Vulval cancers
Vulval cancer is uncommon, with an incidence of ten cases per 100 000
women .These are skin tumours of the vulva and are divided into HPV
associated (usually younger patients) and non-HPV (usually older
patients) cancers. The latter group may have their cancer associated with
VIN and lichen sclerosis,melanoma, pagets disease,smoking ,
immunosuppression.
Clinical presentation
Vulval cancers usually present with vulval symptoms. Patients may
present with a lump
(noticed when washing
), vulval pain (some tumours are
ulcerating) and post-menopausal bleeding (some tumours bleed
on touch). Some patients are frequently unaware of vulval cancer.
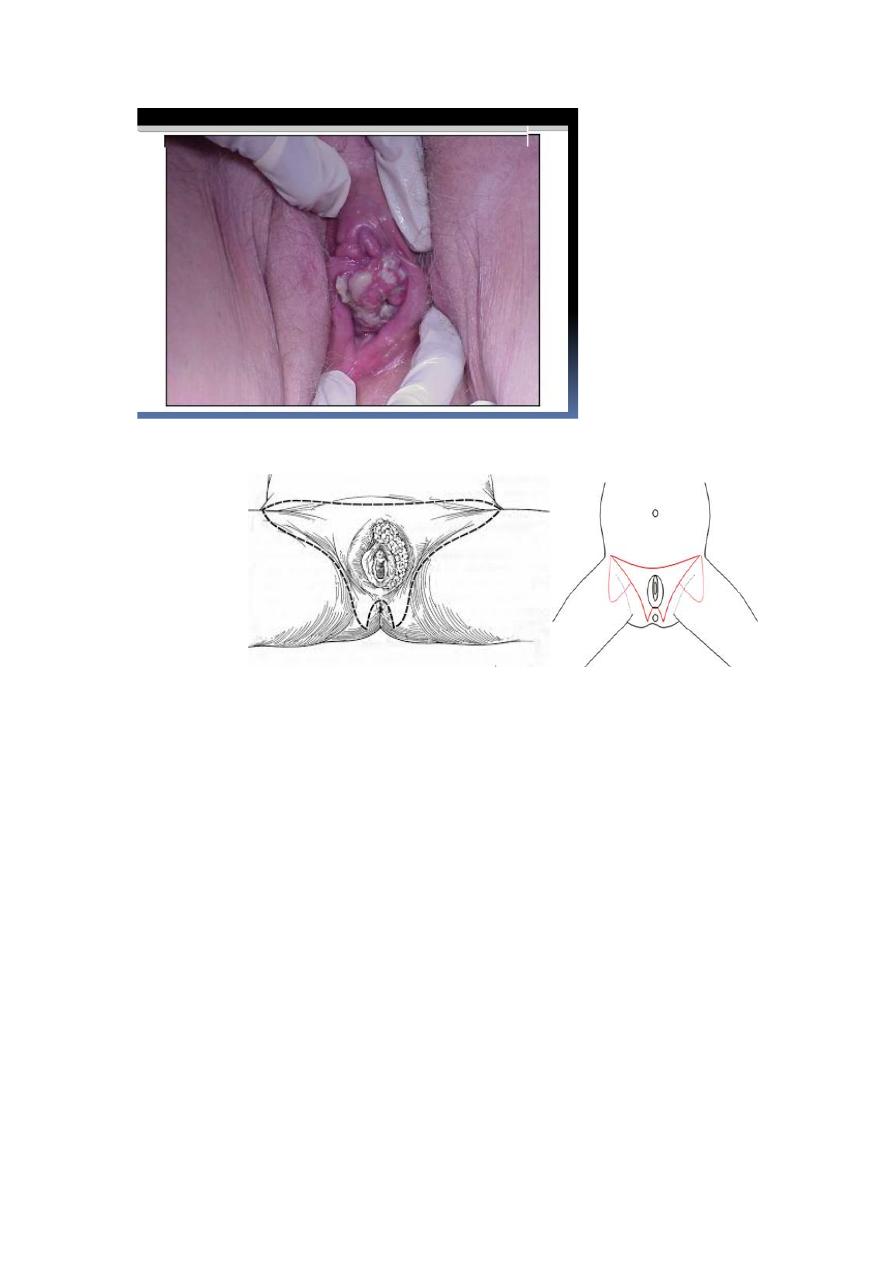
The tumours are usually clinically obvious and are often cauliflower-type
growths on the vulva.
The most common sites are the labia majora and clitoris and the tumours
may be uni- or multifocal so it is important to examine the patient
thoroughly (include the anal area, vagina and cervix). Vulval cancer
spreads regionally to the groin nodes (inguinal and femoral) and palpation
of these nodes is important to exclude clinically obvious malignant nodes.
Patients should also have the cervix inspected to make sure that there is
no involvement by cancer or cervical intraepithelial neoplasia (CIN).
Pathophysiology
Most vulval cancers are squamous cell cancers of the skin. The lymphatic
drainage of the vulva (and the lower third of the vagina) is to the inguinal
and femoral lymph nodes and this is the first place to which the tumour
metastasizes. Beyond this, the tumour can spread up the lymphatic chain
and finally to the liver and lungs at a late stage.
Investigations:
A full-thickness biopsy should be taken from the tumour and should
include the interface between the apparent normal surrounding tissue and
the cancer. biopsy is essential for diagnosisThe cervix should be
visualized to exclude a cervical cancer, which may occasionally coexist..

