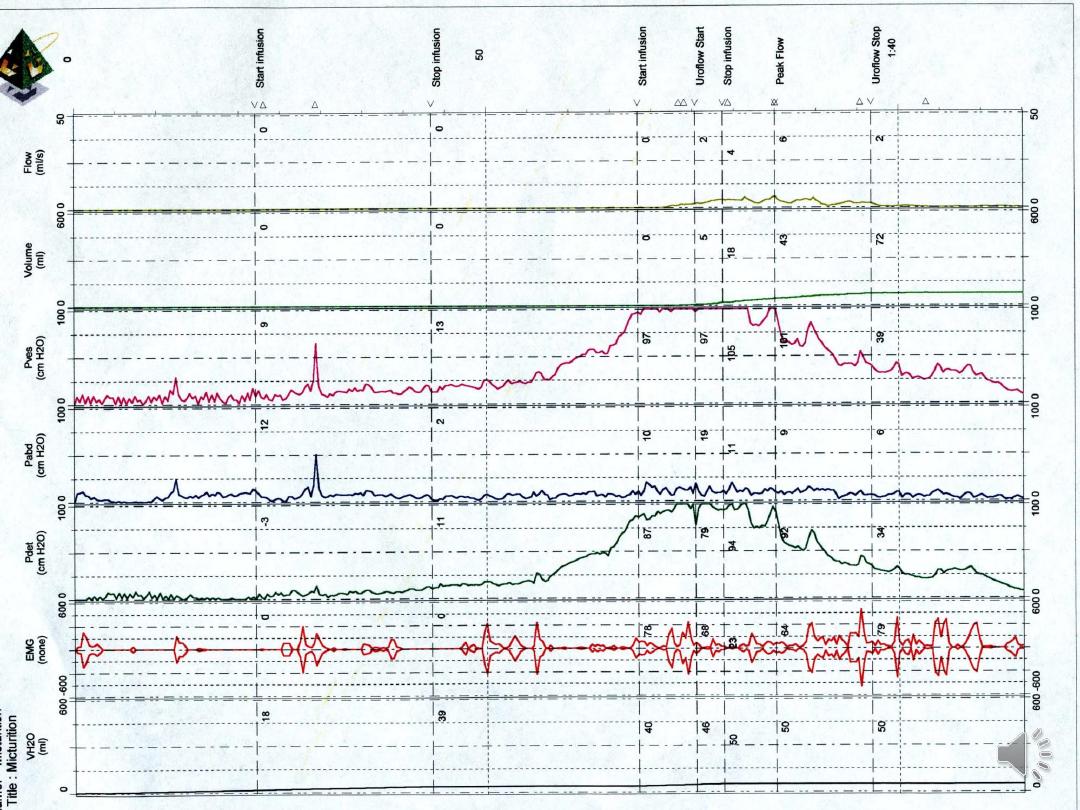
Urodynamic study:
Not recommended before start conservative treatment.
• Urodynamic testing, as indicated:
• Cystometry. Subtracted cystometry

Urodynamic
studies :
They are means of evaluating the pressure-
flow relationship between the bladder and the
urethra for defining the functional status of the
lower urinary tract.
• It aids in the diagnosis of urinary incontinence
based on patho-physiology.
•It assess both the filling-storage phase and the
voiding phase of bladder and urethral function

Conservative management:
• 1- Life style intervention:
• A trial of caffeine reduction.
• Modification of fluid intake.
• Weight loss if BMI more than 30.

Stress incontinence Therapy :
2- Physical therapy:
Pelvic floor physiotherapy.
• Pelvic Floor Muscle Training (PFMT):(more than 3 ms)
• It should be offered to all women as first-line management
and is effective for both stress and urge UI . If brief verbal
instruction on PFM contractions is adequate in 78% of
women .
• Vaginal cones ,electrical stimulation.
Anti-incontinence devices.
• Absorbent Products
are pads or garments designed to absorb urine to
protect the skin and clothing. By reducing wetness and odour,
they help to keep patients comfortable and allow them to
function in usual activities.

