
Acute renal injury (AKI)
Dr. Ali Althabhawi
Acute kidney injury (AKI)
AKI has been traditionally defined as an abrupt loss
of kidney function leading to a rapid decline in the
glomerular filtration rate (GFR), accumulation of
waste products such as blood urea nitrogen (BUN)
and creatinine, and dysregulation of extracellular
volume and electrolyte homeostasis.
The incidence of AKI varies from 2–5% of all
hospitalizations to > 25% in critically ill infants and
children
.
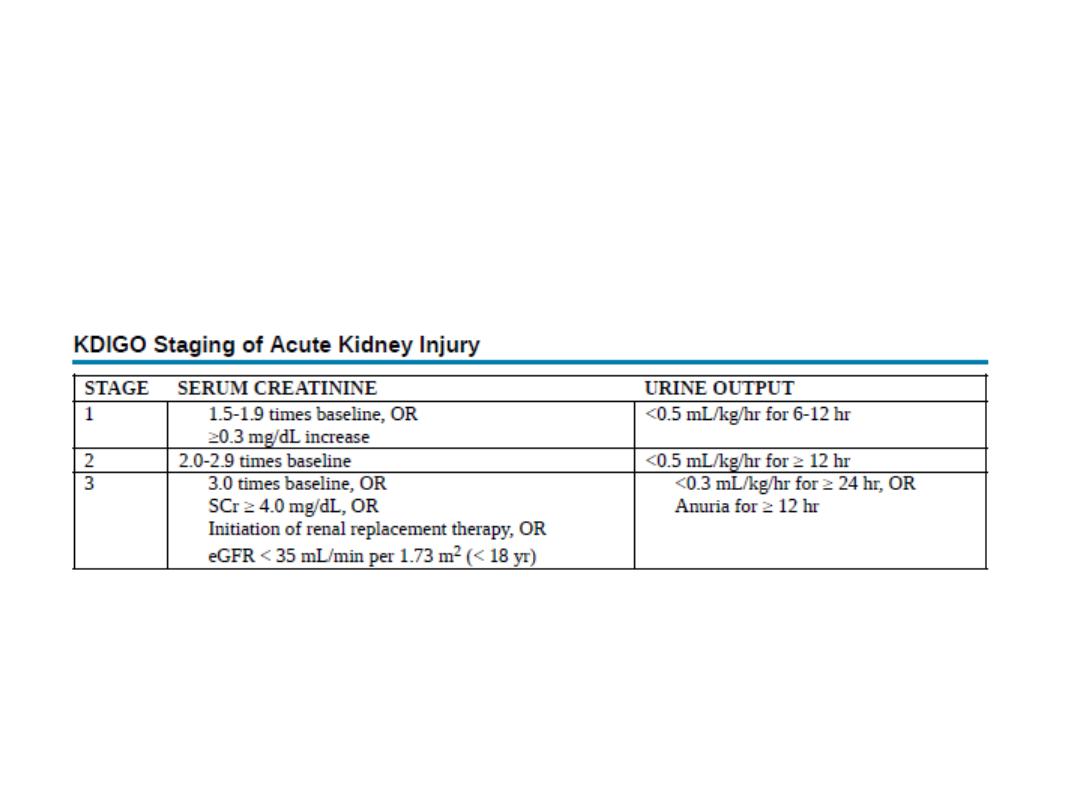
A classification system proposed by the Kidney Disease
Improving Global Outcomes (KDIGO) AKI Consensus
Conference takes both serum creatinine and urine output
criteria into account to define and stage AKI
Pathogenesis
AKI has been conventionally classified into three
categories: prerenal, intrinsic renal, and postrenal
PRERENAL
➢
Dehydration
➢
Gastroenteritis
➢
Sepsis
➢
Hemorrhage
➢
Hypoalbuminemia
➢
Cardiac failure
➢
Burns
➢
Capillary leak
➢
Cirrhosis
➢
Abdominal compartment syndrome
➢
Anaphylaxis

➢ INTRINSIC RENAL
➢ Glomerulonephritis
➢ Postinfectious/poststreptococcal
➢ Lupus erythematosus
➢ Henoch-Schönlein purpura
➢ Membranoproliferative
➢ Anti–glomerular basement membrane
➢ Hemolytic-uremic syndrome
➢ Acute tubular necrosis
➢ Cortical necrosis
➢ Renal vein thrombosis
➢ Rhabdomyolysis
➢ Acute interstitial nephritis
➢ Tumor infiltration
➢ Toxin and drugs
➢ Tumor lysis syndrome
➢ Vasculitis

POSTRENAL
➢ Posterior urethral valves
➢ Ureteropelvic junction obstruction
➢ Ureterovesicular junction
obstruction
➢ Ureterocele
➢ Tumors
➢ Urolithiasis
➢ Urethral strictures
➢ Hemorrhagic cystitis
➢ Neurogenic bladder
➢ Anticholinergic drugs