chest x-ray is useful to exclude obvious lung metastases. a computed
tomography (CT) or magnetic resonance (MR) assessment of the pelvis
should be undertaken to exclude obvious pelvic lymphadenopathy.
Poor prognostic factors include:
large (greater than 4 cm) primary tumours, sphincter involvement and
metastases to the groin nodes.
Staging of vulval cancer
:
Stage Description 5-year survival
1 1a: Confined to vulva and/or perineum, 2 cm or less maximum
diameter. Groin nodes not palpable. Stromal invasion no greater than 1
mm
1b: As for 1a but stromal invasion >1 mm
2
Confined to vulva and/or perineum, more than 2 cm maximum
diameter. Groin nodes not palpable
3
Extends beyond the vulva, vagina, lower urethra or anus; or unilateral
regional lymph node metastasis
4
4a: Involves the mucosa of rectum or bladder upper urethra; or pelvic
bone; and/or bilateral regional lymph node metastases
4b: Any distant metastasis including pelvic lymph nodes
Treatment
Two broad categories of patient can be identified at the outset:
• Those who have small unifocal vulvar lesions with no clinical evidence
of nodal involvement.
• Those who have more advanced vulvar disease and or have clinical
evidence of nodal involvement.
For the purposes of further discussion, these will be termed as early and
late disease, respectively.
Surgical management of early vulvar cancer
Wide local excision is usually sufficient for the majority of lesions
between 1 and 10 mm in depth. Surgical excision should therefore be at
least 15 mm on all the tumour dimensions. In situations where for
example in early but midline cancers(clitoris, urethra, anus), radiotherapy
may have a role in allowing local control without loss of function
Surgical management of advanced vulvar lesions

advanced vulvar lesions indicates that wide local excision would either
be a radical vulvectomy and/or would compromise function.
The prime objective is to maximize local control, closely followed by
consideration of further function and cosmesis in that particular woman.
Management of lymph node:
In small ( < 2 cm) lateral tumours, only an ipsilateral groin node
dissection need initially be performed.
A lateralized lesion, is defined as one in which wide excision, at least 1
cm beyond the visible tumour edge, would not impinge upon a midline
structure
If the ipsilateral nodes are subsequently shown to be positive for cancer,
the contralateral nodes should also be excised or irradiated as the nodes
are more likely to be positive in this scenario.
For larger lateralized bilateral node dissection would be advisable.
En bloc and separate groin incisions
The need for en bloc removal of the lymph nodes has received
much attention, largely because it has been felt that this type of
procedure accounts for a significant pro portion of the morbidity
and that the technique employing separate groin incisions results
in a better cosmetic outcome.
The anxiety relating to the triple incision is the possibility of
relapse in the bridge of tissue left between the vulvectomy or local
excision and the groin nodes. Certainly if the lymphatic channels
contain malignant cells at the time of resection, then recurrence
would seem to be a real possibility. Current consensus would
suggest that en bloc dissection of the nodes is probably best
retained for large vulvar lesions and in situations where there is
gross involvement of the groin nodes-
Complications of surgery
.
1. Groin dissection
• Wound breakdown/cellulitis
• Lymphocyst
• Lymphoedema
2. Vulvar resection

• Wound breakdown/cellulitis
• Rectocoele
• Urinary problems
• Psychological
Patients with lymphoedema describe a heavy, ‘wooden’, sometimes
painful feeling in the legs as a result of retention of lymph fluid. This can
cause reduced mobility and problems wearing shoes. Management
involves leg elevation, good skin care, massage of the limbs and, in
severe cases, support stockings.
The sentinel lymph node (SLN) procedure:
may replace groin node dissection in the future where the SLN (the first
lymph node to be involved with metastases) is identified and removed in
isolation. If this node is negative, the patient is followed up and if
positive, radiotherapy is given.
Advanced disease (stages 3 and 4) is difficult as patients often die from
disease. Patients are treated with combinations of surgery (to remove
malignant nodes), radiotherapy and chemotherapy. This is as difficult
treatment as patients are often elderly and radiotherapy to the vulval skin
frequently produces pain through skin desquamation. Palliative care input
therefore is important at an early stage.