SUBfertility
Dr.SumeyaObgectives
This lecture explain the definition ,types, causes, investigations and lines of treatments for both male and female infertilityBackground
Definition:Infertility = “failure to conceive following 1 year of unprotected intercourse if under 35 years of age or six months if over 35”.
• 10-15% couples affected
• Etiology
• Couples:
• 16% Tubal and pelvic pathology
• 21 % Male problems
• 29% Ovulatory dysfunction
• 18% Unexplaine
• 7% Endometriosis,2%Cervical,3%Uterine,4%Multiple
•
For a woman with a normal menstrual cycle of 28 days, ovulation occurs around day 14. The average survival time of the oocyte is around 24 hours, while after ejaculation sperm may survive for up to 7 days in the female reproductive tract.
Background
Normal couple:25-30% chance of pregnancy per ovulatory cycle
• Primary -Couple has never conceived
• Secondary - couple has had at least one prior conception
Infertility
Time of Exposure % Pregnant3 months 60%
6 months 70%1 year 85%
18 months 90%
Approach to Infertility
Causes
Male
Female
Combined
Unexplained
Male Infertility
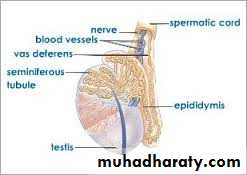
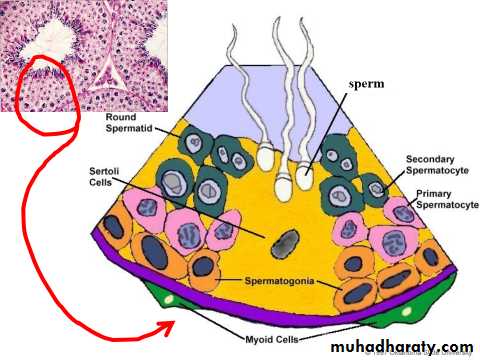
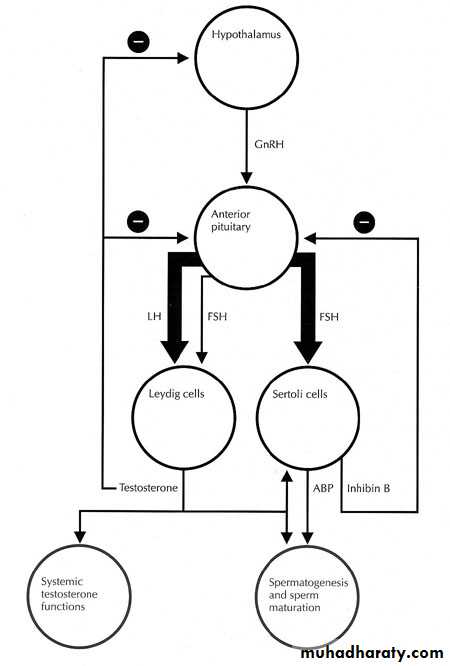
Anatomy of the testisHypothalamic-Pituitary-Gonadal Axis
Male Infertility
HypothalamusCongenital abnormalities of hypothalamus
e.g. Kallman’s syndrome
Starvation, stress or severe illness
Tumors (craniopharyngioma, metastatic tumor)
Head injury
Inflammation (sarcoidosis)
Infection (tuberculosis)
XRT
Drugs: marijuana,
Male Infertility
PituitaryEndocrine: thyroid, prolactin
Tumors
Inflammation: sarcoidosis, meningitis
Infiltration
Infarction
Trauma/XRT
Drugs: anabolic steroids
Male Infertility
Testis:Congenital: Klinefelters (XXY), developmental disorders
Disorders of gonadal steroidgenesis
