Clinical immunology L-4 Dr. Fadhil
Amyloidosis
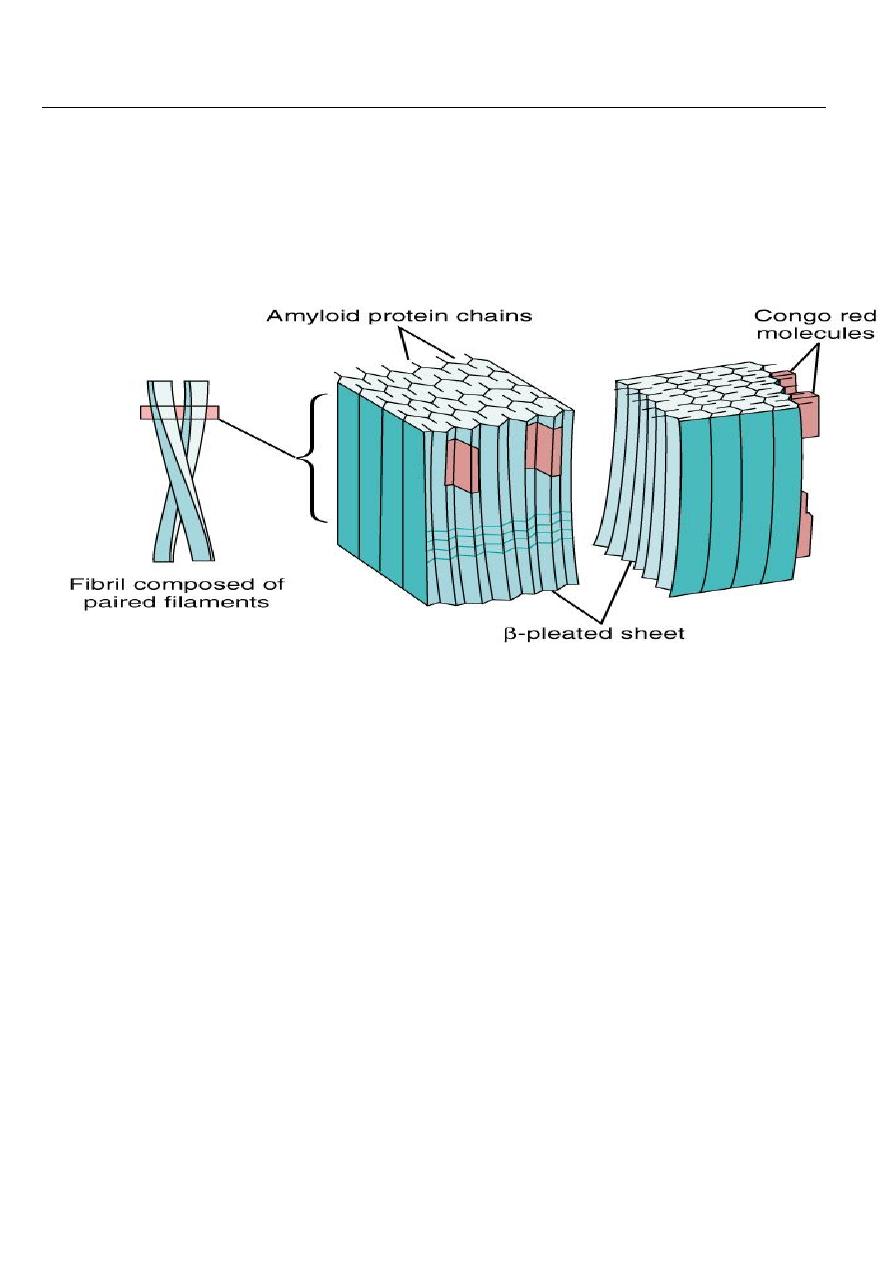
Is a disorder of protein metabolism in which there is an extracellular deposition of
pathological insoluble fibrillar proteins in organs and tissues. Characteristically, the amyloid
protein consist of
B-
pleated sheets that are responsible for its insolubility and resistance to
proteolysis.
Amyloidosis can be acquired or inherited. Classification is based on the nature of precursor of
plasma protein( at least 20) that form the fibrillar deposit. The process for the production of
the fibrils appears to be multifactorial and differs amongst the various types of amyloid.
This disease was named by Virchow in 1854 on the basis of color after staining with iodine
&sulfuric acid.
All amyloid proteins share a unique fibrillar ultrastructure.
amyloid proteins can be deposited locally or can involve virtually every organ system of the
body.
Amyloid fibril deposition may have no clinical consequences or may lead to severe
pathophysiological changes. Often the disease falls between these two extremes.