CLINICAL FEATURES
➢Vomiting, diarrhea 3 days
prerenal
➢ 6
years
child
with
recent
pharangitis+edema+HT=PSGN
➢ Critical ill child with protracted HT and HX of
exposure to nephrotoxin
ATN
➢ Neonate with hydronephrosis in prenatal U/S
congenital P UJ obstruction.
Physical examination
➢ Volume status, tachycardia, dry mouth, poor
peripheral circulation,
prerenal cause
➢Peripheral edema, basal creptation, gallop
rythem, suggest GN, ATN
➢Rash +nephritis=SLE, HSP

Laboratory findings
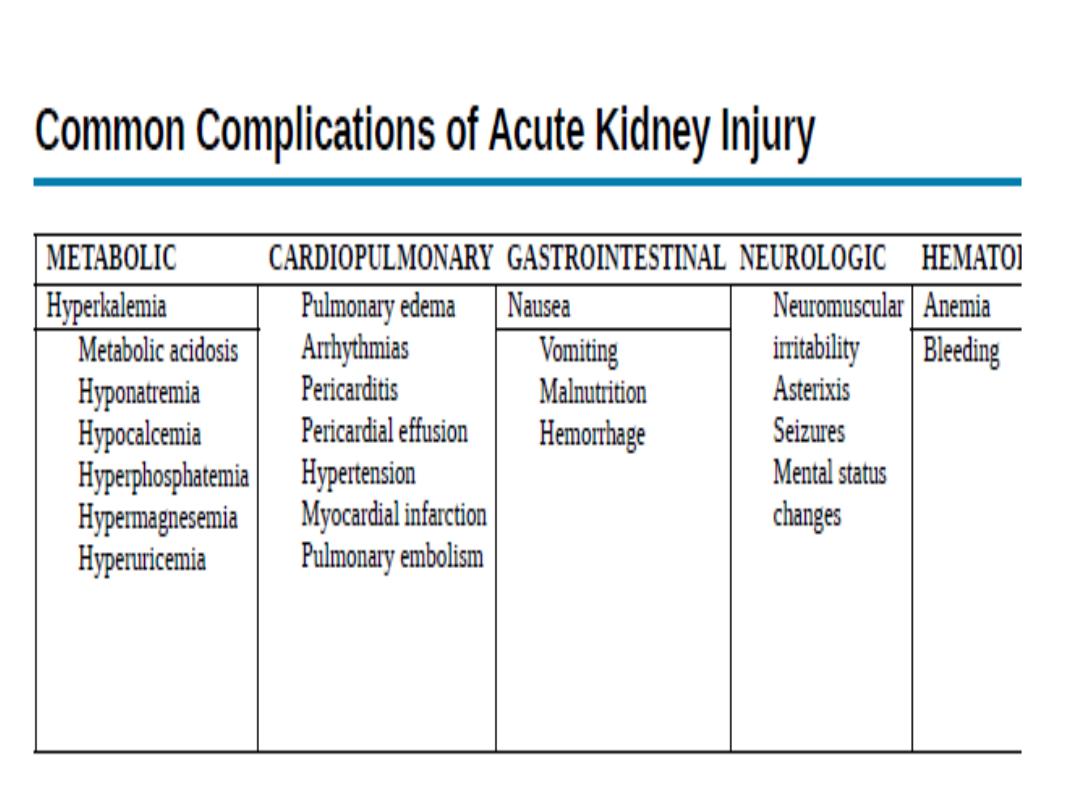
➢ Anemia due to 1- hemolytic(SLE, RVT, HUS)
2- delutional
➢ Leucopenia(SLE)
➢ Thrombocytopenia((SLE, RVT, HUS)
➢ Hyponatremia(delutional)
➢ Metabolic acidosis
➢ BUN, S.Cre
increase
➢ Uric acid , K+, Ph++, increase
➢ CA++ low
➢ C3
level
low
in(SLE,
PSGN,
radiation
GN,
membarenoprolefrative)
➢ Abs in PSGN
➢ GUA 1- RBC, protienurea, granuler cast,
internsic
cause
➢
2- WBC, WBC cast, low grade protienurea, RBC,
tubulointerstesial disease
➢ CXR cardiomegaly, pulmonary edema.
➢ Renal U/S
hydronephrosis, hydroureter, obstruction
➢ Renal biopsy may needed.

urinary indices may be useful in differentiation
of pre renal and internsic ARI
Indices
Pre renal
Sp.gravity
>1.020 <1.010
Ur.osmolality
>500 <350
Ur.NA+(Mag/L) <20 >40
FENA+ <1 >2
BUN/S.cre
>20 <20
FENA=Una X Pcre/P na X Ucre

