Peripheral nerve injuries
Dr. Jamal Al-Saidy
Assistant Professor and Consultant Orthopaedic Surgeon
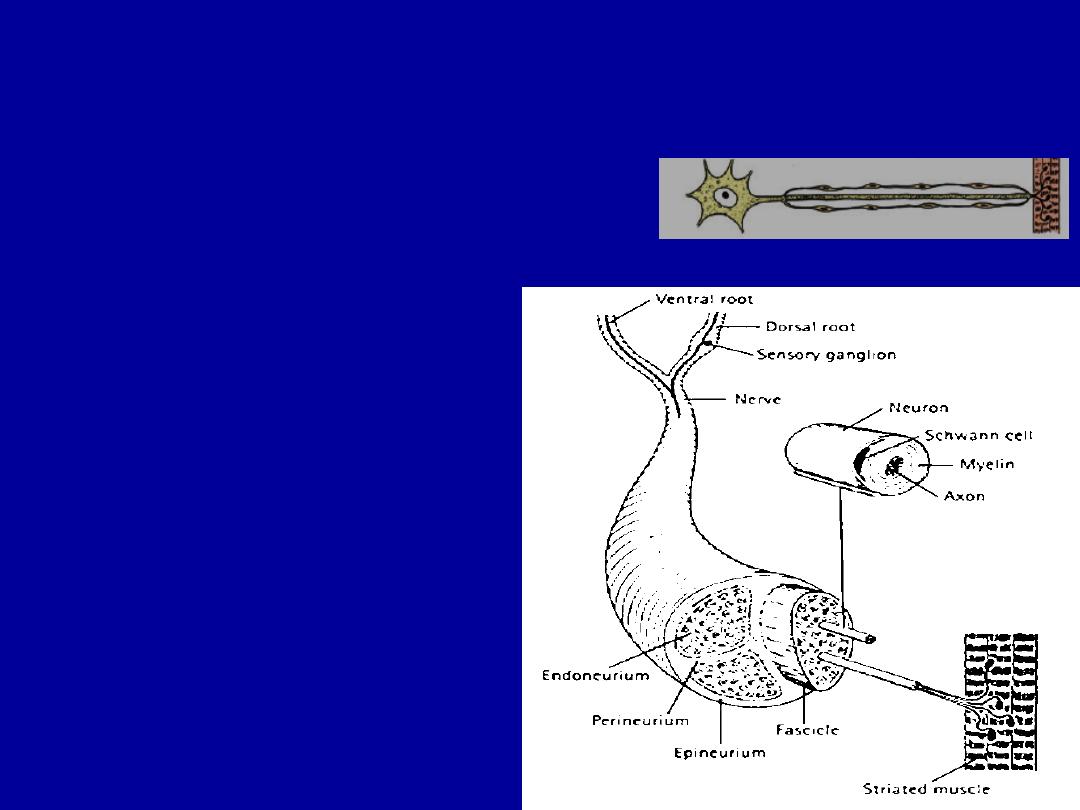
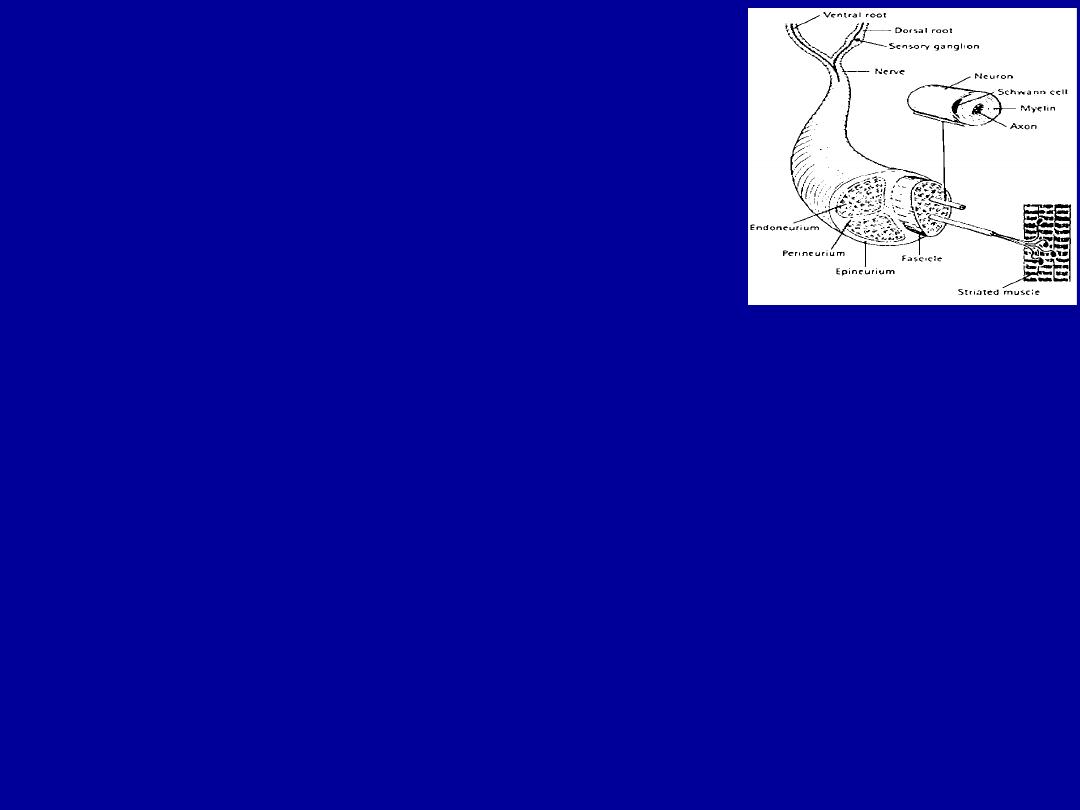
Connective tissue covers
Endoneurium :
covers axon outside Schwann cells
Perineurium :
lies between fascicles.
Epineurium :
covers the whole nerve
Myelin :
Lipoprotein
Secreted by Schwann cells
Insulator
Accelerates the action potential

Causes
:
Cutting
Ischaemia.
Compression .
Traction.
Laceration.
Burning.

