BRONCHIECTASIS
ا.د اسامه عبيد الخفاجيMBChB
FIBM Cardiothoracic & vascular surgey
MRCS Edn.
Bronchiectasis
is a persistent, general or local dilation of the bronchial wall, generally beyond the subsegmental levelPathology Three major patterns of dilatation are recognized macroscopically:
Cylindrical ,Saccular &Varicose
Site: the left lung is involved more often than the right
The left lower lobe was most frequently involved
Etiology:
A-CongenitalCongenital bronchial stenosis
Pulmonary sequestration
Immotile cilia syndrome (Kartagener's syndrome):
Bronchiomalasia
Cystic fibrosis
B-Acquired:
External bronchial compression: Usually by an enlarged LN.
MeaslesPertussis
TB
Internal bronchial occlusion
Inhaled foreign bodyTumor
Retained thick purulent secretions
Clinical presentation
1-A persistent productive cough of purulent sputum2-Hemoptysis
3-repeated chest infection
4- Pleuritic chest pain
5- Dyspnea
6-Associated symptoms include: fever, weight loss, anorexia and anemia.
Physical examination:
Cyanosis
Clubbing
coarse crepitations & wheezing
Dullness over the affected area
Investigations:
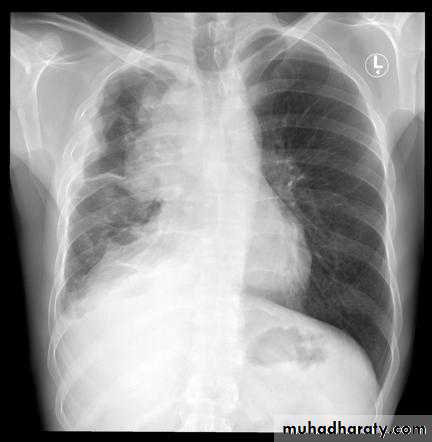
• 1-CXR :The plain chest radiograph is abnormal but generally nondiagnostic, the common findings are
• increased lung markings,
• atelectasis,
• air-fluid levels
• Cavities which fill and empty on serial CXR
• Honey-comb pattern: areas of destroyed lung with compensated overinflated adjacent parenchyma
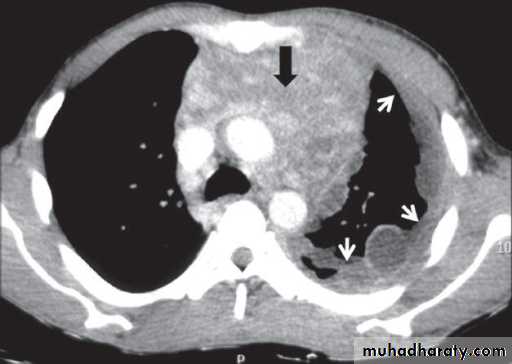
2-CT scan: is the imaging method of choice it shows Bronchial dilatation and wall thickening
• 3-Bronchoscopy : presence or absence of foreign body,
• bronchial stenosis or tumor
• bronchial wash for culture
• tracheobronchial toilet
• 4-PFT : restrictive pattern
• 5-Lung ventilation/perfusion scan: usually mismatch
Treatment:
A-Medical treatment
Prevention and control of infection: by prober usage of antibiotics
Mechanical removal of purulent secretions by:
Cough and chest physiotherapy
Postural drainage
Bronchoscopy
B- Surgical treatment
Indication:
1-Disease progress despite medical treatment
2-Recurrent episodes of chest infection
3-Frequent episodes of hemoptysis
The Mediastinum
It is the central cavity of the thorax bounded by:Thoracic inlet superiorly
Diaphragm Inferiorly
Sternum anteriorly
Vertebral column posteriorly
Pleural cavity laterally
Anatomy:
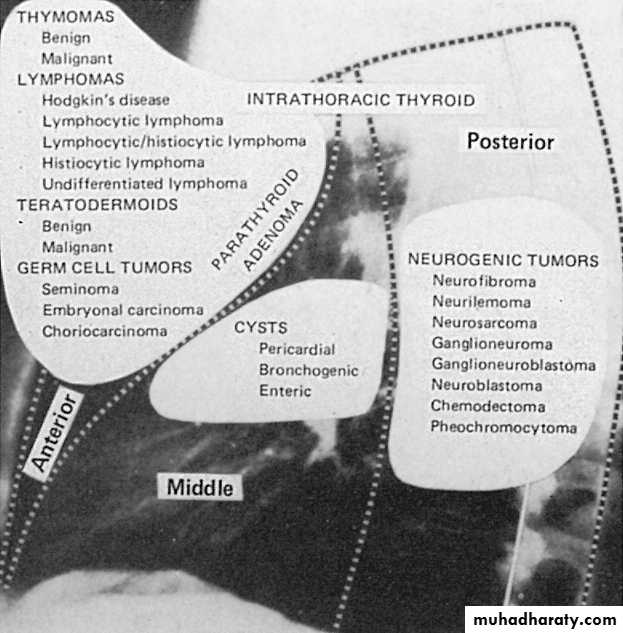
Clinically divided by imaginary lines into
Anterio-superior mediastinum:
It is anterior to the pericardium over the great vessels.