Infection: chlamydia, prostatitis, mumps orchitis
Autoimmune
Cryptorchidism
Tumors; chemo/XRT
Drugs / alcohol
Vascular: testicular torsion
Male Infertility
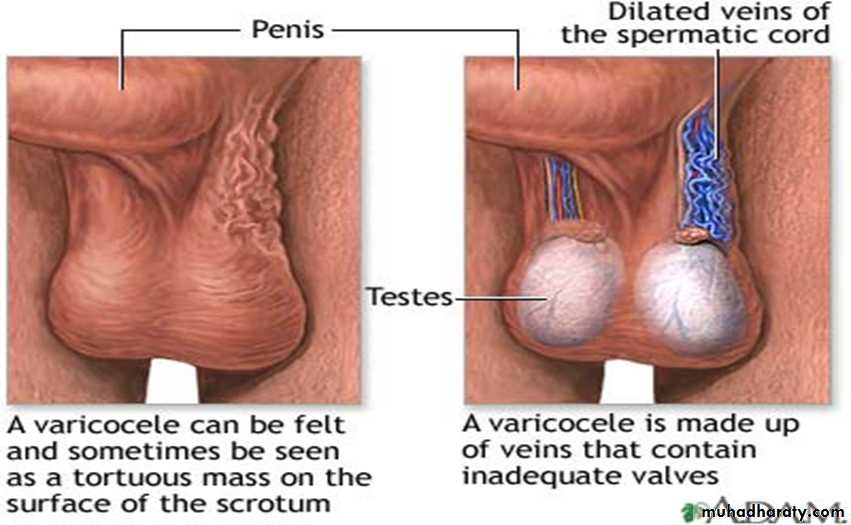
TemperatureRise in scrotal temperature
Occupation
Varicocoele
Male Infertility
Post testicular causes:• Impotence/Ejaculation
• A-Neurogenic: medications (α-blockers, methyldopa)
• B-Endocrine: diabetes
• Congenital: absence vas deferens (CF)
• Genetic: cystic fibrosis
• Primary ciliary dyskinesia: Kartagener syndrome
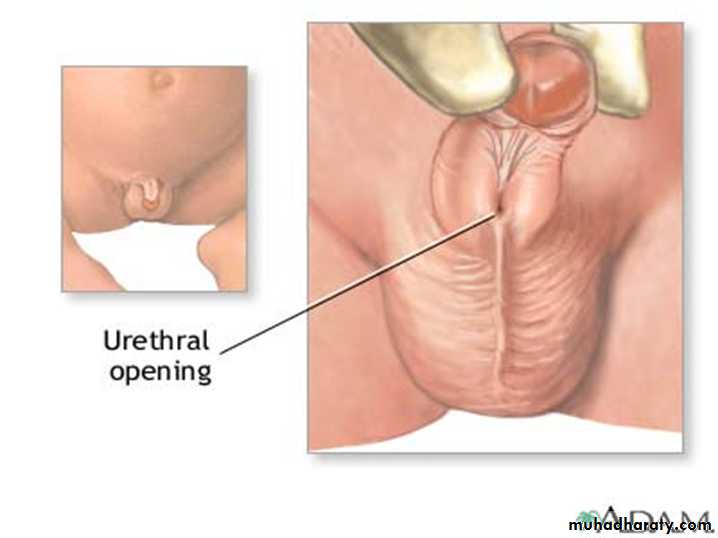
• Hypospadia
• Vasectomy
•
Male Infertility
Investigations:semen analysis
Abstain 2-7 days prior
At least 2 samples over different period of time
If abnormal:
Blood work: FSH, LH, TSH, testosterone, PRL
Testicular U/S
Chromosomal analysis
Semen
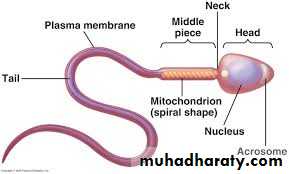
• also known as seminal fluid, is an organic fluid that may contain spermatozoa. It is secreted by the gonads ( testis and accessory sex glans). Seminal fluid contains several components besides spermatozoa: proteolytic and other enzymes as well as fructose are elements of seminal fluid which promote the survival of spermatozoa, and provide a medium through which they can move or "swim".
Male Infertility
Semen analysis: Macroscopical characteristics:Liquefaction time:
• Liquefaction time is a natural change in the consistency of semen from a semi liquid to a liquid. . In evaluation of liquefaction, ejaculate is placed in an incubator at 37°C and allowed to be liquefied. Liquefaction time more than 60 minutes or no liquefaction longer is pathologic
. Semen viscosity:
• Normal semen has a viscous texture.. High viscosity may affect sperm motility and concentration. Appearance of the ejaculate:
• A normal ejaculate has a homogenous grey-opalescent appearance.