3- Drug therapy:
Imipramine (Tofranil):
It facilitates urine storage by decreasing bladder
contractility and increasing outlet resistance. It has an
alpha-adrenergic effect on the bladder neck, an
antispasmodic effect on the detrusor muscle, and a local
anesthetic effect on the bladder mucosa
• Duloxetine:
• It’s serotonin/nor-adrenaline reuptake inhibitor It is
approved for the treatment of stress incontinence in
Europe, enhance urethral activity. Dose 20-40 mg.

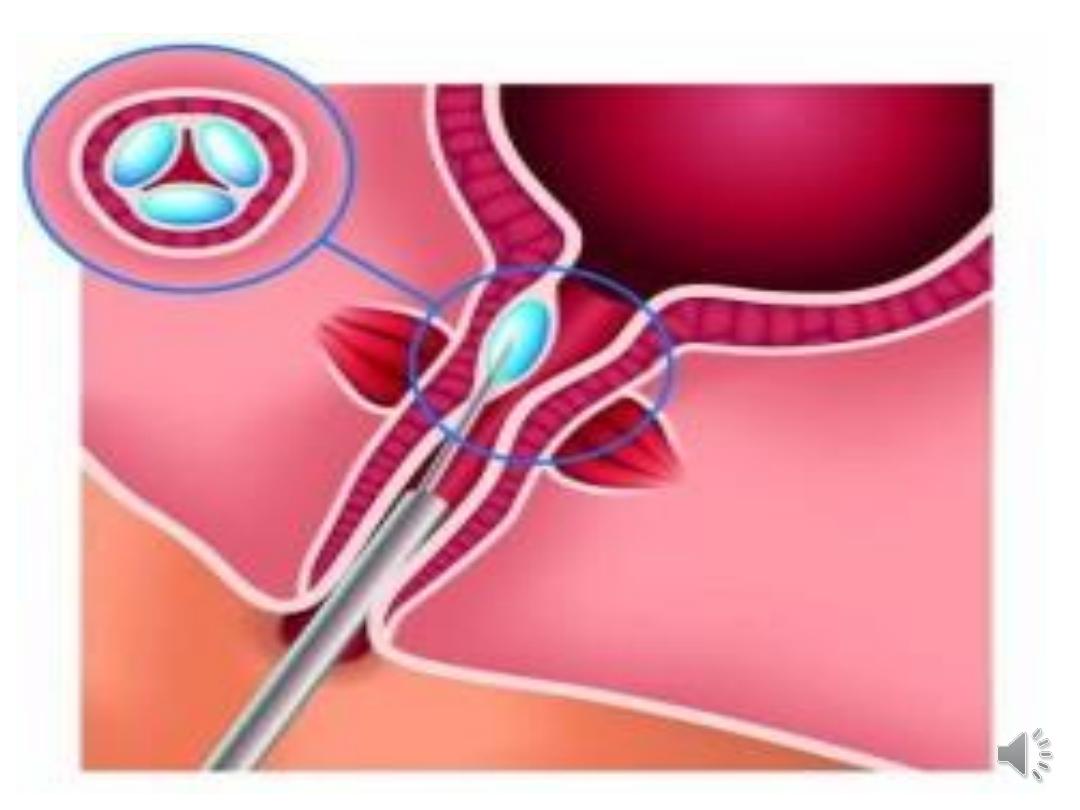
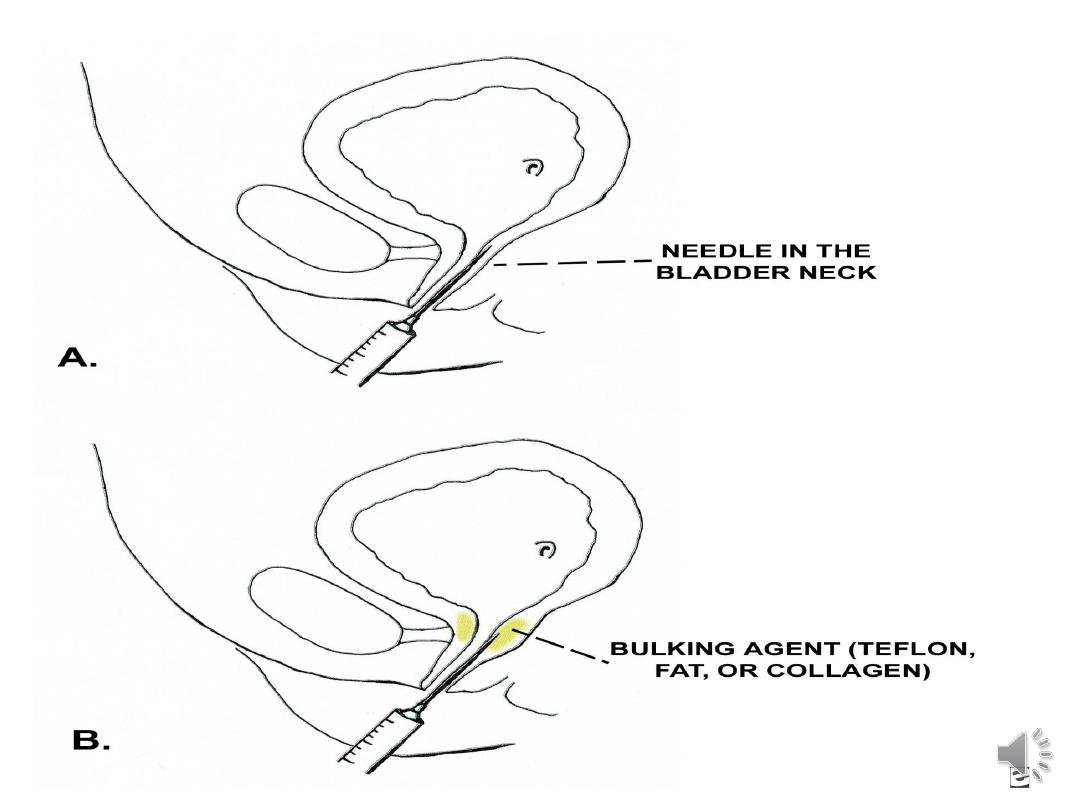
Urethral bulking agent:
It is a substance that can be injected into the
walls of the urethra. This increases the size of the
urethral walls and allows the urethra to stay
closed with more force like collagen, or
autologous substances .More recently,
investigations stem cell injections.
It can be transurethral and per-urethral injection.