Regardless the etiology, the clinical diagnosis of amyloidosis is usually not made until the
disease is far advanced.
The clinical manifestations of amyloidosis depends on the organ(s) affected.
The diagnosis of amyloidosis should be considered in all cases of unexplained nephrotic
syndrome, cardiomyopathy, &peripheral neuropathy.

CLASSIFICATION
Amyloid diseases are classified by etiology and type of protein deposited.
1- acquired systemic amyloidosis
a- reactive(AA) (secondary) amyloidosis!
These are due to amyloid formed from serum amyloid A(SAA), which is an acute phase
protein. It is, therefore, related to chronic inflammatory disorders and chronic infections.
Clinical features depend on the nature of underlying disorder. Chronic inflammatory disorders
include rheumatoid arthritis, inflammatory bowel disease and untreated familial
Mediterranean fever.
In developing countries it is still associated with infectious diseases such as tuberculosis,
bronchiectasis and osteomyelitis. AA amyloidosis often presents with chronic kidney disease,
with hepatomegaly and splenomegaly. Macroglossia is not a feature and cardiac involvement
is rare.
The degree of renal failure correlates with SAA level in a more favourable out come in patients
with low normal levels.
b-light chain amyloid. (AL, primary) seen in patients with Myeloma and plasmacytoma.
It manifested as restrictive cardiomyopathy& peripheral neuropathy.
c- Dialysis related amyloidosis:
This is due to B2- microglobulin producing amyloid fibrils in chronic dialysis patients. It
frequently presents with carpal tunnel syndrome. It occurs 5-10 years after dialysis.
dialysis associated(A
B
2M) amyloidosis. Occurs 5-10 years of dialysis
d- senile systemic amyloidosis:
Usually asymptomatic& occurs in patients over the age of 70 years.
2-Familial(hereditary)amyloidosis: these are autosomally dominant transmitted diseases
where the mutant protein forms amyloid fibrils, starting usually in the middle age.
hereditary systemic amyloidosis: An autosomal dominant disorder& manifested as
peripheral& autonomic neuropathy& cardiomyopathy.
Examples include disorders such as familial amyloidosis polyneuropathy (FAP),
cardiomyopathy or the nephrotic syndrome. Major foci of FAP occur in Portugal, japan and
Sweden.
Local amyloidosis:
Deposits of amyloid fibril of various types can be localized to various organs or tissues(
skin, heart or brain).
•
The brain is a common site of amyloid deposition.
•
Intracerebral and cerebrovascular amyloid deposits are seen in Alzheimer’s disease
Diagnosis
the diagnosis is established by biopsy which may be of an affected organ , rectum or
subcutaneous fat.
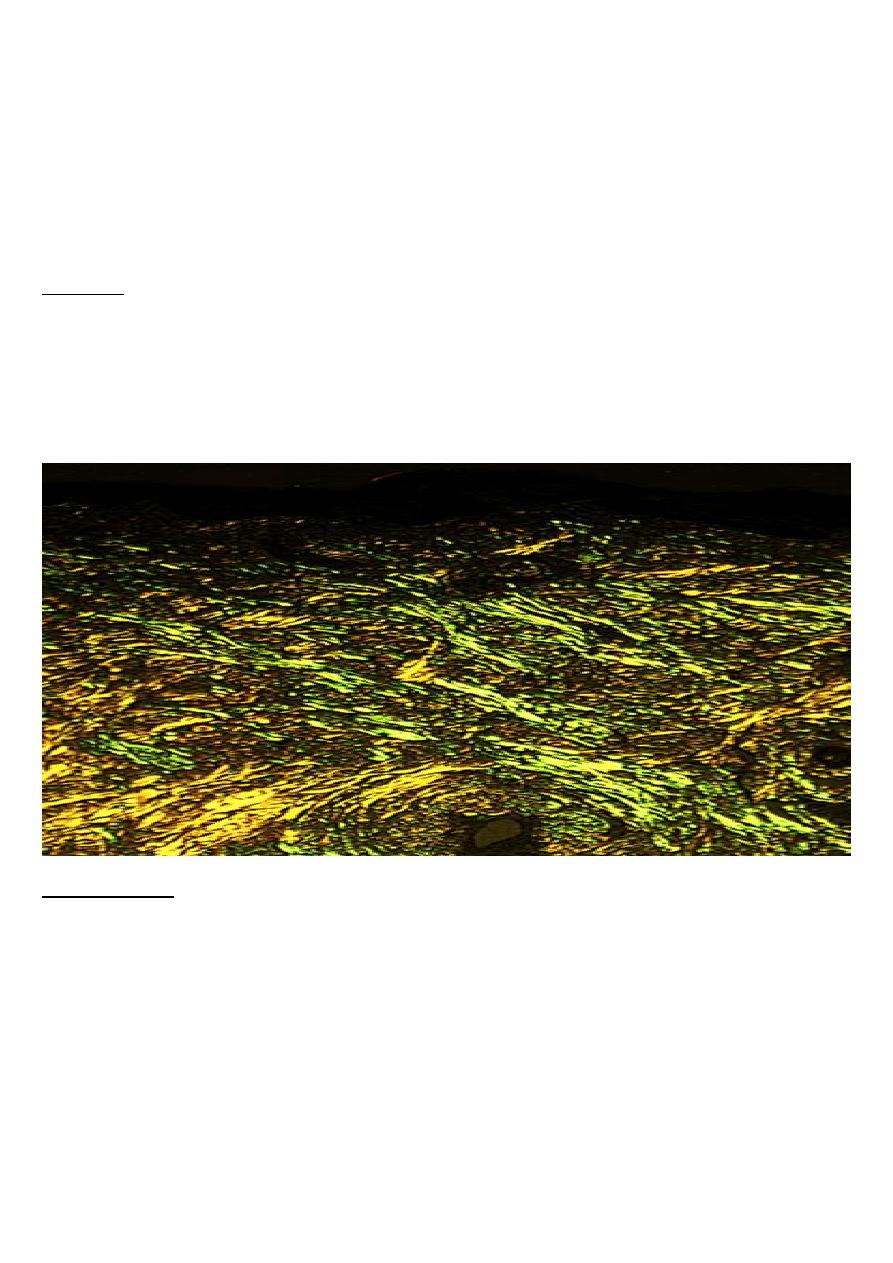
The pathognomonic histological feature is apple-green birefringence of amyloid deposits
when stained with Congo red dye and viewed under polarized light.
MANAGEMENT
