1
Bullous diseases
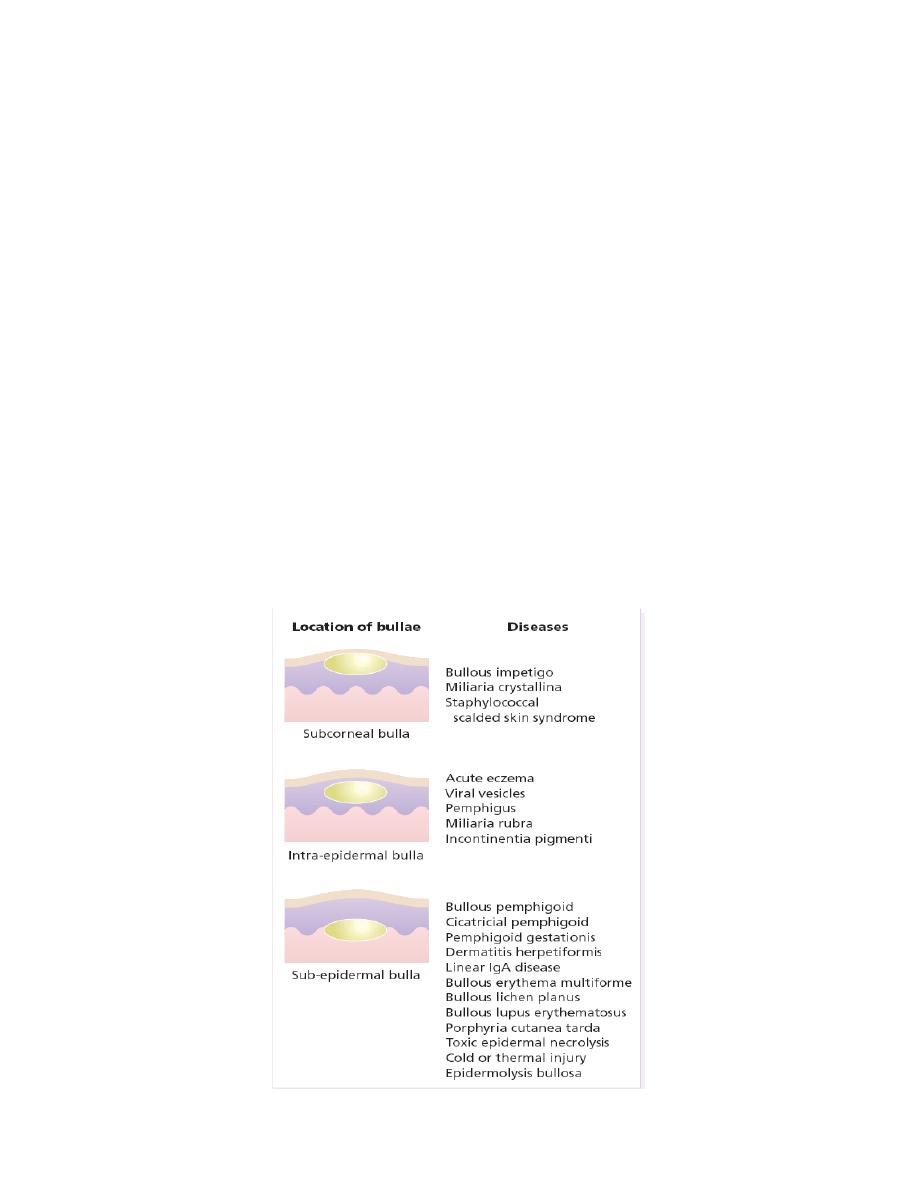
Blisters are accumulations of fluid within or under the epidermis. They have many causes,
and a correct clinical diagnosis must be based on a close study of the physical signs. The
appearance of a blister is determined by the level at which it forms. Subepidermal blisters occur
between the dermis and the epidermis. Their roofs are relatively thick and so they tend to be tense
and intact. They may contain blood. Intraepidermal blisters appear within the prickle cell layer of
the epidermis, and so have thin roofs and rupture easily to leave an oozing denuded surface: this
tendency is even more marked with subcorneal blisters, which form just beneath the stratum
corneum.