T
ypes of N.injurey
Sedon,s description– old classification
.
(1) Transient ischaemia
Acute N.compression for :-
( 15 minutes) numbness and tingling.
( 30 minutes) loss of pain sensibility.
( 45 minutes ) muscle weakness.
Relief of compression is followed by
intense paraesthesiae lasting up to 5 minutes .
Restoration for sensation ( 30 sec ) and ( 10
minutes ) for full muscle power.
These changes are due to transient anoxia and they leave no trace of
nerve damage
.
. (

( 2 )
Neuropraxia
Reversible physiological nerve conduction block.
loss some types of sensation and muscle power.
spontaneous recovery after a few days or weeks.
it is due to mechanical pressure causing segmental
(local)demyelination.
e.g . . Crutch palsy , Saturday night palsy ,
tourniqet palsy.
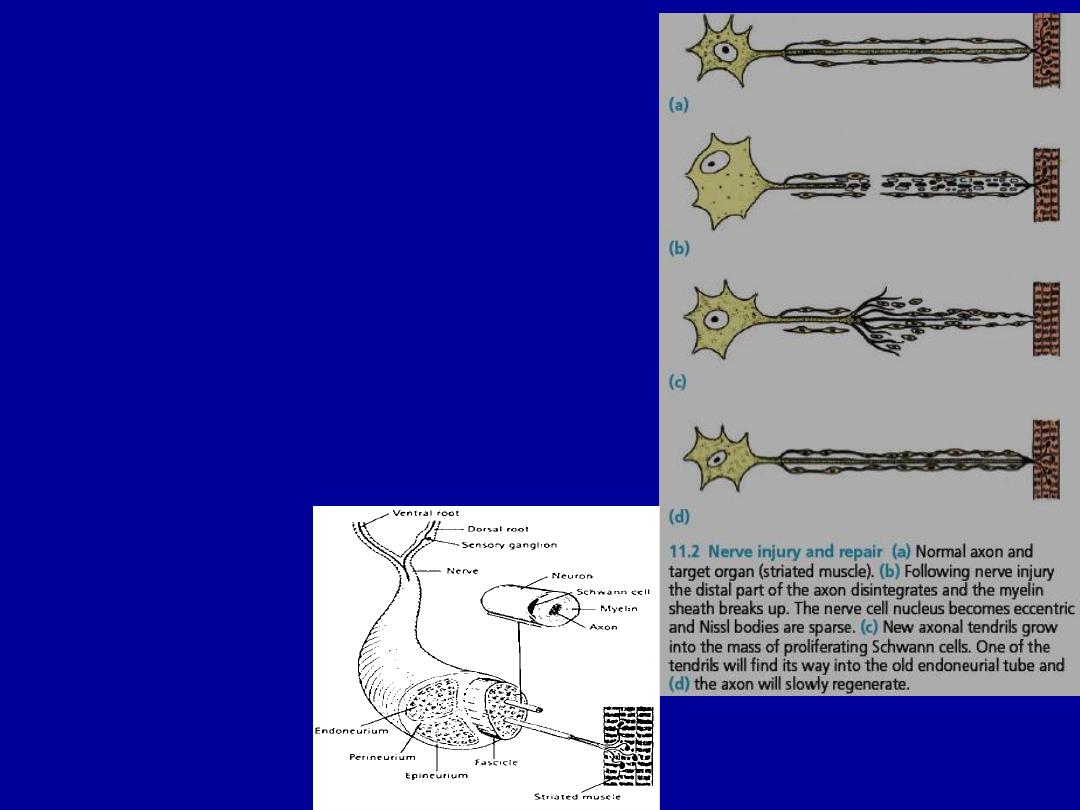
(3) Axonotmesis
More severe .
Axonal interruption.
Neural tube are intact.
Loss of conduction.
The nerve is in continuity.
Closed fracture and dislocation.
Wallerian degeneration :
Distal to the lesion, and for
a few millimetres retrograde, axons disintegrate and are resorbed by phagocytes
Axonal regeniration
started within hrs with a speed
of1mm per day.
Px : good
– fair
Division of the nerve trunk.
Open wound
If no re-innervation occurs within 2 yrs motor
end plates & sensory receptors atrophy
& will never recover.
Neuroma :
a knot formed by regenerating axons,
proliferating Schwann cells & fibroblasts .
Px : poor
(4) Neurotmesis :

The double crush phenomenon
(Peripheral entrapment syndromes are often associated
with cervical or lumbar spondylosis).
There is convincing evidence that proximal compression of a
peripheral nerve renders it more susceptible to the effects of a
second, more peripheral injury. This may explain why peripheral
entrapment syndromes are often associated with cervical or
lumbar spondylosis. A similar type of ‘sensitization’ is seen in
patients with peripheral neuropathy due to diabetes or alcoholism.

