1
Paramyxoviruses
اﻟﻤﺮﺣﻠﮫ اﻟﺜﺎﻟﺜﮫ /ﻓﺎﯾﺮوﺳﺎت
د. اﻧﺘﻈﺎر ﻋﻼوي ﺟﻌﻔﺮ / ﻓﺮع اﻻﺣﯿﺎء اﻟﻤﺠﮭﺮﯾﮫ / ﻛﻠﯿﮫ اﻟﻄﺐ / ﺟﺎﻣﻌﮫ ذي ﻗﺎر
PhD. M.Sc. Microbiology
٩١٠٢-٢٠٢٠
Introduction
Introduction
Paramyxoviruses are roughly spherical-shaped viruses and usually vary in size
from 100 to 300 nm. These viruses consist of a negative-sense single-stranded
RNA genome enclosed in a helical nucleocapsid surrounded by a pleomorphic
envelope.
Classification
The family Paramyxoviridae consists of three important genera (Morbillivirus
,Paramyxovirus , and Pneumovirus ), which contain important human pathogens
responsible for causing most of acute respiratory infections and contagious
diseases of children and infants.
The genus
Morbillivirus
includes the measles virus.
The genus Paramyxovirus includes parainfluenza and mumps virus.
The genus Pneumovirus includes respiratory syncytial virus (RSV),
which is responsible for majority of acute respiratory infections in infants
and children
Diseases associated with some paramyxoviruses
Measles virus
Disease
Measles virus
Measles, atypical measles,
and subacute
sclerosing panencephalitis
Human paramyxovirus
HPIV-1,
and HPIV-3
HPIV-2,
Croup and pneumonia
HPIV-3, and HPIV-4
Bronchiolitis
and
tracheobronchitis
Mumps virus
Mumps
Respiratory syncytial virus
Upper
and
lower
respiratory tract infection,
common cold
Nipah virus
Encephalitis

2
Measles virus
Measles is a highly communicable acute viral disease characterized by fever,
conjunctivitis, and pathognomonic Koplik’s spots. It is one of the five classic
exanthematous diseases of the childhood; others being chickenpox, rubella and
roseola.
Morphology
Measles virus is spherical, but is often pleomorphic, measuring 120–250 nm in
diameter. It contains a negative-sense RNA genome. The helical nucleocapsid is
surrounded by an envelope carrying H and F proteins on its surface.
Viral replication
Measles virus replicates in the cell cytoplasm. The virus first adsorbs cell surface
by its hemagglutinin, then enters the cell, and uncoats inside the cytoplasm of
the cell. The viral RNA polymerase transcribes the negative-strand genome into
mRNA. Multiple copies of mRNAs are produced, each of which is translated into
specific viral proteins. This is followed by the assembly of nucleocapsid, and the
virus is released by budding from the cell membrane.
Antigenic and genomic properties
The measles virus has only one serotype and infects only humans, not any other
mammals. The virus is antigenically uniform.
Other Properties
The measles virus is heat labile. It is readily inactivated by ether,
formaldehyde, high temperature, and ultraviolet light.
The virus resists heating at 50°C for 1 hour.
Pathogenesis and Immunity
The virus initiates infection and replicates locally in the trachea and bronchial
epithelial cells of the respiratory tract. After 2–4 days, the virus spreads
systemically in lymphocytes, perhaps carried by pulmonary macrophages, and
causes viremia. Wide dissemination of the virus causes infection of the
conjunctiva, respiratory tract, urinary tract, lymphatic system, blood vessels, and
the central nervous system (CNS). The characteristic rash seen in measles is
caused primarily by cytotoxic T cells attacking the measles virus-infected
epithelial cells in the skin.
3
Key Points
Encephalitis is one of the most important sequelae of the infection caused by
measles. The virus causes:
Encephalitis by direct infection of the neurons;
Immune-mediated conditions, such as postinfectious measles
encephalopathy, believed to be immune mediated.
Clinical Syndromes
Incubation period varies from 8 to 12 days. Measles is a highly contagious febrile
illness. The prodromal phase is characterized by high fever, malaise, anorexia,
conjunctivitis, cough, and coryza. Koplik’s spot is the typical pathogenic lesion
found in the mucous membrane. These are bluish gray grain substance on a red
base, which usually appear on the buccal mucosa opposite the second molar. are
pathognomonic of measles. Their presence establishes the diagnosis of measles.
Clinical Syndromes
An erythematous maculopapular rash appears within 12–24 hours of
appearance of the Koplik’s spots. The rash usually begins on the face, then
spreads extensively and appears on the trunk, extremities, palms, and soles and
lasts for about 5 days.
Desquamation of the rashes except those of palms and soles may occur after 1
week.