Sometimes the morphology or distribution of a bullous eruption gives the diagnosis away,
as in herpes simplex or zoster. Sometimes the history helps too, as in cold or thermal injury, or in
an acute contact dermatitis. When the cause is not obvious, a biopsy should be taken to show the
level in the skin at which the blister has arisen.
2
The dermo-epidermal junction
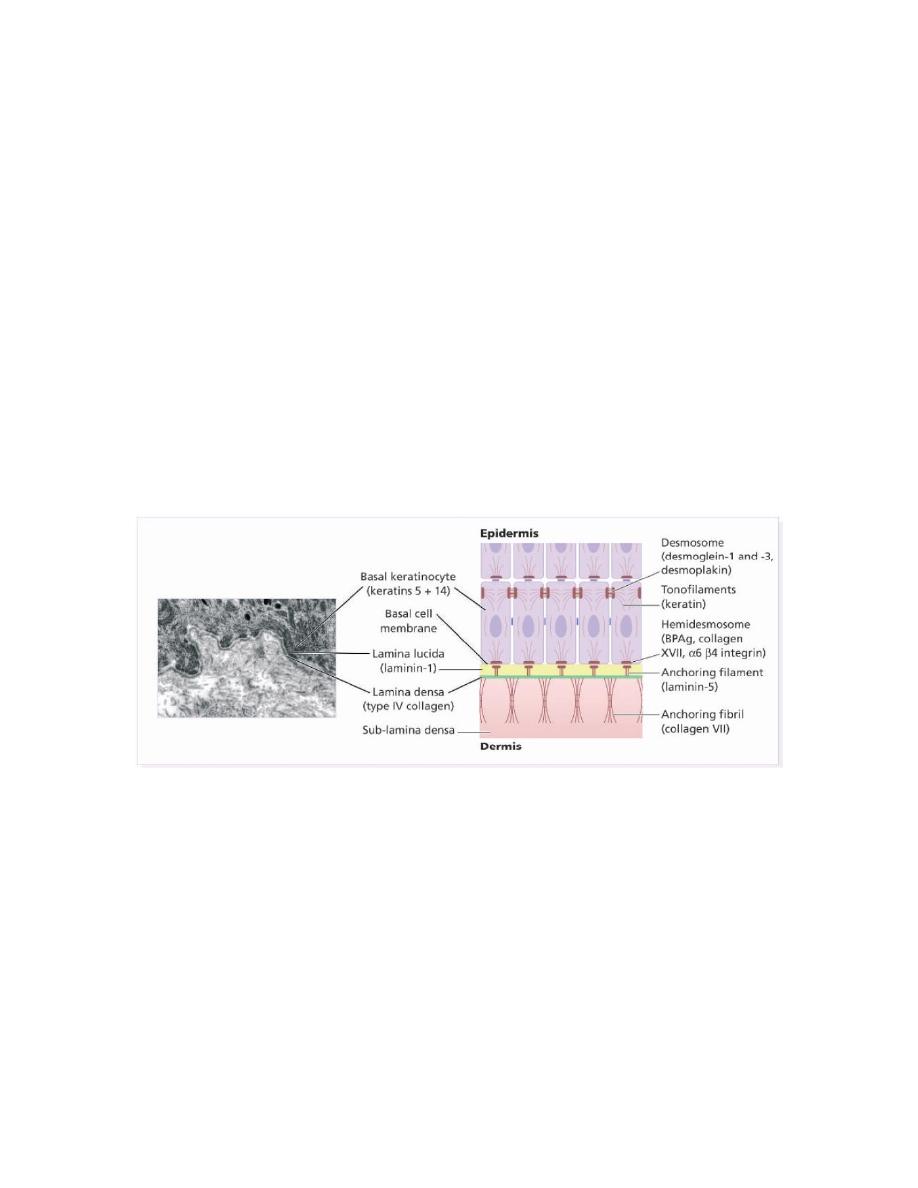
The basement membrane lies at the interface between the epidermis and dermis.
Electron microscopy shows that the lamina densa (rich in type IV collagen) is separated from the
basal cells by an electron-lucent area, the lamina lucida. The plasma membrane of basal cells has
hemidesmosomes (containing bullous pemphigoid antigens, collagen XVII and α6 β4 integrin).