Classification of nerve injuries
:- (
sunderland 1978
)
First degree:
•transient ischaemia .
•Neurapraxia.
•Reversible.
Second degree:
•Axonotmesis.
•endoneurium is preserved.
•Complete recovery without the need for intervention.

-
Third degree
:
•Worse than axonotmesis .
•Endoneurium is disrupted.
•Perineurial sheaths are intact and internal damage is limited
.
Fourth degree:
• only the epineurium is intact.
•Internal damage is severe.
•Recovery is unlikely.
•The nerve repaired or grafted.
Fifth degree:-
•The nerve is divided completely, must be repaired.

Clinical features of N.inj
Acute
n.i :
are easily missed.
Always test for n,i and v.i.
Numbness ,Paraesthesia ,Muscle weakness.
Abnormal posture ( e.g wrist drop in r.n,palsy ).
The neurological examination must be repeated at intervals.
In chronic N.i
The anaesthetic skin may be smooth and shiny.
Evidence of diminished sensibility(e.g burns , ulcers).
Lack of sweating.
Muscular wasting.
Fixed postural deformities.

Grading Of Muscle Power
Grad ( 0 ) : - no contraction .
Grad ( 1 ) : - a flicker of activity .
Grad ( 2 ):- muscle contraction but unable to overcome g
Grad ( 3 ) ; - muscle contraction able to overcome gravity
Grad ( 4 ) : - contraction against resistance .
Grad ( 5 ) : - normal power .

Principles of treatment
Nerve exploration:
if
the nerve seen to be divided.
type of injury(knife,a high energy injury)
delayed recovery :
After closed # : if threre is nerve injury 90
% it is neurapraxia and a F/U for 2-3 months usually recovery If
not NCS & EMG if signs of axono or neurotemesis
exploration & repair
Conditions should be dealt with before the nerve lesion
Vascular injury, unstable fracture, contaminated
soft tissue and tendon divisions
Closed low energy injuries usually recover
spontaneously.
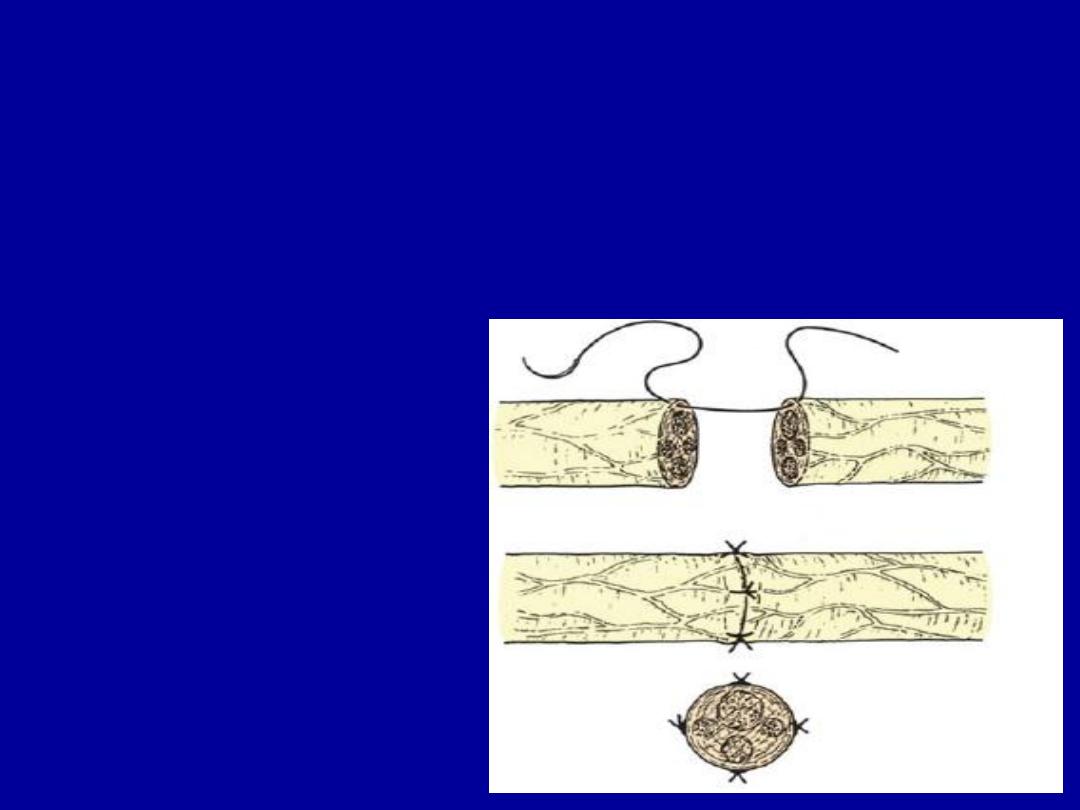
Primary repair
Advided nerve is best repaired as soon as this
can be done safely because :-
-
No retraction.
- No rotation.
- No fibrosis.

Delayed repair
Late repair weeks or months after injury
may be indicated because :-
1. No sign of recovery at the expected time.
2. Missed diagnosis.
3. Late presentation.
4. failed Primary repair.

Nerve grafting
•Free autogenous N.G .
•To bridge gaps too large for direct
suture.
•Sural .n is most commonly used.
•Up to 40 cm can be obtained from
each leg.

Nerve transfer
• Spinal accessory n. can be transferred to
the suprascapular n.
• Intercostal ns. Can be transferred to the
musculocutaneous n.

Care of paralysed parts
•Protection.
•Movement.
Tendon transfers
•
Considered when motor recovery is not occur.