the aims of treatment are to support the function of the affected organ and in acquired
amyloidosis to prevent further amyloid deposition through treatment of the primary cause.
Genetic counseling is an important aspect of treatment in heredofamilial amyloidosis.
Liver transplantation had been carried out since 1990 for patients with familial amyloid-
polyneuropathy(FAP).
Recent trials have indicated that a prednisolone/melphalan/ Colchicine's program can
prolongs the life.
AutoimmuneS diseases
•
Result from a failure of self-tolerance
•
Immunological tolerance is specific unresponsiveness to an antigen
•
All individuals are tolerant of their own (self) antigens
•
these disorders are chronic and usually irreversible
•
incidence: 5%-7% of population, higher frequencies in women, increases with age
Immunological tolerance
• This is the process by which the immune system distinguishes self from foreign tissues.
• Central tolerance occurs during lymphocyte development in the thymus and bone
marrow.
• T&B lymphocytes that recognize self antigens are deleted before they develop into fully
immunocompetent cells.
• Some autoreactive cells
• inevitably evade deletion &escaping to the peripheral circulation. These cells are
controlled through peripheral tolerance mechanisms.
• These include the suppression of autoreactive cells by 'regulatory' T-cells& the
generation of the hyporesponsivness 'anergy‘ in lymphocytes.
• Failure of any of these tolerance mechanisms may result in the development of
autoimmune disease.
Factors predisposing to autoimmune disease
Both genetic and environmental factors contribute to the development of autoimmune
disease.
The most important genetic determinants of autoimmune susceptibility are the HLA genes,
reflecting there importance in shaping of lymphocyte responses.
Several environmental factors can trigger autoimmunity in genetically susceptible
individuals.
The most widely studied of these is infection, as occurs in acute rheumatic fever fallowing
streptococcal infection or reactive arthritis fallowing bacterial infection.
A number of mechanisms have been postulated including cross- reactivity between the
infectious pathogen and self determinants(molecular mimicry), and release of sequestered
antigens which are not usually visible to the immune system from damaged tissue.
Occasionally the development of autoimmune disease is a side effect of drug treatment,
for example:
the metabolic products of the anesthetic drug halothane bind to liver enzymes, resulting in
a structurally novel protein.
This is recognized as new(foreign) antigen by the immune system causing hepatic necrosis.
HLA-association in autoimmune disease
Disease HLA-ASSOCIATION
CLASSIFICATION OF AUTOIMMUNE DISEASE
TYPE
DISEASE
•
Organ specific
Immune response Directed against
Localized antigens
•
Grave's disease
•
Addison's dis.