Surgery for stress incontinence:
minimally invasive surgery may be the most
effective form of managing urinary incontinence
• Tape procedures
A piece of plastic tape is inserted through an
incision inside the vagina and threaded behind the
urethra. The middle part of the tape supports the
urethra, and the two ends are threaded through two
incisions in either the:
• tops of the inner thigh – this is called a transobturator
tape procedure (TOT)
• abdomen – this is called a retropubic tape procedure or
tension-free vaginal tape procedure (TVT)
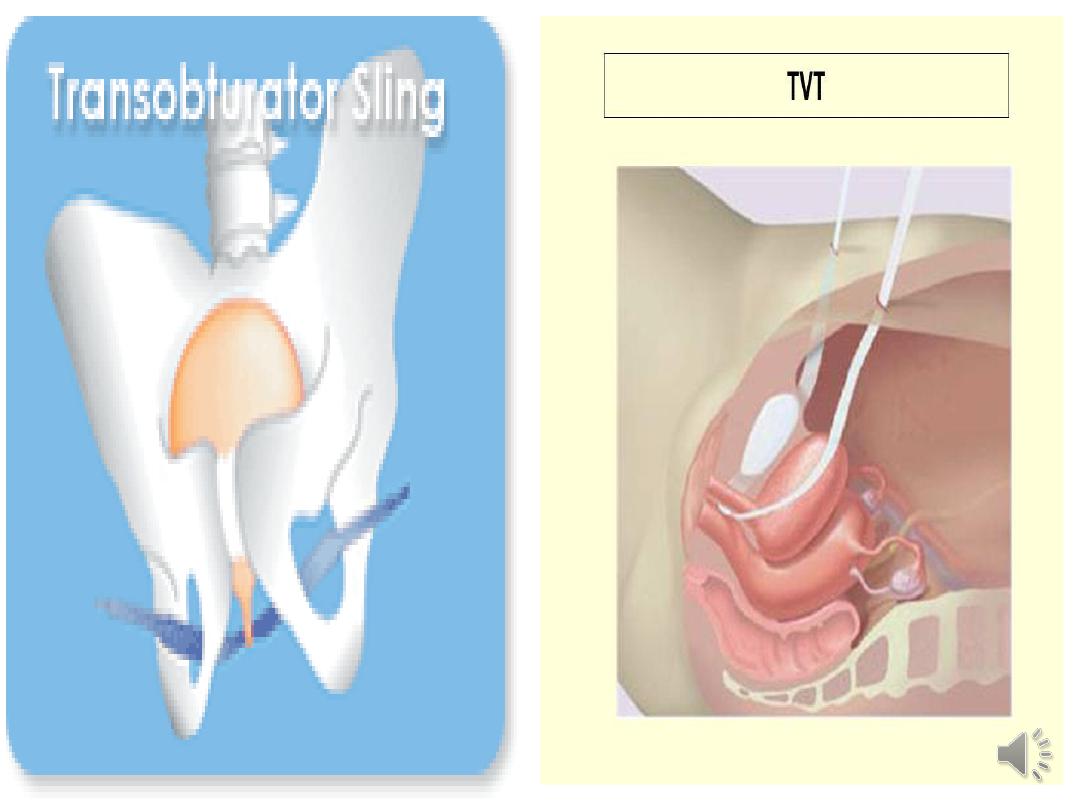
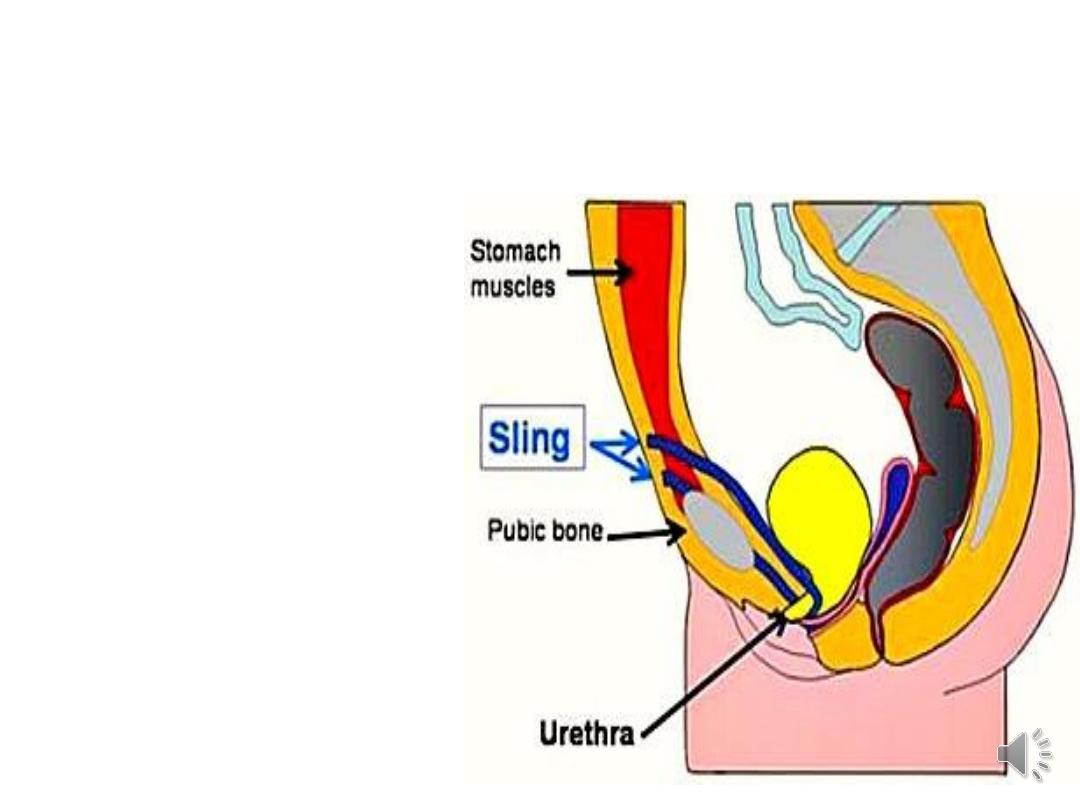
Surgery:
• Colpo-suspension:
• Sling procedures:
Abdominal.
Laparoscopic.
Abdominal-vaginal.
Vaginal.

