1
Poisoning by specific pharmaceutical agents
Analgesics
Paracetamol (acetaminophen)
Toxicity is caused by an intermediate reactive metabolite that binds
covalently to cellular proteins,
causing cell death. This results in hepatic
and occasionally renal failure. In therapeutic doses, the toxic
metabolite is detoxified in reactions requiring glutathione, but in
overdose, glutathione reserves become exhausted.
Management
Activated charcoal may be used in patients presenting within 1
hour.
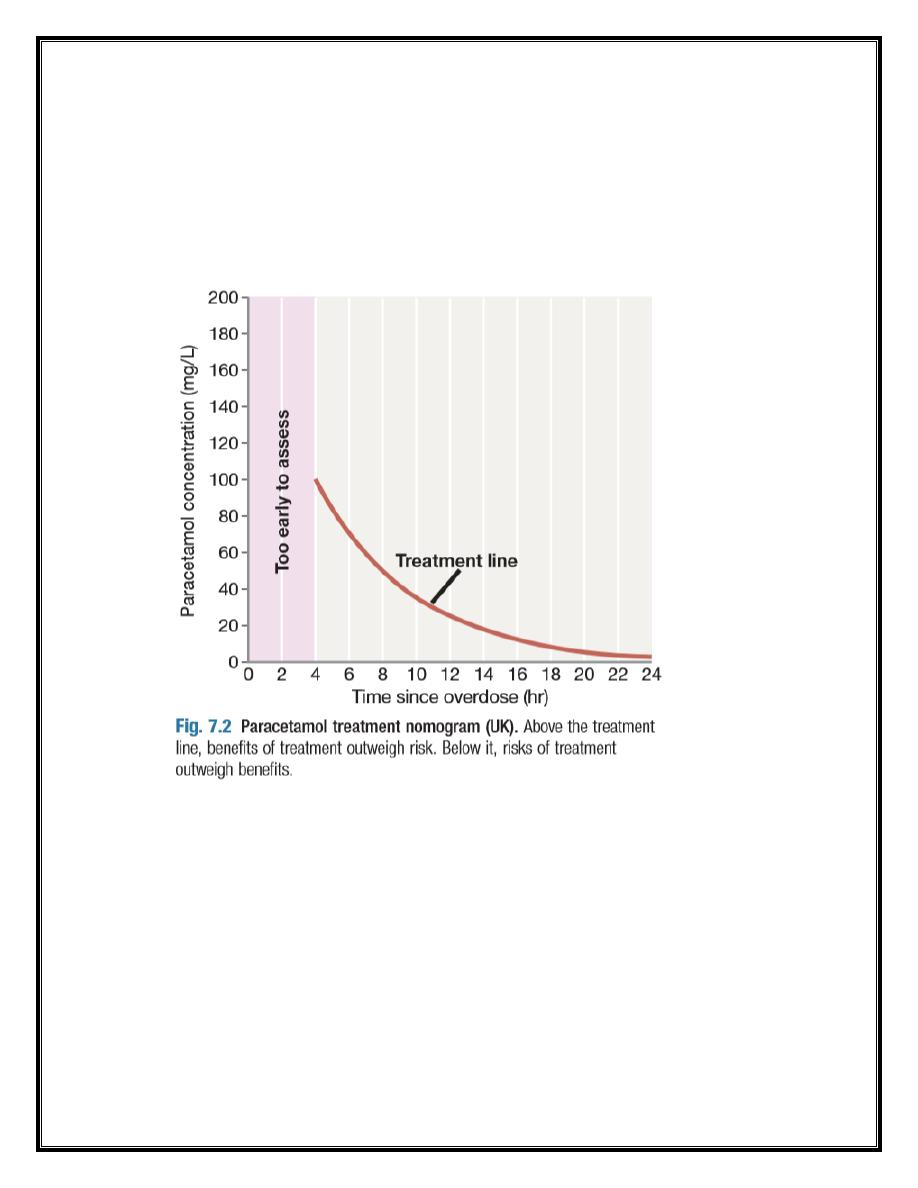
Antidotes for paracetamol act by replenishing hepatic glutathione
and should be administered to all patients with acute poisoning
and paracetamol concentrations above a ‘treatment line’.