Prognosis
Depend on : -
Type of the lesion
: -
- neurapraxia always recovers fully.
- axonotmesis may or may not .
- neurotmesis will not unless repaired.
level of the lesion
: -
The higher the lesion the worse is the prognosis
.
Type of the nerve
:
-
purely motor or purely sensory recover better than mixed nerves.
Size of gap
: -
Above the critical resection length ,end to end suture is not
successful and a graft is needed.
Age
: -
children do better than adults
.
Delay in suture
:-
The best result with early repair.
Surgical techniques
:
Skill, experience, suitable facilities.
Associated lesions
of vessels, tendons, causes unuseful limb.

Entrapment syndromes
A compression of a peripheral nerve where it passes through a fibro-
osseous tunnel.
Causes
Idiopathic
Pregnancy
Menopause
Myxoedema
RA
Local factor (osteophyte, ganglion..)

Sites
Carpal tunnel syndrome (median)
Cubital tunnel syndrome (ulnar)
Tarsal tunnel syndrome (tibial)
Inguinal ligament (lateral cutaneous)
Thoracic outlet (roots of brachial plexus)

Pathology
• ↓ blood flow
• ↓ axonal conduction
• Local demyelination
• Endoneurial fibrosis
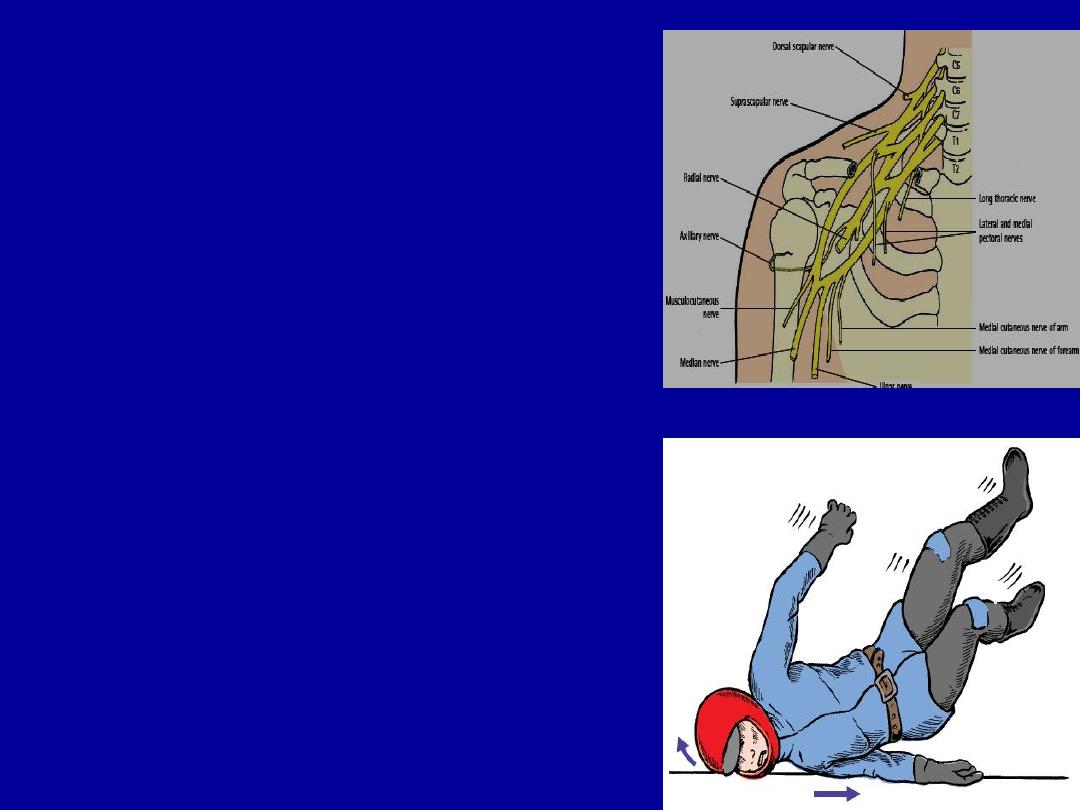
Brachial plexus injury
Nerve roots of
( C5 to T1 ) .