Urge incontinence Treatment:
Changes in diet habits.
behavioural modification(Bladder Re-training).
pelvic-floor exercises.
medications :
Anti-cholinergic Drugs
• Oxybutynin :
It reduces incontinence episodes by 83-90%. The total continence rate
reported to be 41-50%.
• Tolterodine (Detrol):
It is a potent anti-muscarinic agent for treating detrusor over activity.
The dosage range is 1-2 mg twice daily.

New forms of surgical intervention:
•Botulinum toxin
•It s use in patients with neurologic
conditions who have overactive bladder.
Intra-detrusor injections via cystoscopy
•Mixed incontinence :
Anti-cholinergic drugs and surgery.

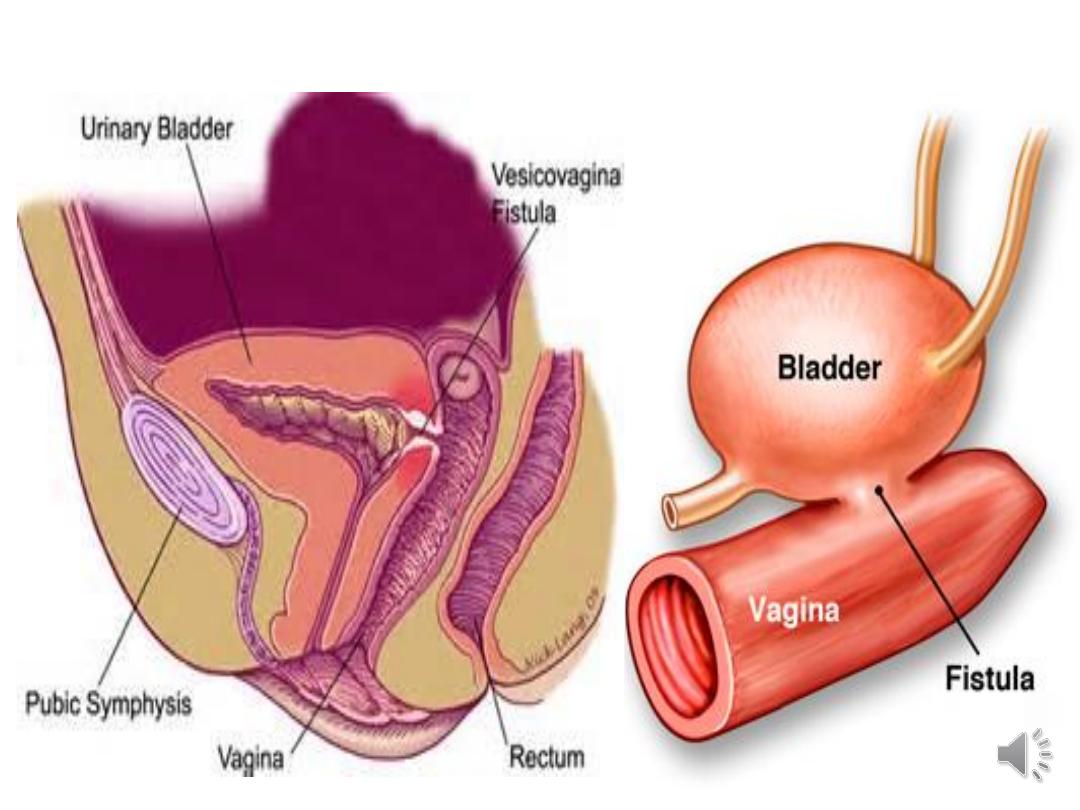
Urinary Fistula:( True Incontinence)
Vesico -vaginal F.
Uretero -vaginal fistulas
are the most feared complications of female pelvic
surgery. More than 50% of such fistulas occur after
hystrectomy for benign diseases as uterine fibroids,
menstrual abnormalities, and uterine prolapse.
The incidence of vesico-vaginal fistula is unknown.
The incidence of vesico-vaginal F. resulting from
hysterectomy is estimated to be less than 1%.

