Epidemiology of Diabetes Mellitus
Definition
Diabetes mellitus is a metabolic disorder of multiple etiology characterized by chronic hyperglycemia with disturbances of carbohydrates, fat and protein metabolism resulting from a defect in insulin secretion, insulin action or both.Why diabetes is important?
Diabetes is a common disease.There is evidence that the overall worldwide prevalence of diabetes is gradually increasing.
Diabetes causes great morbidity and early mortality in a large number of people, since it is associated with many complications.
The cost of managing the complications of DM is high.
Burden of DM
Diabetes prevalence is increasing in the developed world due to aging of the population, and in the developing world due to increased urbanization accompanied by cultural and socio-economic changes. Experts estimated that the number of adults with diabetes will reach 300 million in the year 2025, more than 75% of them (i.e. 228 million) will be in the developing countries.Global Prevalence Estimates, 2000 and 2030
4.4 %2.8 %
Reference: Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes. Diabetes Care. 2004; 27(5): 1047-1053.
1995
2025
19 million
57 million
DIABETES
Top Three Countries in the world
King et al, Diabetes Care, 1998
2.9 million
Number of deaths attributable to diabetes in the year 2000 (Roglic et al, 2005)(5.2% of total mortality)
HIV/AIDS deaths: 3 million
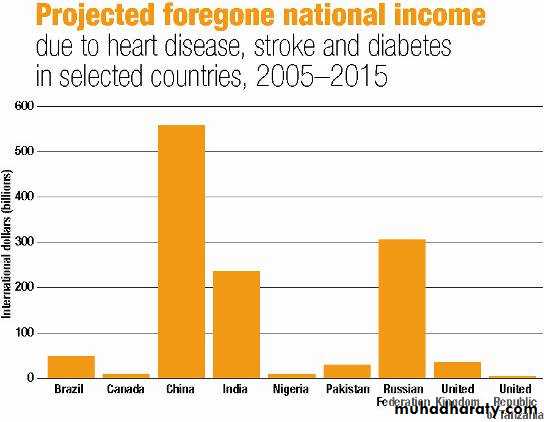
Economic Burden
It is estimated that the cost of caring for people with diabetes is 2-4 times the cost of caring for non-diabetic people in most health care systems. In 1992 a study in the US concluded that more than US $ 100 billion was spent on overall health care of people with diabetes.Funding for Noncommunicable Chronic Diseases at WHO
Global NCD disease burdenTotal WHO expenditure on NCDs
In 2002, 3.5% of total budget of
US$ 43.6 million on NCDs
Source: WHO long-term strategy for prevention and control of leading chronic diseases
© World Health Organization [2004]
The economic impact: billions
Types of DMType 1 DM
Accounts for 10% of all patients
Destruction of B-cells
Absolute insulin deficiency
Mostly at ages <30 years (it can occur at any age)
Types of DM
Forms of Type 1 :A- Autoimmune:
- Presence of autoimmune markers ( ICAs, IAAs, Autoantibodies to GAD65)
- Strong HLA association
- There is a genetic element
B-Idiopathic: (no known cause)
Only minority of patients fall in this group
Occurs in individuals of African& Asian origin
Strongly inherited
Lacks autoimmune markers
No HLA associated
Types of DM (Contin.)
Type 2
Most common (90%)
After age of 40 years
Predominant insulin resistance with relative insulin deficiency, ultimately loss of B-cells mass can lead to insulin dependency
Onset is insidious
Due to genetic factors, environmental factors or both.
Types of DM (Contin.)
Other specific types:Genetic defects of Beta-cells: onset at early age (<25 years). Inherited as an autosomal dominant pattern. Previously known as maturity onset diabetes of young (MODY).
Diabetes secondary to diseases of the pancreas or endocrinal diseases & drugs.
Gestational diabetes
Complications of DM
Type 1 DM(Insulin deficiency)
Micro vascular
(Small vessels)Nephropathy
Retinopathy
Neuropathy
Type 2 DM
(Insulin resistance)
Macrovascular
(Large vessels)
Atherosclerosis
*CHD
* Cerebrovascular disease
* Peripheral arterial disease
Cardiovascular disease (i.e. macrovascular complications) is the cause of death in 75-80% of patients with type 2 DM)
Impact of Diabetes Mellitus
DiabetesThe leading cause of new cases of end stage renal disease
A 2- to 4-fold increase in cardio-vascular mortalityThe leading cause of new cases of blindness in working-aged adults
The leading cause of non-traumatic lower extremity amputations
Diagnosis of DM
Fasting plasma glucose >126mg/dl (7mmol/l)2 hours postprandial plasma glucose >200mg/dl
Any random plasma glucose >200mg/dl (11.1 mmol/l), together with polyuria, polydypsia, weight loss, and visual blurring
Must confirm diagnosis with two abnormal plasma glucose results on separate days
Diagnosis of DM
Glycosylated hemoglobin (HbA1c)- reflection of how well the glucose has been controlled.