The lamina lucida contains the adhesive macromolecules, laminin-1,. Fine anchoring filaments
(of laminin-5) cross the lamina lucida and connect the lamina densa to the plasma membrane of
the basal cells. Anchoring fibrils (of type VII collagen), extend from the papillary dermis to the
deep part of the lamina densa.
Pemphigus Group
Pemphigus refers to a group of disorders with loss of intraepidermal adhesion because
of autoantibodies directed against proteins of the desmosomal complex that hold keratinocytes
together. The desmosome is a complex structure, with many of its components targets for
autoantibodies.
Pemphigus vulgaris
Definition: Severe, potentially fatal disease with intraepidermal blister formation on skin and
mucosa caused by autoantibodies against desmogleins (one of demosomal proteins) .

3
Pathogenesis:
-Genetic predisposition: HLA-DR4.
- Patients develop antibodies against desmoglein 3 (Dsg3) and later desmoglein 1 (Dsg1) . The
bound antibodies activate proteases that damage the desmosome, leading to acantholysis.
-Occasionally drugs cause pemphigus vulgaris . Agents containing sulfhydryl groups
(penicillamine, captopril, piroxicam) ,penicillin, and rifampicin.
-Associated with other autoimmune diseases as thymoma and myasthenia gravis
Clinical features:
Skin
The skin lesions in PV are rarely pruritic, but are often painful. The primary lesion of PV
is a flaccid blister, which may occur anywhere on the skin surface . Usually, the blister arises on
normal-appearing skin, but it may develop on erythematous skin. Because these blisters are
fragile, intact blisters may be sparse. The most common skin lesions that occur in these patients
are erosions, often painful, subsequent to broken blisters. These erosions are often quite large, as
they have a tendency to spread at their periphery . This characteristic finding can be elicited in
pemphigus patients with active blistering by applying lateral pressure to normal-appearing skin at
the periphery of active lesions. The result is a shearing away of the epidermis in normal-appearing
areas, a phenomenon known as the
Nikolsky sign.
This sign helps differentiate pemphigus from
other blistering diseases of the skin . Sites of predilection include scalp, face, mechanically
stressed areas, nail fold, intertriginous areas (can present as intertrigo).
Mucous membranes
In the majority of patients, painful mucous membrane erosions are the presenting sign of
PV( 60% of the patients as presenting symptoms and 100% during the course of the disease) and
may be the only sign for an average of 5 months before skin lesions develop .
The mucous membranes most often affected are those of the oral cavity. Intact blisters are rare,
probably because they are fragile and break easily. Scattered and often extensive erosions may
appear on any part of the oral cavity, although they perhaps occur most frequently on the buccal
mucosa. These erosions may spread to involve the pharynx and larynx with subsequent

4
hoarseness. Often, these erosions are so uncomfortable and, in fact, painful that the patient is
unable to eat or drink adequately.
Diagnostic approach:
- Clinical evaluation; check sites of predilection.
- Nikolsky sign:
- True Nikolsky sign: Gentle rubbing allows one to separate upper layer of epidermis from lower,
producing blister or erosion.
- Pseudo-Nikolsky sign (Asboe–Hansen sign): Pressure at edge of blister makes it spread.
- Histology: When a fresh lesion is biopsied (small excision, not punch biopsy), There is
suprabasilar acantholysis is seen (free-floating, rounded keratinocytes) with retention of basal
layer keratinocytes (tombstone appearance)
-Direct immunofluorescence: Perilesional skin shows deposition of IgG (100%),
C3 (80%) , in early lesions. Antibodies surround the individual keratinocytes.
- Indirect immunofluorescence: Using monkey esophagus, 90% of sera show positive reaction;
titer can be used to monitor disease course.
Note Serum antibody titer usually correlates with severity of disease.
Therapy:
Systemic corticosteroids are necessary for long periods of time. The main cause of
morbidity and mortality today in patients with pemphigus vulgaris is corticosteroid side-effects.
For this reason, corticosteroids are always combined with steroid-sparing agents.
Patients should be screened for osteoporosis and latent tuberculosis before embarking on long-
term corticosteroid therapy. Osteoporosis prophylaxis may be warranted.