•In USA, more than 50% of vesicovaginal and
ureterovaginal F. occur after hysterectomy for
benign diseases.
•Pelvic radiation is the primary cause of delayed
fistula. Radiation is used to
treat
cervical
or endometrial carcinoma .
•In developing countries, obstetrical complications
are the most common cause .
• In cases of longstanding and obstructed labour
leading to pressure necrosis on the anterior
vaginal wall. It may be large and have extensive
local tissue damage and necrosis.

Diagnosis:
History.
Ph. examination : PV , any fluid collection noted.
Investigations:
Discharge can be tested for urea, creatinine, or
potassium concentration to determine VVF.
• Indigo carmine dye can be given intravenously and if the
dye appears in the vagina, a fistula is confirmed.
• Three swab test:
By filling of the bladder with methylene blue and use
cotton in three sites in the vagina and see which will
stain.
•Colour Doppler ultrasonography with contrast
media of the urinary bladder may be considered .
• Cysto-urethroscopy may be performed.
• If ureteric involvement is suspected then IVP
performed.
•The differential diagnosis for the discharge of
urine vesico-vaginal F. ,or Vaginitis.
•Urine should be sent for culture and sensitivity,
and infection should be treated.

Treatment:
•Vesico-vaginal and Uretero-vaginal fistulas
recognized within 3-7 days after the causative
operation may be repaired immediately via a
trans-abdominal or trans-vaginal approach.
•Fistulas identified after 7-10 days postoperatively
should be monitored periodically until all signs of
inflammation and indurations have resolved.

•The traditional approach has been to wait at
least 3-4 months before fistula closure.
•Some they close the fistula with or without using
peritoneal flap without waiting 3-4 months.
•Patients with a history of multiple failed repairs,
patients with associated enteric fistula or
patients with a history of pelvic radiation should
not undergo fistula repair for at least 6-8 months.

For a small fistula, an initial trial of urethral
catheter drainage may be attempted for 4-6
weeks. Optimal success achieved in patients who
had longer and narrower fistulas.
. Persistent incontinence after an adequate period
of watchful waiting requires open exploration
and formal fistula repair.

•The trans-vaginal approach is the safest and most
comfortable for the patient.
• A history of previous failed repairs does not
preclude trans-vaginal reconstruction.
•Fistulas occurring after hysterectomy are usually
amenable to trans-vaginal reconstruction.
•Trans-vaginal repairs do not require excision of
the fistula tract.