Treatment
➢1-
Infant and children with obstruction or non ambulatory child
bladder catheter, to collect UOP
➢ 2-
fluid therapy
according to volume status
➢ A- in case of
Hypovolemia,
N/S 20 CC/kg within 30 min may be
repeated 2 or 3 times and watch the UOP in 2 hour , if no
possible of internsic or post renal.
➢ Diuretics indicated provided that good volume status
Frusamide
2-4 mg/kg+MANITOL 0.5g/kg
, if no UOP within 30 min ,
consider diuretic infusion
, if no UOP, consider
Dopamin
2-3Mg/kg/min with diuretic , if no UOP, stop diuretic and fluid
should be restricted.
➢ B-in case of
normal volemia
consider(insensible water loss) 400
cc/m2 /day + the fluid equal to the UOP.
➢ C- In case of
Hypervolemia
insensible water loss and UOP
should be omitted.
➢ Type of the fluid is glucose-containing solution
10-30%
as
maintaince .
➢ Input, output, UOP, chemistry should be checked daily

3- Hyperkalemia
>6mg/dl may lead to cardiac arrythemia
(ECG=tent
T wave , widing QRS, ST depression, and
arrest).
Indication of withholding of K+(fluid, diet)+Resin 1g/kg
orally or rectally by enema every 2-4 hour.
If >7mg/dl give the flowing
➢ Ca.gluconate 10% 1cc/kg within 3-5min
➢ NACO3 1-2cc/kg over 5-10min
➢ Reguler insulin 0.1U/kg with glucose 50% 1cc/kg
over 1hour.
If in spite of all these measure , still persistent
hyperkalemia
consider dialysis.
4-
Acidosis
if mild rarely need treatment , if sever PH
<7.15
NAHCO3 <8
with hyperkalemia
need
NAHCO3 infusion (desire PH 7.2, NAHCO3 12).
5-
Hypocalcemia
primarily treated by lowering S.PH++ ,
and Ca++ sh be not given I-V unless with tetany to ovoid
Ca . deposition in tissue, use Ca. carbonate 1-3 tab with
meal.

6-
Hyponatremia
delutional
need fluid restriction
, if <120 or symptomatic(seizure, lethargy )need
3%NACL .
NACL in m.ag required=0.6XBwt X (125- s.NA)
7-
Bleeding
due to platelet dysfunction, stress,
heparin(dialysis),
need oral or I.V H2 blocker
ranitidine
8-
HT
in GN, HUS, need salt and water restriction,
Nefidipine 0,25-0,5mg/kg every 2-6hour(max 10mg),
B.blocker,long acting
Ca.cannel blocker., if sever
crisis need NA nitropruside or Labetalol infusion.
9- Anemia
mild, delutional , packed RBC, 10 cc/kg
within 4-6hour if Hb <7g/dl(better fresh)
10-
nutrition
NA, PH, K, should be restricted in most
cases, protein should be
moderately decrease,
increase calorie intake.

Indications of Dialysis
1. -Volume over load +evidence of HT, and /or
pulmonary edema refractory to treatment
2. Persistent hyperkalemia
3. Sever acidosis unresponsive to treatment
4. Neurological symptoms(alter mental state ,
seizure)
5. BUN >100-150mg/dl or lower if rapidly
rising.
6. Ca/Ph imbalance with hypocalcemia tetany .
7. Inability to provide adequate nutritional
intake because of need for sever fluid
restriction.

Intermittent hemodialysis
Intermittent hemodialysis
➢ Is useful in patients with relatively stable hemodynamic status.
➢ This highly efficient process accomplishes both fluid and
electrolyte removal in 3-4 hr sessions using a pump-drive
nextracorporeal circuit and large central venous catheter.
➢ 3-7 times per week based on the patient’s fluid and electrolyte
balance.

Peritoneal dialysis
➢ Is most commonly employed in neonates and infants
with AKI
➢ Hyperosmolar dialysate is infused into the peritoneal
cavity via a surgically or percutaneous placed
peritoneal dialysis catheter.
➢ The fluid is allowed to dwell for 45-60 min and is then
drained from the patient by gravity (manually or with
the use of machine-driven
Cycling.
➢ Cycles are repeated for 8-24 hr/day based on the
patient’s fluid and electrolyte balance.
➢ Anticoagulation is not necessary.
➢ Contraindicated in patients with significant abdominal
pathology.

Continuous renal replacement therapy (CRRT)
➢ Is useful in patients with unstable hemodynamic status
➢ Concomitant sepsis
➢ Multi organ failure in the intensive care setting.
➢ CRRT
is an extracorporeal therapy in which fluid,
electrolytes, and small- and medium-size solutes are
➢ continuously removed from the blood (24 hr/day) using a
specialized pump-driven machine. Usually, a double-
lumen catheter is placed into the subclavian, internal
jugular, or femoral vein

THANK YOU