- hyperglycemia causes an increase in HbA1c
- values expressed in percentages,
* with non-diabetic 5.5 to 7%,
* diabetic with good control 7.5 to 11.4%
* diabetic with moderate control 11.5 to 15%
*diabetic with poor control greater than 15%
Diagnosis of Impaired Glucose Tolerance
Impaired glucose tolerance was defined by the Expert Committee as:
Fasting Plasma glucose of 110-125mg/dl
2-hour post glucose load 140-199mg/dlRisk factors
Genetic factors- Twin studies indicate a very strong genetic component to the etiology of type 1 DM. It is more common in those with certain HLA types.
- Twin studies also demonstrate a greater than 30% concordance among monozygotic twins pairs in the expression of type 2 DM.
- Certain racial groups , as African Americans, Hispanics, and Native Americans, are at increased risk for type 2 diabetes.
Risk factors (contin.)
Age: Incidence of type 2 DM increases with increasing age.Physical inactivity: Lack of exercise may alter the interaction between insulin and its receptors and subsequently leads type 2 DM.
Vigorous exercise > 1/week, 25% risk reduction (Manson & al, Lancet 1991, 338; 774-8., JAMA, 1992, 268,63-7)
Looking TV 2-10 hours per week: RR 1.66 of having DM compared with 0-1 hour per week
( HU et al; Arch Intern Med 2001;161: 1542-1548)Obesity: Incidence of type 2 DM increases with increasing body mass index. Obesity can induce resistance to the action of insulin.
RR risk of DM in females (ref. BMI < 22)
22-23 3.0
24-25 5.0
> 31 40
(Colditz & al, Ann Int Med, 1995, 122; 481-6)
Risk factors (contin.)
Drugs & hormones: Long list of drugs that affect carbohydrate metabolism had been identified. e.g. Phenytoin, diuretics (thiazide type), corticosteroids. Oral contraceptives, and beta-adrenergic blocking agents.Pancreatic disorders: Inflammatory, neoplastic, and other disorders of the pancreas e.g. cystic fibrosis, and pancreatectomy.
History of gestational diabetes or delivery of large babies.
Diabetes MellitusTreatment
NO CURE!Relieve symptoms.
Maintain quality of life.Prevent further complications.
Preventive measures
Primary prevention: Primary prevention of type 2 DM can be achieved by:
- Promotion of healthy nutrition: Encourage low saturated fat, high fiber diet.
- Smoking cessation
- Correction of obesity: Encourage weight loss to keep BMI<30
There are two approaches for primary prevention:
Primary prevention (contin.)
The high risk approach:This is directed to high risk people such as those with family history of type 2 DM, obese individuals, and those with previous abnormalities of glucose tolerance including gestational diabetes.
Primary prevention (contin.)
The population approach:This is based on altering the environmental risk factors and determinants of type 2 DM in the whole population through public education
Secondary prevention
This level of prevention aims at early detection of asymptomatic casesEarly detection and treatment
Screening for gestational diabetes
Screening for susceptible groups
Screening for diabetes:
Screening all adults over 40 years of age with fasting plasma glucose every 2-3 years.
Begin screening at earlier age with a positive family history, obesity, or symptoms of DM.
The community should be involved in diabetes awareness and screening
Tertiary prevention
This involves treatment of already established cases of diabetes
What are the objectives of treatment of diabetes?
To relieve symptoms
To reduce mortality and economic costs of diabetes
To prevent as much as possible acute and long term complications and to monitor the development of such complications and to provide timely intervention
To improve the quality of life and productivity of the individual with diabetes
Goals of diabetes management
• Acceptable• Ideal (normal)
• intervention
• <140 mg/dl
• <125 mg/dl
• FPG
• < 7
• < 6
• HbA1C
• < 140/90
• < 130/80
• Blood pressure
• < 240 mg/dl
• < 200mg/dl
• S. Cholesterol
• < 130 mg/dl
• < 100 mg/dl
• LDL cholesterol
• No smoking
• No smoking
• Stop smoking
• BMI <30
• BMI <25
• Decrease weight
• Daily 30 min.
• Daily 30-60 min.
• Daily exercise
Goals for chronic diabetes may be somewhat different for good control, not ideal goals which are normal for a non-diabetic
Patient and family counseling
Patients and their families should be aware of the following:
The disease is permanent, life-long treatment is required
Control of blood sugar to delay appearance of microvascular complications
Importance of foot care
Wash & dry feet daily
Soften & gently reduce calluses
File (but not cut) nails
Wear shoes that are soft and well fitting
Never walk barefoot
Notice & deal with small injuries or signs of pressure
Patient and family counseling (contin.)
Management of hypoglycemic attacksInjection technique (when insulin used) and rotation of sites
Counseling in family planning if possible
Lifestyle modification:
smoking cessation
Diet control
Weight loss
Increase Physical activity
Social and psychological factors