Stab wound or severe traction
caused by a fall on side of neck
or the shoulder.
Preganglionic lesion:-
disruption proximal to the dorsal root
ganglion, cannot recover and surgically
irreparable.
Postganglionc lesion:-
distal to D.R.G, surgically reparable
and potentially capable of recovery.
The injuries
are often overshadowed by other,
life-threatening trauma such as rupture of the
subclavian or axillary artery.
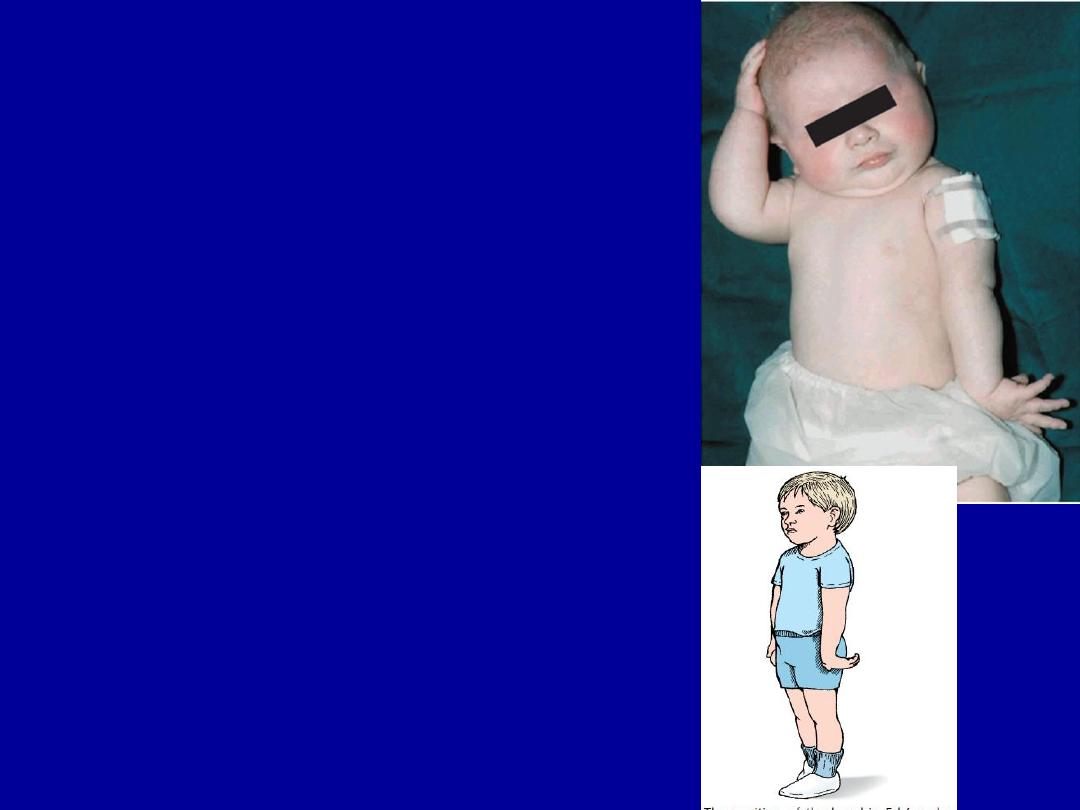
Obstetrical B.P palsy
Excessive traction on plexus during child birth
Upper root inj.(
Erb’s palsy)
C5-C6 and sometimes C7.
Paralysis of the abductores and external rotators
of the shoulder and supinators.
The arm is held to the side ,internally rotated and
pronated.There may also be loss of finger extension.
Usually complete recovery occurs
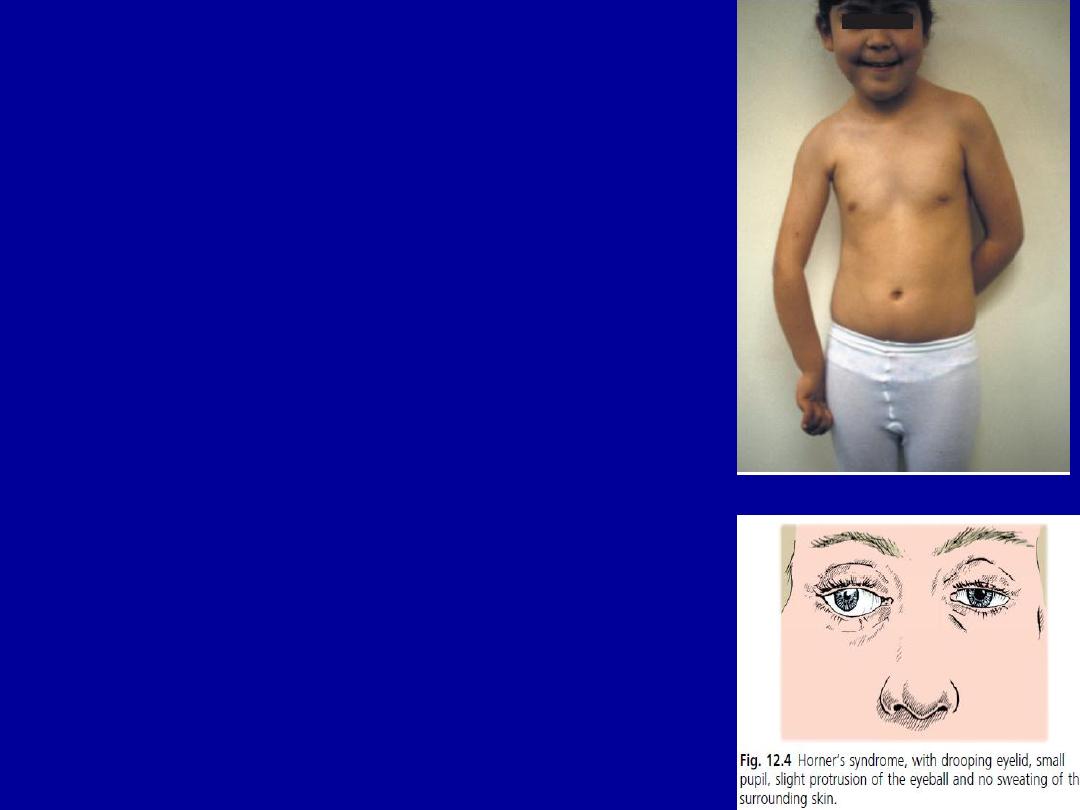
Lower root B.P inj.
(
Klumpke’s palsy)
C8 and T1.
The arm supinated and the elbow flexed.
Loss of intrinsic muscles power in the hand.
Reflexes are absent .
May be unilateral Horner syndrom.
Usually in breech delivery

Total plexus inj
Less common but more severe.
Complete plexus lesion.
The arm is flail, pale.
All finger muscles are paralyzed.
X-rays should be taken to exclude fractures.

