URINARY INCONTINENCE
major problem for older adults, affecting up to 30% of community-dwelling elders and 50% of nursing home residentsaffects women twice as commonly as men at ages <80 yo
>80 yo, sexes are equally affected
Risk factors
Advanced age
functional impairment
Dementia
Obesity
Smoking
affective disorder
Constipation
certain medical illnesses (such as chronic obstructive pulmonary disease and heart failure),
history of pelvic surgery
DRIIIPP
Reversible Conditions Associated with Urinary IncontinenceDelirium
Restricted mobility—illness, injury, gait disorder, restraint
Infection—acute, symptomatic urinary tract infection
Inflammation—atrophic vaginitis
Impaction—of feces
Polyuria—diabetes, caffeine intake, volume overload
Pharmaceuticals—diuretics, -adrenergic agonists or antagonists, anticholinergic agents (psychotropics, antidepressants, anti-Parkinsonians)
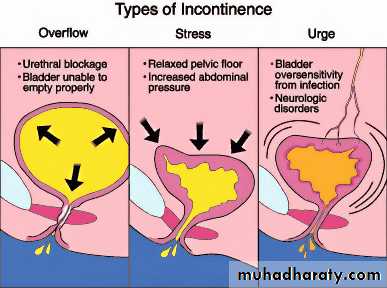
Stress Incontinence
results when the urethral sphincter mechanisms are inadequate to hold urine during bladder fillingleaking small amounts of urine during activities that increase intraabdominal pressure: coughing, laughing, sneezing, lifting, or standing up
most common causes of stress incontinence in women are insufficient pelvic support due to childbearing, gynecologic surgery, and the decreased effects of estrogen on tissues of the lower urinary tract
Diagnosis and treatment
History
Stress test
Surgical intervention
Pelvic muscle exercise
Urge Incontinence
detrusor overactivity (DO)characterized by uninhibited bladder contractions and is the most common form of UI in older adults
Described by patients as: uncontrollable need to void
Urinary frequency and nocturnal incontinence
particularly accompanied by loss of larger urine volumes (>100 mL)
Etiology – urge incontinence
may be idiopathic, associated with lesions of the central nervous system, such as a stroke, or be due to bladder irritation from infection, stones, or tumors
Diagnosis – urge incontinence
Measurement of postvoid residual (PVR) should be part of an incontinence evaluation in all patients
the patient's bladder is catheterized 5–10 min after the patient has voided
PVR > 200 mL suggests detrusor underactivity or obstruction
Treatment – urge incontinence
bladder retraining by encouraging the patient to void every 2 hourstry urgency control by sitting or standing quietly while focusing on allowing the urgency to pass before slowly walking to the bathroom
anticholinergic drugs, oxybutinin and tolterodine, which cause bladder relaxation
Mixed Incontinence
refers to UI where symptoms of both stress and urge incontinence are presentOverflow Incontinence
due to either bladder outlet obstruction or an atonic bladder
Male patients, but rarely females, may complain of dribbling after voiding
an continuing urge to urinate, or straining to urinate
palpable distended bladder
Etiology – overflow incontinence
Prostatic hypertrophy, prostate cancer, and urethral stricturescystocele can cause this problem in women
spinal cord disease, autonomic neuropathy of diabetes, alcoholism, vitamin B12 deficiency, Parkinson's disease, tabes dorsalis, or chronic outlet obstruction
Diagnosis and treatment – overflow incontinence
Urodynamic testing
distinguishing urethral obstruction from detrusor underactivity
For obstruction: surgical removal of the obstruction
BPH: terazosin, doxazosin, or tamulosin