Semen volume:
• The lower reference limit for semen volume is 1.5 ml (WHO 2010). Semen pH:• A lower threshold value is 7.2
Microscopic characteristics
• Agglutination
• Agglutination of spermatozoa means that motile spermatozoa stick to each other, head to head, midpiece to midpiece, tail to tail, or mixed, e.g. midpiece to tail.
The major types of agglutination (WHO 2010):
• grade 1: isolated <10 spermatozoa per agglutinate, many free spermatozoa.• grade 2: moderate 10–50 spermatozoa per agglutinate, free spermatozoa.
• grade 3: large agglutinates of >50 spermatozoa, some spermatozoa still free.
• grade 4: gross all spermatozoa agglutinated and agglutinates interconnected.
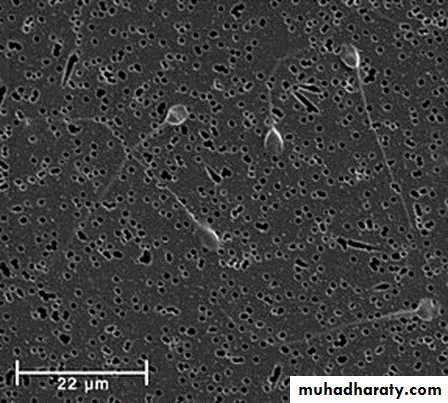
Sperm count and concentration
• According to WHO2010, the lower reference limit for sperm concentration is 15 × 106 spermatozoa per ml and the lower reference limit for total sperm number is 39 × 106 spermatozoa per ejaculate. A sperm concentration of less than this value is regarded as abnormal .Sperm motility
• The percentage of motile spermatozoa and their progressiveness usually give a good indication on sperm quality and are important in predicting men fertility . Several studies have demonstrated the correlation of motility with the fertilization rate in vivo and in vitro .
• Categories of sperm movement (WHO 2010):
• Progressive motility (PR):
• Non-progressive motility (NP):• Immotility (IM):.
Lower reference limit (WHO 2010):
• The lower reference limit for total motility (PR + NP) is 40%.
• The lower reference limit for progressive motility (PR) is 32%.
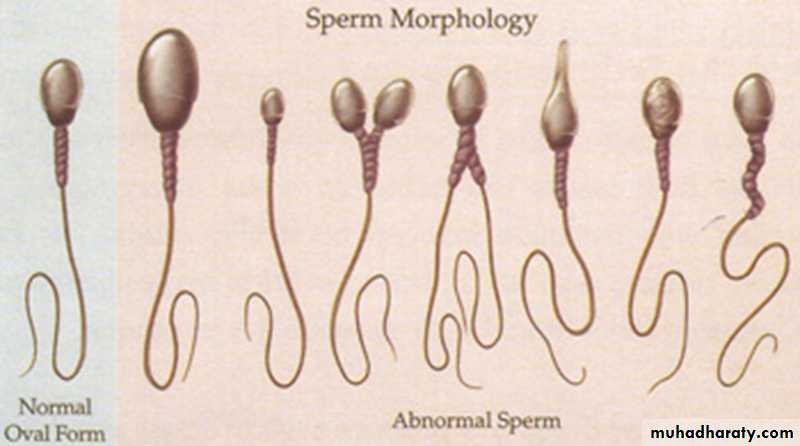
Sperm morphology
• The reference value for normal sperm morphology determined by Kruger is >4% .Sperm vitality
It is especially important for samples with less than about 40% progressively motile spermatozoa. The lower reference limit for vitality (membrane-intact spermatozoa) is 58 %( WHO 2010).Round cell count (cells other than spermatozoa)
• .The semen sample with <5 round cells/ HPF was considered normal .Endocrine Tests
The endocrine assessment of an infertile man includes measurements of serum testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH), and perhaps other tests:• Serum Testosterone
• Measurement of a morning serum total testosterone is usually sufficient. In men with borderline values, the measurement should be repeated and measurement of serum-free testosterone may be helpful.