Management
May be
Recover completely.
Improve.
Unaltered
.
While waiting for recovery, physiotherapy is contenued.The relaible
indicator of improvement is return biceps activity by 3 months.
Operative intervention should be considered if there is no biceps
recoverey.

Long thoracic nerve
injury
• C5,6,7
• In mastectomy
• Winging of scapula
(Paralysis of serratus anterior)
• Wall test

Acessory spinal nerve injury
C2-6
Stab wound in posterior triangle
Iatrogenic, L.N biopsy
Drooping of shoulder
Cannot shrug shoulder
C5-C6)
)
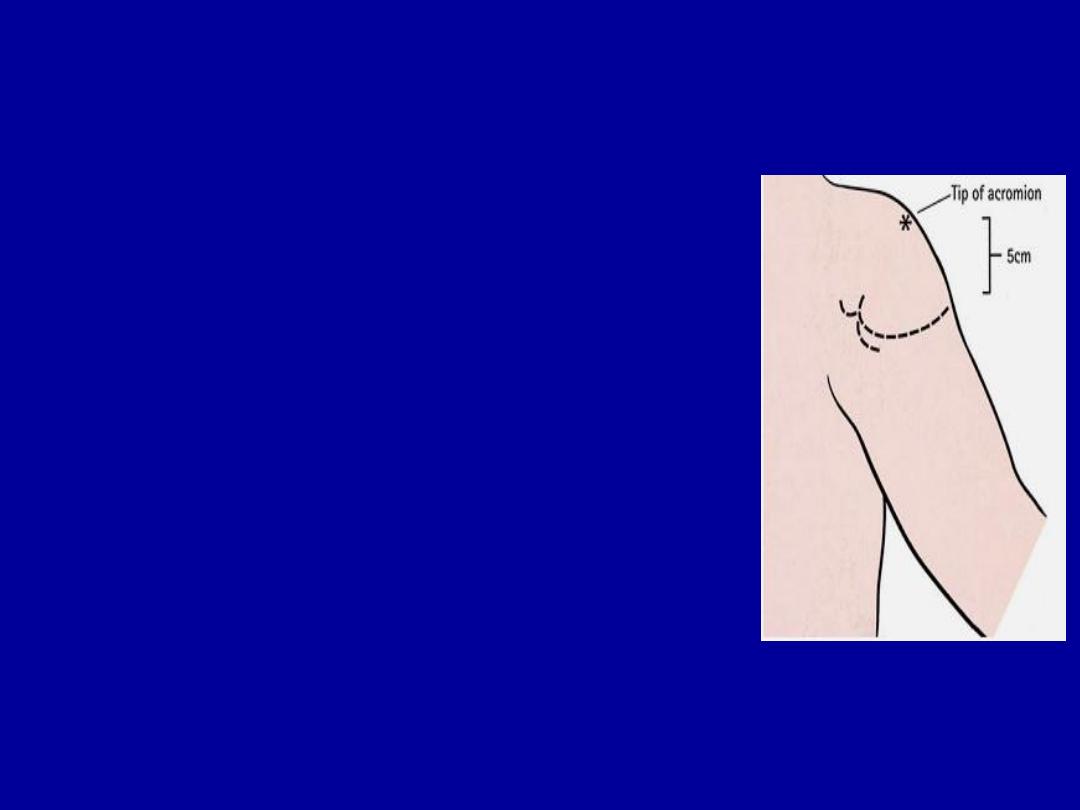
Axillary nerve
Post.cor of B.P.
Shoulder dislocation or proximal humerus #
Shoulder weakness.
Deltoid wasting.
Failure to maintain abduction + anaesthesia over deltoid
80% of cases recovers spontaneously.
If no sign of recovery by 6 to 8 weeks,EMG should be
performed and N.exploration.
Radial nerve C5-T1
I. Low lesions :- elbow
Fractures, dislocations, wound,
iatrogenic injury.
loss of MP extension
Weakness of abduction and
interphalangeal extension of the
thumb.
Wrist extension is preserved.

II. High lesion :- arm
Fractures of humerus, prolonged
tourniquet pressure.
Inability to extend M.P joints
Wrist drop
Sensory loss of a small patch on the dorsm around the anatomical
snuffbox.

III.
Very high lesion :- axilla
Trauma, Operations, Chronic compression in the
axilla(Saturday-night palsy , crutch palsy).
In addition to weakness of the wrist and hand, the
triceps is paralysed and the triceps reflex is absent.

Treatment of R.N.L
Open injuries :-
explored and repaired or grafted as soon as possible.
Closed injuries :-
waiting for 12 weeks if not improved, then EMG
, the nerve should be explored.
Iatrogenic injury :-
repaired or grafted without delayed.
While recovery
is awaited physiotherapy is continued and hand
splints is used.
Tendon transfers :-
if recovery does not occur
Pronator teres to the short radial extensor of the wrist.
F.c.r to the long finger extensors.
Pal. longus to the long thumb abductor.