Transmission of infection
Infected respiratory droplets are the primary source of infection. Patients are
infectious from 3 days before the onset of illness until the rash desquamates.
Infectivity is maximum at the prodrome and diminishes rapidly with the onset of
the rash. The infection is transmitted from person to person by inhalation of
large droplet aerosols produced during the act of coughing and sneezing.
Diagnosis
The clinical manifestations of typical measles cases are so characteristic that the
diagnosis is self-evident.
Prevention and Control
Measles vaccine along with mumps and rubella (MMR) vaccine is currently used
for universal immunization of children
Vaccines
Measles vaccine is a live attenuated vaccine,
The first dose of vaccine is given to children older than 12 months in the
United States, but are used for children aged 9 months in developing
countries with high endemicity.
The second dose of the vaccine is given usually to school going children
aged 4–6 years.
Mumps Virus
Mumps is an acute infectious disease of children, characterized by acute,
nonsuppurative, painful swelling of the salivary glands (parotid gland), caused
by mumps virus.
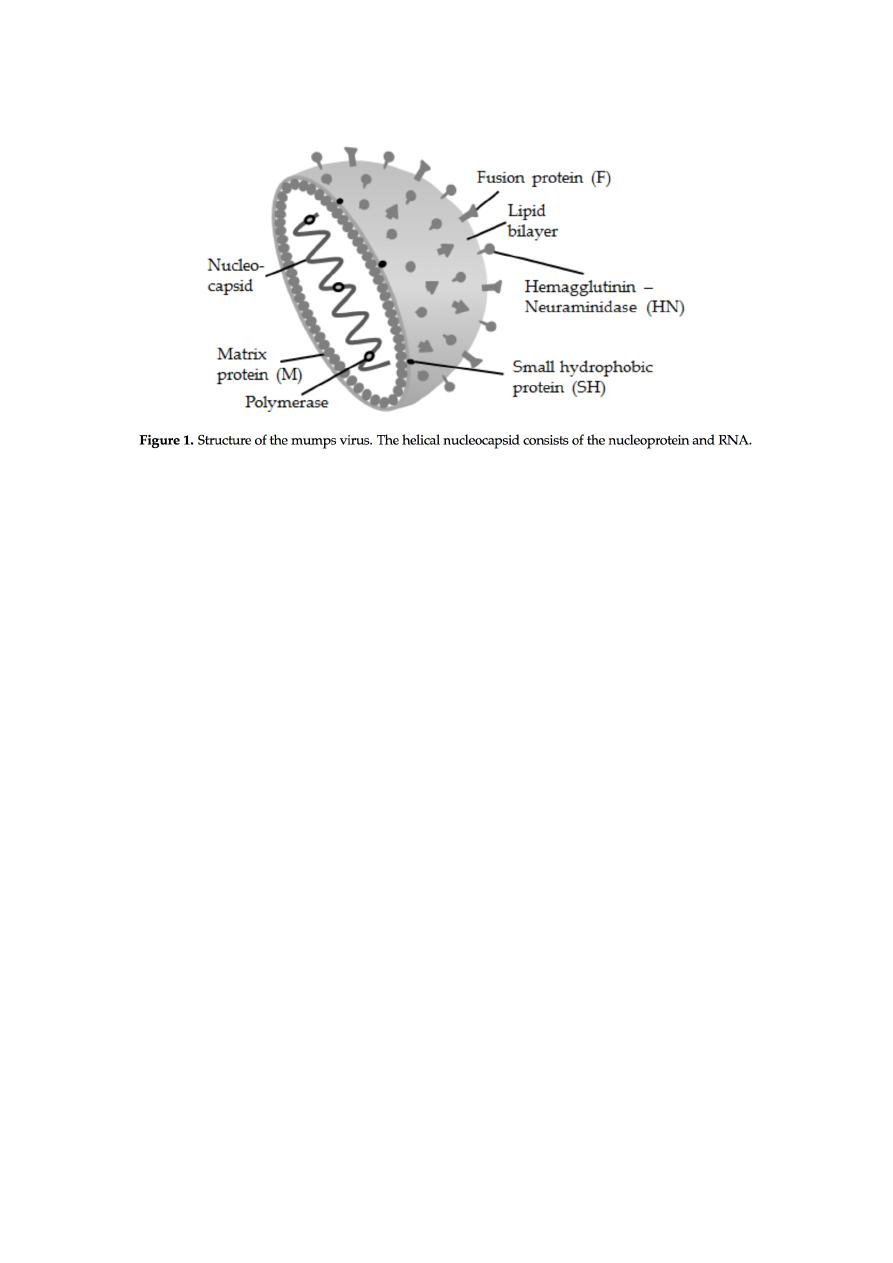
Morphology
Mumps virus is a typical paramyxovirus containing a single stranded, negative-
sense RNA surrounded by an envelope.