•
Pernicious
•
anemia
•
Type-1 diabetes
•
Pemphigus vulgaris
•
Idiopathic thrombocytopenic
•
purpura
•
Autoimmune hemolytic anemia
•
Myasthenia gravis
•
Rheumatoid arthritis
•
Dermatomyositis
•
primary biliary
•
cirrhosis
Ankylosing spondylitis B27
Type-1 diabetes DR3/4
Rheumatoid arthritis DR4
Grave's disease DR3
Myasthenia gravis DR3
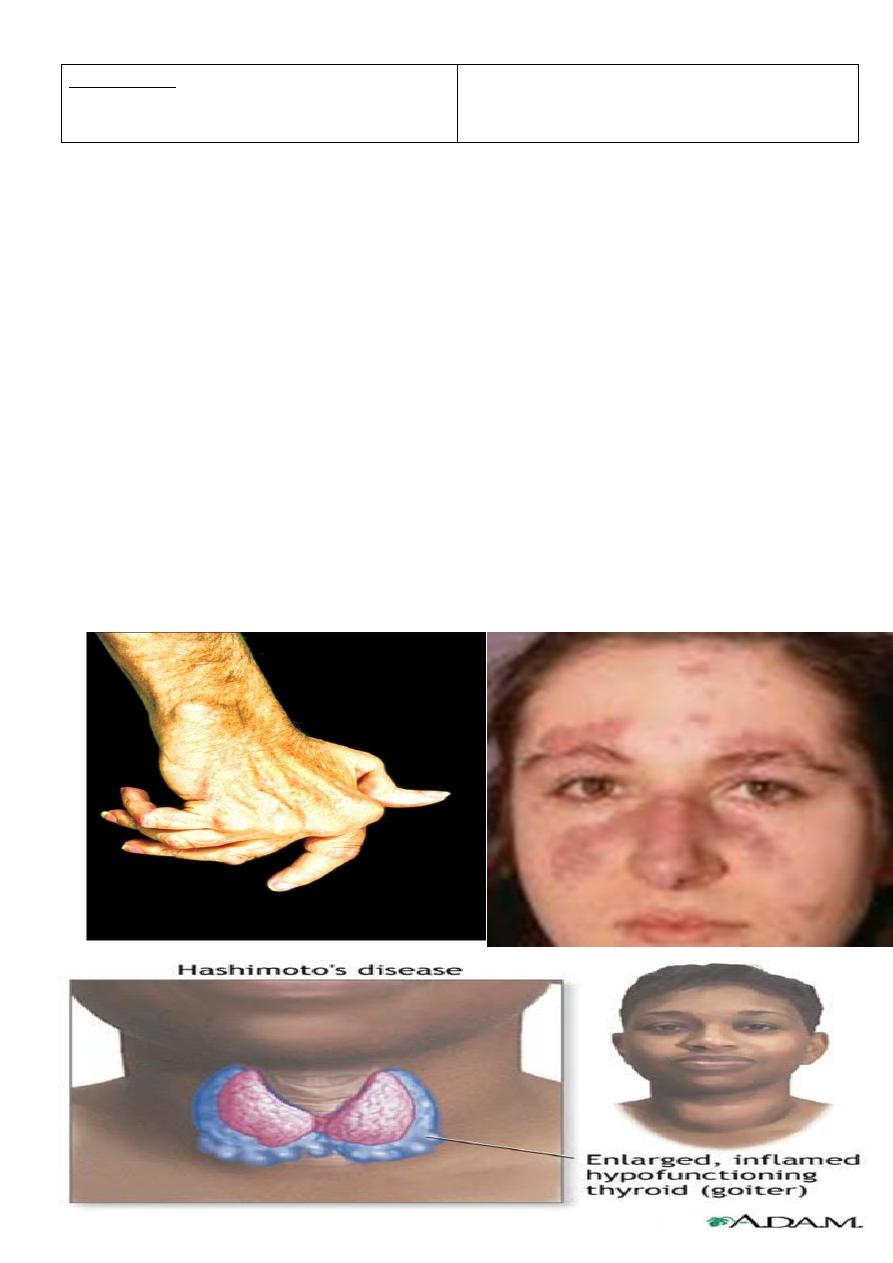
Multisystem
Immune response directed to
widespread target antigens
•
Systemic sclerosis
•
Mixed connective tissue disease
•
SLE
Treatment of autoimmune diseases
Treatment aimed at:
•
Killing dividing cells
-Immunosuppressant
•
Controlling T cell signaling
–
Cyclosporin
•
Anti-inflammatory medications
–
Cortisone-like steroids
•
Replacement therapy
–
Insulin