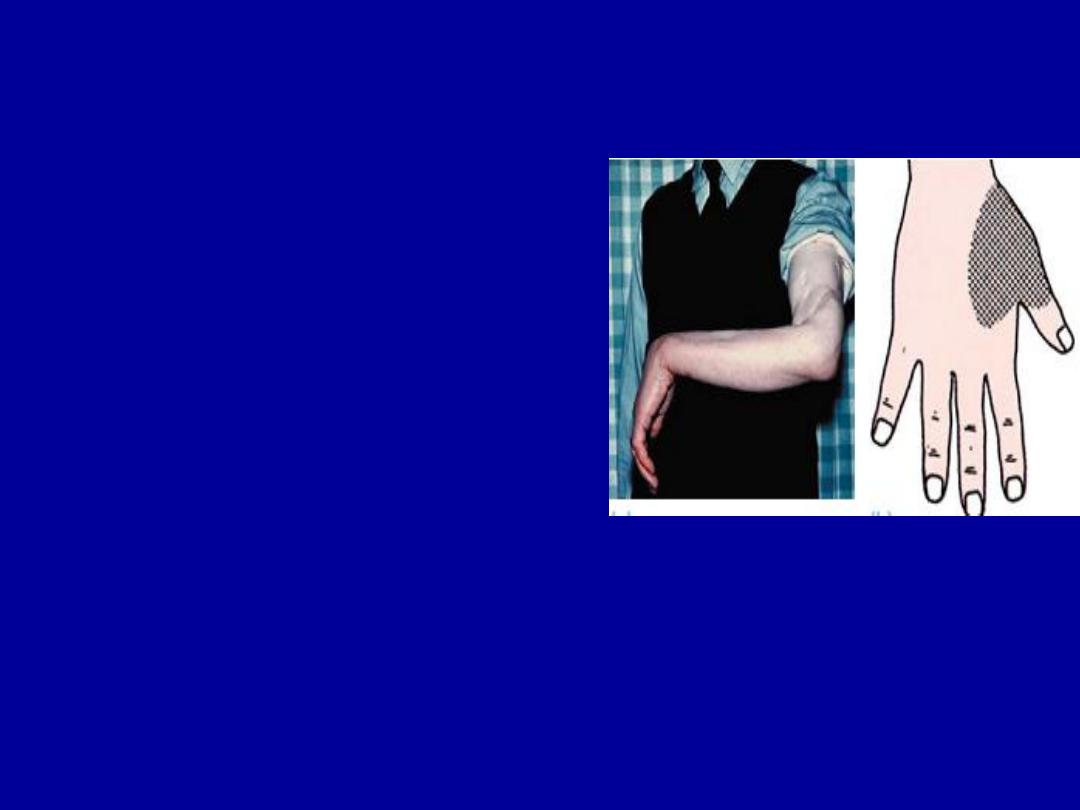
Ulnar Nerve C8-T1
Low lesion:-
Cutting at the wrist.
Numbness of the ulnar one and a half fingers.
→→→→→→→→
Claw hand deformity(hyperextnsion of the m.p joints of the
ring and little fingers, due to weakness of the intrinsic muscles .
Wasting of the hypothenar and interosseous.
→→→→→→→→
Weak finger abduction and loss thumb adduction(difficult pinch)
→
Froment’s sign +ve because add.p.is weak and f.p.l is
being used.
→→→→→→→→→→→→→→→→→→→→→

High lesion
Occur in elbow F or D.
Motor and sensory loss are the same as in a low lesion,
but the hand is not markedly deformed(less clawed)
because the ulnar half of flexor d.p is paralysed. (the
‘high ulnar paradox’).
Treatment:
- exploration(repair,suture,graft).
-anterior transposition of ulnar N.
-protection and physiotherapy.
-tendons transfers.

Median Nerve
C5-T1
Low lesion
Cuts in front of the wrist, carpal dislocation.
Unable to abduct the thumb and the sensation is
lost over the radial three and a half digits.
In long standing cases the thenar eminence is
wasted and atrophic changes may be seen.

High lesion
Forearm fractures, elbow dislocation, stabs, gunshot
wounds.
The signs are the same of the low, but the hand is held
with ulnar fingers flexed and the index straight (pointing
sign).
Loss of apposition
cannot do
(OK) .

