1
Dermatology Dr. Hussein A. Al-Sultany
2019-2020
Viral Skin Infections
Herpesviruses
Herpesviruses belong to Herpesviridae which is a large family of DNA viruses.
There are eight distinct viruses in this family known to cause diseases in humans (human
herpes viruses (HHV)), include:
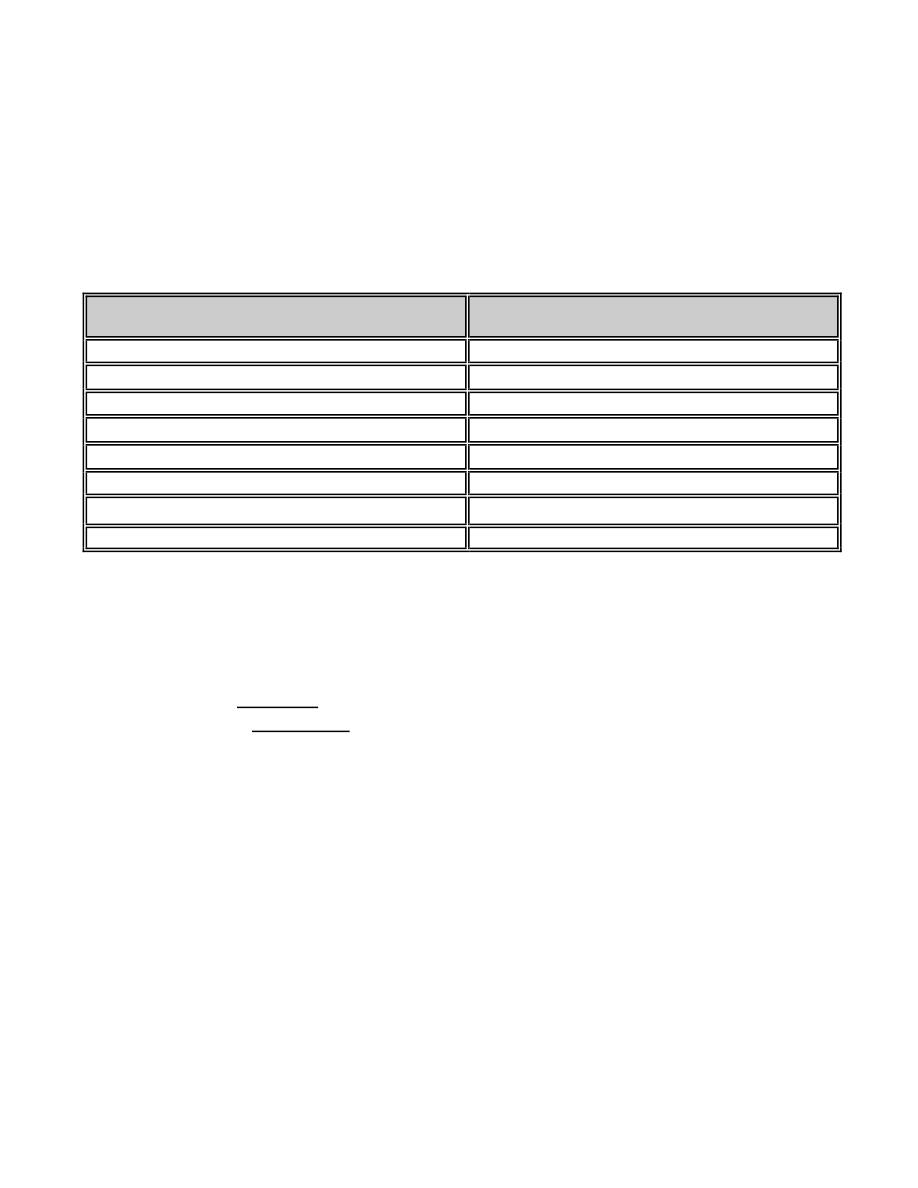
Virus type
Diseases
HHV-1 (HSV-1)
Herpes Labialis.
HHV-2 (HSV-2)
Herpes Genitalis.
HHV-3 (VZV)
Chickenpox and Herpes Zoster (HZ).
HHV-4 (EBV)
Infectious Mononucleosis.
HHV-5 (CMV)
Infectious Mononucleosis-like syndrome.
HHV-6
Roseola Infantum.
HHV-7
Pityriasis Rosea.
HHV-8
Kaposi's Sarcoma.
Herpes Simplex Virus (HSV):
It has been separated into two types:
Type 1: are usually orofacial (herpes labialis).
Type 2: are usually genital (herpes genitalis).
The virus usually spread by direct contact.
Herpes viruses are not curable, after the episode of the primary infection, the virus may
become latent, possibly within nerve ganglia, but still capable of giving rise to recurrent
bouts of vesication (recurrences or recrudescences).
1- Primary infection:
A- Herpes labialis: the most common recognizable manifestation in children is an acute
gingivostomatitis, accompanied by malaise, headache, fever and cervical
lymphoadenopathy. Vesicles, soon turning into small ulcers, can be seen scattered over
the lips and mucous membranes. The illness lasts about 2 weeks.
B- Herpes genitalis: usually transmitted sexually, cause multiple and painful genital or
perianal vesicles which rapidly ulcerate.
2- Recurrent (recrudescent) infection:
The lesions usually recur at the same place.
A- Herpes labialis: usually on the lips and the vermilion border.
B- Herpes genitalis: usually on the genitalia.
2
Triggering factors:
A- Herpes labialis: fever, URTI (cold sores), ultraviolet radiation, menstruation, or stress.
B-
Herpes genitalis: physical stress, emotional stress, steroids, menstruation,
imunossupression, and friction from sexual activity or tight clothes
Clinical features: tingling, burning or even pain is followed within a few hours by the
development of erythema and clusters of tense vesicles (grouping arrangement).
