Connective tissue diseases
Dr. Ahmed Abdulhussein AL-HuchamiConnective Tissue diseases:
Are groups of clinico pathological conditions involve connective tissue of most systems of the body, include mainly LE, scleroderma, systemic sclerosis, dermatomyositis, MCTD &others…Lupus Erythematosus:
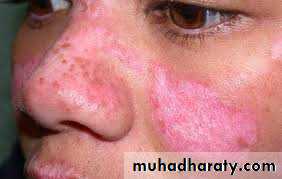
is an autoimmune disorder resulting from an interplay of genetic, environmental &hormonal elements with a heterogeneous clinical expression extending from a localized cutaneous form to a life threatening systemic form.LE is a spectrum of diseases, in one end of spectrum: DLE is purely cutaneous LE, at the other end :SLE. In the middle of spectrum: sub acute LE, neonatal LE, complement deficiency LE& drug-induced LE .
Pathogenesis
Infectious agent e.g viral cross react with self-antigen in person with genetic backgroundExacerpating factors:
Ultraviolet lightSex hormones
Stress
SLE criteria(4 out of 11)
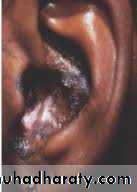
Malar(butterfly) rashDiscoid lesions
Photosensitivity
Oral ulcer
Arithritis
Serositis e.g. pleuritis, pericarditis
Renal: proteinuria, casts
Neurological: psychosis, seizure
Hematological: decreased platelets, WBC or RBC
Immunological: anti-DNA, anti-Sm, antiphospholipid antibodies
ANA
Drug-induced SLE
It is different from idiopathic SLE by (1) presence of anti-histone antibodies instead of ANAMost commonly implicated drugs:
ProcainamideHydralazine
Minocycline
INH
Penicillamine
TNF- inhibitors
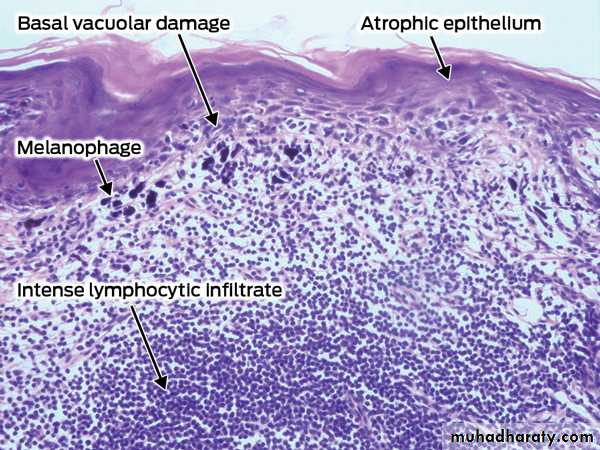
Pathology
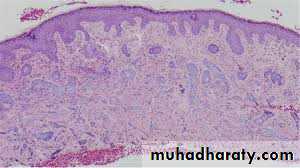
Colloid bodies (damaged keratinocytes)Vacuolar changes in basal layer
Epidermal atrophy
Thickenening of basement membrane
Peri-adnexal, upper and lower dermal lymphocytic infiltrate
Mucin deposition
DIF (direct immunofluorescence) show granular deposit at DE junction (lupus band)a and around adnexa
Treatment
General: avoidance of sun and ppt factorSpecific :
Topical: Sun protection, topical and intralesional steroids
Systemic: Antimalarial e.g. hydroxychloroquine, chloroquine
Others: retinoids, thalidomide, dapsone
Morphea
Affect female more than maleDoes not affect survival but can cause a disability especially the linear type
Fibroblast isolated from morphea lesion produce increased amount of collagen and this is thought to be due to production of IL-4 and TGF-β by T-cells
Some believes that Borrelia plays a role
Types
1. Plaque-type : present as white indurated plaque surrounded by lilac border2. Deep morphea: invlove deep dermis, subcutis +/- fascia
3. Generalized morphea: plaques coaleasce affecting the entire trunk except nipple, can involves the extremities, it is disabiling causing difficulty in breathing,
4. Linear morphea: Mostly affect children
Variants:En coup de sabre type linear morphea of head, can involve muscle, bone
Parry-Romberg syndrome: hemifacial atrophy including eyes and tongue(the most severe form)
Diagnosis
Autoantibodies: ANA and anti-ssDNA are commonly seen in linear and generalized typesPathology: hyalinized and eosinophilic collagen bundles with a little space in between and atrophy of hair follicles and sweat glands
Treatment
Topical :Vit D analogues e.g. calcipotriol
Systemic treatment:
Glucocorticoids, methotrexate ,PUVA (psoralen plus UVA) and UVA1
Others: penicillin, penicillamine, acitretin , calcitriol and IFN-γ
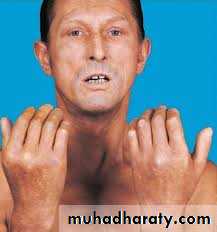
scleroderma:systemic sclerosis
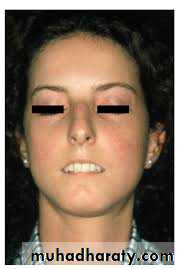
Cutaneous manifestations of scleroderma:1. Hardening of skin (hard to pinch)
2. Microstomia (hard to open mouth) with furrowing around mouth
3. Beaking of nose
4. Loss of facial expression
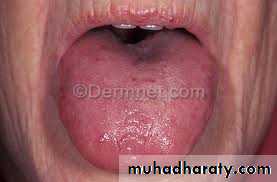
5. Telangiectasia of skin, lip and tongue
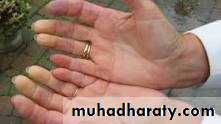
6. Ulcers and necrosis of finger tips
7. Calcinosis cutis (deposition of calcium in skin, subcutaneous tissue and muscle)
8. Nail fold telangiectasia