• Serum Luteinizing Hormone and Follicle-Stimulating Hormone
• When the serum testosterone concentration is low, high serum FSH and LH concentrations indicate primary hypogonadism and values that are low or normal indicate secondary hypogonadism.
Other Hormones
• Serum prolactin should be measured in any man with a low serum testosterone concentration and normal to low serum LH concentration. Although inhibin assays are not widely available outside of research laboratories, low serum inhibin concentrations may be an even more sensitive test of primary testicular dysfunction than high serum FSH concentrations, provided the assay is specific for inhibin B.TERMINOLOGY
• Oligozoospermia; sperm conc. less than 15 × 106 spermatozoa per ml• Teratozoospermia; normal sperm morphology is <4% kruger strict criteria
• Asthenozoospermia; total motility (PR + NP) < 40% or progressive motility (PR) < 32%.
• Azoospermia; no sperm in ejaculate
• Aspermia; no semen
Male Infertility
Tx / Interventions:Treat underlying causes
Intrauterine Insemination (IUI)
Intracytoplasmic Sperm Injection (ICSI)
TREATMENT
Treatment of male infertility involves the couple.• Specific endocrine treatment is available for men whose infertility results from hypogonadotropic hypogonadism. Hypogonadotropic hypogonadism due to hyperprolactinemia can often be corrected and fertility restored by lowering the serum prolactin concentration. If the hyperprolactinemia results from a medication, as is often the case, that medication should be discontinued, if possible. The hyperprolactinemia is caused by a lactotroph adenoma. It should be treated with a dopamine agonist, such as cabergoline or bromocriptine. The process of spermatogenesis normally takes 3 months. As a result, restoration of a normal sperm count usually does not occur for at least 3 and sometimes 6 months or more after the serum prolactin and testosterone concentrations have returned to normal.
• In some patients, who have a lactotroph macroadenoma, the hypogonadotropic hypogonadism appears to be the result of permanent damage to the gonadotroph cells by the mass effect of the adenoma. Gonadotropin treatment should be instituted for these patients.
• Gonadotropin therapy: Treatment is initiated with human chorionic gonadotropin (hCG), 1,500–2,000 IU three times per week subcutaneously or intramuscularly for at least 6 months. hCG has the biologic activity of LH. The hCG dose should be adjusted upward according to symptoms of hypogonadism, serum testosterone concentrations, and semen parameters.
• Some patients with acquired hypogonadotropic states can be stimulated with hCG alone to produce sufficient sperm. If after 6–9 months the patient remains azoospermic or severely oligospermic, then human menopausal gonadotropin (hMG) or recombinant FSH should be added.
• • Pulsatile GnRH treatment: Pulsatile subcutaneous or intravenous treatment with GnRH has also been successfully used to treat gonadotropin deficient patients. GnRH has to be delivered in pulses using a portable pump with an attached catheter and needle for many months or years; most patients find it inconvenient to use GnRH therapy for so long.
Genital infection
• Infertile men rarely present with symptoms or signs of acute genital infections or prostatitis, but they are sometimes diagnosed as having infections of the urogenital tract by the presence of increased leukocytes in the semen. Despite the absence of symptoms, we typically treat patients who have leukospermia, even if the culture is negative, with at least a 10-day course of antibiotics such as erythromycin or trimethoprim-sulfamethoxazole. A second course of therapy is usually given if leukocytes persist in the semen after antibiotics.Sperm Autoimmunity
• Continuous or intermittent high doses of prednisone (from 40 mg/ day to 80 mg/day) for up to 6 months have been shown in placebo-controlled trials to improve cumulative pregnancy significantly in partners of men with sperm autoantibodies.• However, many patients cannot tolerate this regimen because of the adverse effects of high-dose corticosteroid therapy. As a result, most couples prefer to try an assisted reproductive technique, such as ICSI, as primary treatment for sperm autoimmunity.
Empirical Therapy
• Many treatments have been used empirically for male infertility, including clomiphene citrate and other hormones and vitamins.• Aromatase inhibitors may improve sperm concentrations in men with severe oligozoospermia or azoospermia prior to sperm retrieval for ICSI.