Steroid included prednisolone (1mg/kg) per day .steroid-sparing agents included
cyclophosphamide 1–2 mg/kg daily, azathioprine 2.5mg/kg, Alternative immunosuppressive
agents: Chlorambucil 0.1–0.2 mg/kg daily; cyclosporine 2.5-5mg/kg daily; mycophenolate
mofetil 2.0g daily, dapsone .
Pemphigus vegetans.
Definition: Unusual variant of PV with hyperkeratotic verruciform reaction (vegetans).
Clinical features: Two forms:

5
- Pemphigus vegetans Neumann type: Originally typical PV, then development of Fungoid or
papillomatoid lesions.
-Pemphigus vegetans Hallopeau type: Also known as pyodermite végétante, limited to
intertriginous areas, starts as pustules that evolve into vegetating lesions.
Histology is the same of PV with papillary hyperplasia and interaepidermal abscesses of
eosinophils formation.
Diagnostic approach: As for PV.
Therapy: as PV.
Pemphigus foliaceus
Definition: Form of pemphigus with superficial blisters caused by autoantibodies against Dsg1.
Pathogenesis:
-Autoantibodies against Dsg1, the main desmoglein in the upper epidermis; rarely antibody shift
so that they later are formed against Dsg3 and patient develops PV.
-More often drug-induced than PV. Usual agents have sulfhydryl groups such as captopril,
penicillamine, and piroxicam.
-May be caused by sunburn or as paraneoplastic sign.
Clinical features:
Sites of predilection include scalp, face, chest, and back (seborrheic areas) with diffuse
scale and erosions . Can progress to involve large areas (exfoliative erythroderma). Facial rash
sometimes butterfly pattern. Oral mucosa usually spared (Dsg1 is scarcely ( )بالكادexpressed in
oral epithelia). Individual lesions are slowly developing slack blisters that rupture easily, forming
erosions and red-brown crusts.
Histology: Blister forms in stratum corneum or stratum granulosum.
Diagnostic approach:
-Clinical appearance.
- Skin biopsy often not helpful.
- Direct in all cases and indirect immunofluorescence in 85% show superficial deposition of IgG.
Therapy: Same approach as PV but usually more responsive to therapy. Dapsone may be helpful.

6
Pemphigoid Group
Bullous pemphigoid.
Definition: Subepidermal blistering disease caused by autoantibodies to components of the
hemidesmosomes in the basement membrane zone (BMZ). Favors elderly, and incidence clearly
much higher in older age groups.
Pathogenesis:
Autoantibodies are directed against two hemidesmosomal proteins:
- BP 230 or BP antigen 1 (BPAG1), a 230kD component of the inner plaque of the
hemidesmosome.
- BP 180 or BP antigen 2 (BPAG2), a 180kD transmembrane glycoprotein also known as type
XVII collagen., BP 180 or BP antigen 2 (BPAG2) is a pathognomonic.
-Less common causes include drugs (benzodiazepine, furosemide, penicillin, sulfasalazine),
sunlight, and ionizing radiation.
Clinical features:
Before blisters develop, pruritus, dermatitic, and urticarial lesions may be present. Since
the entire epidermis is the blister roof, the blisters are very stable. They are tense, often have a
fluid level, and can reach 10cm in diameter . Oral mucosal involvement in 20%; rarely presenting
sign.
Histology:
Subepidermal blister formation
Cellular infiltration of both eosinophils, and neutrophils.
Absence of acantholysis.
Diagnostic approach:
-Clinically.
- Histology.
- Laboratory: Elevated ESR, eosinophilia in 50%.
-Direct immunofluorescence: band of IgG in 80% and C3 in 100% along BMZ.
-Indirect immunofluorescence: (70%) Using NaCl split skin, the autoantibodies usually attach to
just the roof of the blister.

7
Treatment
As PV but better response than PV, and needed less dose and course of treatment.
Cicatricial pemphigoid
More common in female 2:1.
Pathogenesis: Poorly understood; several different target antigens, BP 180, BP 230, laminin5,
integrin.
Clinical features:
Conjunctiva: Affected in 75% of cases; when sole site called ocular pemphigoid. Starts
unilaterally, within 2 years usually bilateral. Adhesions, ectropion, corneal damage . (25% of
patients lose their vision)
Oral mucosa: Also affected in 90% of cases; vesicles, blisters, erosions, scarring. Desquamative
gingivitis occurs. Much less painful than PV.