It has two major surface glycoproteins:
(a) One with both hemagglutinin and neuraminidase and
4
(b) The other with cell-fusion protein.The F protein is responsible for fusion of
lipid membrane of the virus to the host cell.
Antigenic and genomic properties
Only one antigenic type of mumps virus is known. Neutralizing antibodies are
produced against the hemagglutinin.
Other properties
The mumps virus is a heat-labile virus. It is sensitive to heat and rapidly
inactivated at room temperature.
Treatment with formaldehyde, ether, or ultraviolet light also inactivates the
virus. The virus can be stored for a longer period by lyophilization at 70°C.
Virus Isolation
Cell culture: The virus grows well in tissue culture, Hep-2 cells. The CPE
consists of multinucleated giant cells and acidophilic cytoplasmic
inclusions. The growth of virus in the cells can be detected by direct
immunofluorescence and hemadsorption. The virus also grows well in
amniotic cavity of 6–8 days’ old embryonated egg.
Pathogenesis of mumps
Infection by mumps virus begins after the entry of the virus into the respiratory
tract. The virus then replicates locally and disseminates by blood circulation to
target tissues, such as the CNS and salivary glands, particularly the parotid
glands by viremia. Salivary glands, such as parotid glands, show desquamation of
necrotic epithelial cells lining the ducts. The virus replicates in these target
tissues and then causes a secondary phase of viremia. The virus is spread by
viremia throughout the body.
Clinical Syndrome
The incubation period is long and varies from 12 to 25 days. Most of the
infections are asymptomatic. The onset of mumps is sudden.
Fever, headache, and earache are the initial symptoms. These symptoms are
followed by painful swelling of the parotid gland. Initially, it may be unilateral
but may become bilateral later. The condition is accompanied by fever, local
pain, and tenderness.
5
Epididymo-orchitis is the second most common manifestation in adults,
which is usually preceded by parotitis. Orchitis may occasionally cause
testicular atrophy and sterility.
Complications of mumps: Meningoencephalitis is the most frequent
complication of mumps in childhood.
Transmission of infection
The infected patients are the source of infection. A patient remains
infectious usually from 9 days prior to the onset of parotid swelling as
long as 7 days after onset of the swelling.
The infection is transmitted by direct person-to-person contact and also
by inhalation of respiratory droplets. The unvaccinated people and
immunocompromised people are at more risk to infection by mumps
virus.
Laboratory Diagnosis
Diagnosis of mumps is usually clinical. The laboratory diagnosis is useful for
diagnosis of atypical infection or manifestation of mumps without typical
symptoms.
Host immunity
Humoral immunity is characterized by the appearance of antibody against the
soluble S antigen and hemagglutinating antibodies. The antibody against S
antigen is the first to appear, within 3–7 days after the onset of symptoms. The
hemagglutinating antibodies directed against hemagglutinin confer lifelong