It contains:
The thymus gland
Aortic arch and branches
Great veins
Fatty areolar tissue
Middle mediastinum:
is bordered anteriorly by the anterior pericardial reflection and posteriorly by the posterior pericardial reflection.
The middle mediastinal contents include
the heart,
pericardium,
phrenic nerves,
tracheal bifurcation and main bronchi,
hila of each lung,
Posterior mediastinum:
bounded anteriorly by the pericardium and posterior pericardial reflection
The posterior mediastinum contains
the esophagus,
vagus nerves,
sympathetic nervous chain,
thoracic duct,
descending aorta,
azygous and hemiazygous systems,
paravertebral lymphatics,
Thymoma
Most common neoplasm of the antero-superior mediastinum and second most common mediastinal massPeak incidence 40-60 years of age
Pathology: Histologically classified into
1-Predominantly lymphocytic2-Predominantly epithelial
3-Mixed (most common 50%)
Staging : No TNM classification
Masaoka classification:Stage I: encapsulated tumor.
Stage II:
IIa : microscopic transcapsular invasion
IIb: macroscopical invasion into the thymus of fat or adherent to pleura or pericardium
Stage III: macroscopic invasion of neighboring organs e.g., pericardium, great vessels,lung.
Stage IV:
IVa: pleural or pericardial dissemination
IVb: lymphatogenous or hematogenous metastasis
Clinical presentation:
1- 1/3 of patients are asymptomatic
2-Local mass effect: cough, dyspnea, hemoptysis, SVC obstruction
3-Systemic syndromes (usually autoimmune):
A-Myasthenia
B-Aplastic anemia
C-Cushing's syndrome
D-Hypo and hypergammaglobulinemia
E-Hypercoagulopathy
F-Rheumatoid arthritis
Diagnosis:
Electromyography ( EMG )Tensilon test
Acetyle choline receptor antibody titer
Imaging including CXR, CT, MRI.
Tensilon test: transient increase in muscle strength after administration of short acting anticholinesterase such as edrophonium (tensilon)
EMG: abnormal loss of muscle contraction strength after multiple repetitive stimulation of the appropriate motor nerve → positive for MG
CXR & CT: it appears as a small well circumscribed mass or a bulky lobulated mass confluent with adjacent mediastinal structures
Treatment of thymoma:
Surgical resection is the therapy for thymoma whenever possible without removing or injuring vital structuresBest approach is through a median sternotomy
Treatment modalities:
Stage I → thymectomy alone
Stage II & III → thymectomy + radiotherapy
Stage IV → multiagent multimodularity therapy (surgery + radiotherapy + chemotherapy)
Recurrent disease → multiagent multimodularity therapy (surgery + radiotherapy + chemotherapy)
Postoperative care:
1-ICU2-ETT should be present and artificial ventilation continued probably for the first 24 hours.
3-Aggressive attention to pulmonary status:
Chest physiotherapy
Bronchodilators
Bronchoscopy + endobronchial suction
4-Early ambulation
THANKS