Esophagus and larynx can also develop strictures, requiring surgery.
Genitalia: In women, narrowing of vaginal orifice; in men, adhesions between glans and foreskin.
Skin: Only involved in 25% of cases; usually generalized disease similar to BP.
Localized form is known as Brunsting–Perry disease with persistent plaques on which recurrent
blisters develop which more common in male 2:1 , more than 60 years, no oral lesion & lesion
more in the head & neck.
Histology: same for bullous pemphigoid but there is fibrosis and scaring in the upper dermis.
Direct immunofluorescence: IgG & C3 (80-95%) along BMZ in lesional skin.
Indirect immunofluorescence: When NaCl split skin is used, IgG reactivity can be seen on
either side of the split, or in both locations, depending on target antigen.
Therapy:
- Ocular disease: topical or systemic corticosteroids; consultation with ophthalmologist.
-Mucosal disease: try topical corticosteroids first.
- Widespread or resistance disease:
Prednisolone 1–2mg/kg plus azathioprine 2mg/kg or prednisolone-cyclophosphamide,
antimalarial drugs.

8
High-dose intravenous immunoglobulins .
Persistent localized lesions: excision and grafting .
Subepidermal IgA-mediated Disorders
Dermatitis herpetiformis
Definition: Pruritic vesicular disease caused by IgA autoantibodies directed against epidermal
transglutaminase and presenting with a linear granular pattern at the dermo-epidermal junction. It
is associated with the presence of gluten enteropathy, although few patients actually have
gastrointestinal symptoms less 4%.
DH usually affects older children or young adults. Lesions typically occur on extensor
elbows and knees, over scapulae and sacrum, and in the scalp. They are small and intensely itchy
vesicles of a few millimeters in diameter, usually excoriated, and sometimes with a mildly
eczematous or urticated background . Oral and palmar lesions are both uncommon, but both may
be purpuric if they occur.
Histology: Neutrophilic microabscesses in the papillary dermis are the hallmark. Often
admixed with eosinophils. Edema leads to subepidermal blister formation.
Diagnostic approach:Direct immunofluorescence: Granular deposits of IgA in dermal papillae;
sometimes granular-linear along BMZ. Present in 95% of patients.
Indirect immunofluorescence: IgA antibodies against smooth muscle endomysium (source
of tissue transglutaminase) present in 80%.
Therapy:
The mainstay of therapy is a gluten-free diet ,which also protects against gastrointestinal
lymphoma. The diet is hard to follow and only takes effect after months, but is essential.
Forbidden food Wheat, rye, barley, oats.
Allowed food Potatoes, rice, corn, millet()دخن, buckwheat(ءادوس ةطنح).
Dapsone 50-200 mg/day. Other
sulfapyridine ,
salazopyrine consider sulfapyridine for patients
who can not tolerate dapsone.

9
Linear IgA Disease of adulthood :
Definition: Subepidermal blistering disease caused by deposits of IgA along BMZ.
Clinical features: LAD may be identical to dermatitis herpetiformis but without gastrointestinal
involvement, or resemble BP or even cicatricial pemphigoid with ocular involvement. Over 50%
have mucosal involvement.
Diagnostic approach: Both direct and indirect immunofluorescence tests showed liner IgA
antibobies along BMZ.
Histology: Subepidermal blister; usually with inflammatory infiltrate.
Therapy: Corticosteroids work best for lamina lucida type; dapsone often helpful for lamina
densa type.
Linear IgA Disease of childhood:
Most common subepidermal blistering disorder in childhood.checterized by Subepidermal
blistering disease caused by deposits of IgA along BMZ. Usually occurs before 5years of age and
resolves spontaneously 10-15 years.
Clinical features: Large tense blisters, almost always arranged in rosette fashion, with
predilection for abdomen, groin, axillae, and face . Also urticarial plaques with peripheral blisters.
Mucosal disease very common; as high as 75-90% in some series. Gastrointestinal disease
extremely rare.
Histology: Subepidermal blister; usually with inflammatory infiltrate.
Diagnostic approach: presence of IgA deposits along BMZ identified by direct
immunofluorescence in 100% and indirect immunofluorescence in 40–70%.
Therapy: Both dapsone and sulfapyridine may be useful. If not, systemic corticosteroids.