The Acetylcysteine given intravenously (or orally in some
countries) is highly efficacious if administered within 8 hours of
the overdose. However, efficacy declines thereafter, so
administration should not be delayed in patients presenting after
8 hours to await a paracetamol blood concentration result. The
antidote can be stopped if the paracetamol concentration is
shown to be below the nomogram treatment line.
Anaphylactoid reactions are the most important adverse effects
of acetylcysteine and are related to dose-related histamine
2
release. Common features are itching and urticaria, and in severe
cases, bronchospasm and hypotension. Most cases can be
managed by temporary discontinuation of acetylcysteine and
administration of an antihistamine.
An alternative antidote is methionine 2.5 g orally (adult dose)
every 4 hours to a total of four doses, but this may be less
effective, especially after delayed presentation.
Liver and renal function, International Normalised Ratio (INR) and
a venous bicarbonate should also be measured. Arterial blood
gases and lactate should be assessed in patients with reduced
3
bicarbonate or severe liver function abnormalities; metabolic
acidosis indicates severe poisoning.
Liver transplantation should be considered for paracetamol
poisoning with life-threatening liver failure .
If multiple ingestions of paracetamol have taken place over
several hours (‘staggered overdose’) or days (e.g. chronic
therapeutic excess), acetylcysteine may be indicated; specific
treatment recommendations vary between countries.
Salicylates (aspirin)
Clinical features Salicylate overdose commonly causes nausea,
vomiting, sweating, tinnitus and deafness.
Direct stimulation of the respiratory centre produces
hyperventilation and respiratory alkalosis. Peripheral
vasodilatation with bounding pulses and profuse sweating occurs
in moderately severe cases.
Serious poisoning is associated with metabolic acidosis,
hypoprothrombinaemia, hyperglycaemia, hyperpyrexia, renal
failure, pulmonary oedema, shock and cerebral oedema.
Agitation, delirium, coma and fits may occur, especially in
children.
Toxicity is enhanced by acidosis, which increases salicylate
transfer across the blood–brain barrier.
4
Management
Activated charcoal should be administered if the patient presents
within 1 hour. Multiple doses may enhance salicylate elimination
but are not routinely recommended.
The plasma salicylate concentration should be measured at least 2
(symptomatic patients) or 4 hours (asymptomatic patients) after
overdose and repeated in suspected serious poisoning, as
concentrations may continue to rise for several hours.
Clinical status, however, is more important than the salicylate
concentration when assessing severity.
Dehydration should be corrected carefully because of the risk of
pulmonary oedema.
Metabolic acidosis should be treated with intravenous sodium
bicarbonate (8.4%), after plasma potassium has been corrected.
Urinary alkalinisation is indicated for adults with salicylate
concentrations above 500 mg/L.
Haemodialysis is very effective for removing salicylate and
correcting associated acid–base and fluid balance abnormalities.
It should be considered when serum concentrations are above
700 mg/L in adults with severe toxic features, or in renal failure,
pulmonary oedema, coma, convulsions or refractory acidosis.
Non-steroidal anti-inflammatory drugs
Clinical features
Overdose of most non-steroidal anti-inflammatory drugs
(NSAIDs) usually causes only minor abdominal discomfort,
vomiting and/ or diarrhoea, but convulsions can occur
5
occasionally, especially with mefenamic acid. Coma, prolonged
seizures, apnoea, liver dysfunction and renal failure may follow
substantial overdose but are rare. Features of toxicity are unlikely
to develop in patients who are asymptomatic more than 6 hours
after overdose.
Management
Electrolytes, liver function tests and a full blood count should be
checked in all but the most trivial cases. Activated charcoal may
be given if the patient presents within 1 hour. Symptomatic
treatment for nausea and gastrointestinal irritation may be
needed.