Treatment
Exploration(repair, suture, graft).
Physiotherapy.
Tendon transfers

Femoral Nerve
Injured by gunshot, pressure, traction, bleeding.
Unable to extend the knee.
Numbness of the anterior thigh and medial aspect of
the leg.
Knee reflex is depressed.
Treated by suturing, grafting, caliper to stabilize the
knee or tendon transfers of hamstring to quadriceps.
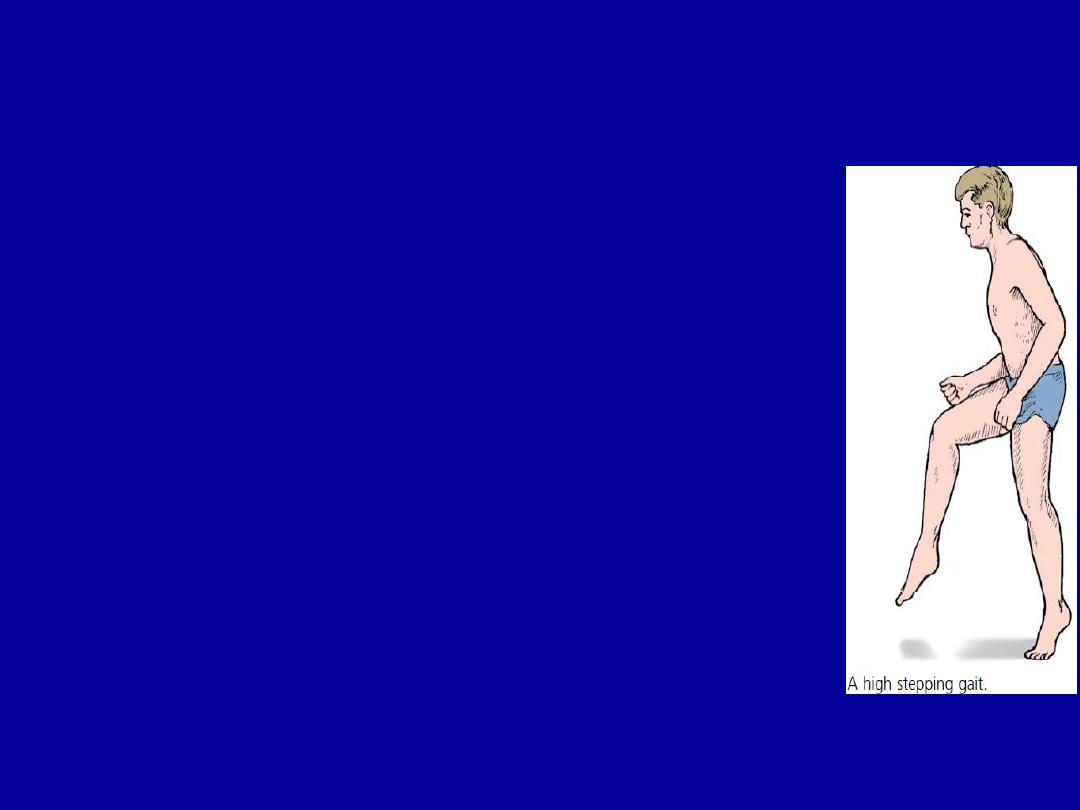
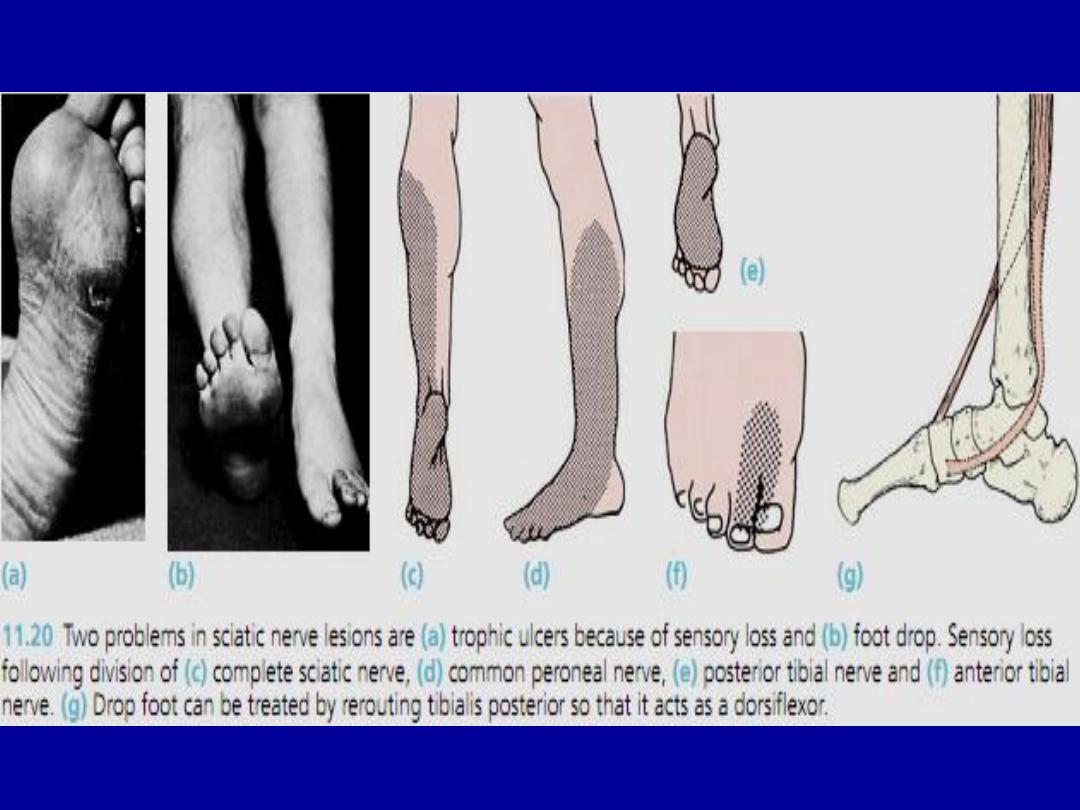
Sciatic Nerve
Injured by wounds, traction, hip dislocation, pelvic
.fractures, intraneural haemorrhage, iatrogenic.
Hamstrings and all muscles below the knee are
paralysed, ankle jerk is absent.
Sensation below the knee is lost except on the medial
aspect of the leg which is supplied by saphenous branch
of the F.N.
High stepping gait.
In late cases, wasting, fixed deformities, and trophic
ulcers.

TTT
Exploration
Repair,( suture, graft ).
Protection, physiotherapy, splint .
Tendon transfere(tibialis posterior to the front).
Foot stabilization
Amputation may be preferable to a flail, deformed, insensitive
limb.

The common peroneal nerve
Damaged at the level of the fibular neck by Sever
traction when the knee forced in to varus e.g :-
lateral ligament injuries
fracture around knee
during operative correction of gross valgus deformities
pressure from :
splint,
cast,
skin traction lying with leg externally rotated
intraneural ganglion).
Wounds.
Foot drop, a high stepping gait.
Sensory : anterior & lateral leg + dorsal foot

Tibial nerve injury
• Loss of plantar flexion
• Claw - toe deformity
• Causalgia is common
…………………………….
• ………………………………………………...
………………………………………………...