immunity against mumps virus. CMI is essential for control of infection. This also
contributes to pathogenesis of the disease and is responsible partially for the
symptoms observed during the course of clinical illness.
Parainfluenza Virus
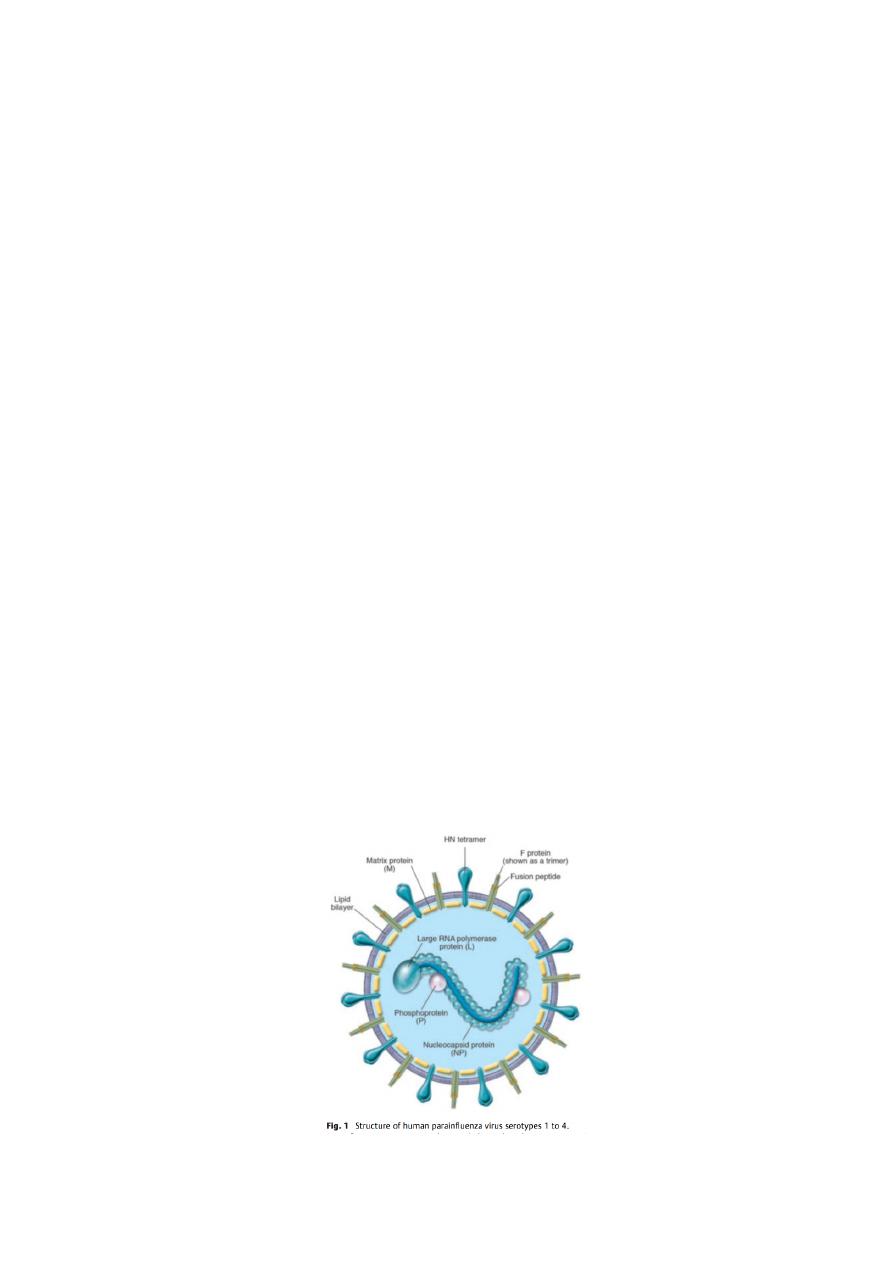
Parainfluenza viruses are pleomorphic viruses measuring 150–200 nm in
diameter.
The virus contains a single-stranded, nonsegmented, negative-sense RNA
genome with nucleoproteins P and L. It is surrounded by a helical
nucleocapsid, which contains glycoprotein spikes.
The surface spikes consist of H, N (neuraminidase), and F proteins. Both
H and N proteins are present on the same spike, whereas the F protein is
present on a separate spike. The F protein mediates the formation of
multinucleated giant cell.

6
Pathogenesis of human parainfluenza viruse infection
The virus adsorbs to the respiratory epithelial cells by specifically combining
with neuraminic acid receptors in the cell through its hemagglutinin.
Subsequently, the virus enters the cells following fusion with the cell
membrane, mediated by F1 and F2 receptors. The virus replicates rapidly in
the cell cytoplasm and causes formation of multinucleated giant cells. The
virus also causes the formation of single and multilocular cytoplasmic
vacuoles and basophilic or eosinophilic inclusions.
The virus causes inflammation of the respiratory tract, leading to secretions
of high level of inflammatory cytokines, usually 7–10 days after initial
exposure. Airways inflammation, necrosis, and sloughing of respiratory
epithelium, edema, and excessive mucus production are the noted
pathological features associated with HPIV infections.
Clinical Syndromes
Human parainfluenza viruses cause croup (a heterogeneous group of illnesses
that affects the larynx, trachea, and bronchi. The condition manifests as fever,
cough, laryngeal obstruction), pneumonia, bronchiolitis and tracheobronchitis,
and Otitis media, pharyngitis, conjunctivitis.
Reservoir, source, and transmission of infection
Parainfluenza viruses cause disease exclusively in humans. No animal reservoirs
are present. Respiratory secretions from the infected humans are the source of
infection. The infection is transmitted by inhalation of respiratory droplets or by
direct person-to-person contact with infected secretions.
Laboratory Diagnosis
u
Respiratory specimens include nasopharyngeal aspirations nasal
washings, and nasal aspirations
1- Direct antigen detection : The ELISA, immunofluorescence assay are
used to detect HPIV antigen.
2- Molecular Diagnosis: A multiplex reverse transcriptase polymerase
chain reaction (RT-PCR) has been developed for simultaneous
detection of HPIV-1, HPIV-2, and HPIV-3 genome in clinical specimens.
Prevention and Control
Currently there is no vaccine against infection by HPIV, However, researchers
are trying to develop one.
•
The risk of HPIV and other respiratory viral infections could be reduced
by:
•
washing your hands often with soap and water for at least 20 seconds.
•
avoiding touching your eyes, nose, or mouth.
•
avoiding close contact with people who are sick.