Crustation occurs within 24–48 h and the whole episode lasts about 2 weeks.
● Vesicles in recurrent infections differ from those in primary infections by: (1) smaller
size. (2) fewer number. (3) closer grouping. (4) the usual absence of constitutional
symptoms or lymphadenopathy, unless there is secondary bacterial infection.
Complications:
1- Herpes encephalitis or meningitis.
2- Disseminated herpes simplex.
3- Eczema herpeticum: widespread infections, usually occur in atopic dermatitis.
4- Secondary bacterial infection.
5- Recurrent dendritic ulcers leading to corneal scarring.
6- Erythema multiforme.
Treatment:
Topical:
Acyclovir cream or penciclovir cream, applied frequently, started as early as possible for
few days.
Topical antiseptic, sunscreens, lubricating creams may also be required.
Systemic:
Acyclovir is an antiviral drug that acts as a specific inhibitor of herpesvirus DNA
polymerase. Famciclovir and valaciclovir can be used.
1- Primary infection:
acyclovir tablets 200 mg five times daily for 7-10 days.
2- Recurrent infection:
A- Episodic treatment: if less than 6 recurrences per year.
Acyclovir tablets 400 mg three times daily for 5 days.
B- Suppressive therapy: if more than 6 recurrences per year.
Acyclovir tablets 400 mg twice daily, for prolonged periods (6 months).
3- Sever disease or immunocompromised patient :
IV acyclovir 5-10 mg/kg three times daily for 7-10 days.
Varicella-Zoster Virus (VZV):
Varicella (Chickenpox):
It is the primary infection of VZV, it is a highly contagious viral infections, transmission
occur via airborne droplets or contact with the vesicular fluid. Patients are contagious 2
days before and 5 days after onset of rash. The IP averages 2 weeks.
Presentation and course:
Prodromal symptoms (fever, chills, malaise, headache, and anorexia) are followed by the
development of papules, which turn rapidly into clear vesicles, which may become
pustules, over the next few days the lesions crust and then clear, sometimes leaving
depressed scars.
3
Lesions appear in crops, so lesions of different stages are present at the same time.
The
lesions are often itchy, and are most profuse on the trunk (centripetal). The vesicles may
also develop in the mucous membranes (especialy of the mouth).
An attack of chickenpox usually confers lifelong immunity.
Complications
1- Secondary bacterial infection.
2- Primary varicella pneumonia (mostly in adult patients).
3- Bacterial pneumonia, otitis media, and suppurative meningitis.
4- Haemorrhagic or lethal chickenpox in the immunocompromised.
5- Scarring.
Treatment:
1- Symptomatic relief : antipruritic lotions (e.g. calamine), antipyretics (except aspirin),
and antihistamines.
2- Antibiotics: indicated for secondary bacterial infections.
3- Systemic antiviral (acyclovir 20 mg /kg, 5 times daily for 7 days), indicated for:
A- Severe attacks.
B- Immunocompromised.
C- Patients 13 years of age or older (more sever & more complicated disease).
● Varicella vaccine (Varivax, Varilrix) is a live (attenuated) virus administered to protect
against chickenpox. It was recommended in 2006 as a part of the routine immunization
schedule in the US, not all countries provide the vaccine due to its cost.
Herpes Zoster (HZ) (Shingles):
HZ is caused by VZV. An attack is a result of the reactivation of virus that has remained
dormant in a sensory root ganglion since an earlier episode of chickenpox.
The incidence of shingles is highest in old age, and in some conditions in which weaken
normal defense mechanisms.
Patients with zoster can transmit the virus to others in whom it may cause chickenpox
(if there is no previous attack).
Presentation and course:
Attacks usually start with a burning pain, soon followed by erythema and grouped
vesicles (grouping arrangement), scattered over a dermatome (dermatomal distribution);
commonly the thoracic segments or the ophthalmic division of the trigeminal nerve.
It may affect more than one adjacent dermatome.
The clear vesicles quickly become purulent, and over a few days burst and crust.
Hemorrhagic or necrotic lesions may indicate an underlying immunodeficiency state.
● HZ is characteristically unilateral, and usually occurs once in life.
● Second episode, or bilateral infection of HZ is very unusual.
● Occasionally, before the rash has appeared, the initial pain is misdiagnosed as acute
appendicitis, renal colic, or myocardial infarction (according to its site).
Complications:
1- Post herpetic neuralgia: the most common complication, which is a persistent neuralgic
pain after the skin lesions have disappeared. Its risk increase with age and severity.
2- Dissimination: may occur in immunocompromised patients, devided into:
a- Cutaneous (more than 20 vesicles outside the affected dermatome).
b- Visceral (lung, liver, and brain involvement).
3- Motor nerve involvement, which has led to muscular paralysis.
4
4- Secondary bacterial infection.
5- Necrosis and scarring.
6- HZ ophthalmicus (HZ of the ophthalmic division of the trigeminal nerve): can lead to
corneal ulcers and scarring.
7- Ramsay-Hunt’s syndrom: involvement of the geniculate ganglion, can lead to facial
nerve paralysis and auditory symptoms.
Treatment:
1- Systemic antiviral therapy: acyclovir 800 mg five times daily for 5-7 days, should be
given in the early stages of the disease (within the first 3 days).
Indications: (a) old patient (more than 50 years). (b) very painful or sever case.
(c) immunosuppressed patient. (d) dissimination. (e) motor nerve involvement.
(f) HZ ophthalmicus. (g) Ramsay-Hunt’s syndrom.
Topical antiviral agents is not effective in HZ.
2- Supportive therapy: rest, analgesics and antipruritic lotions as calamine.
3- Antibiotic therapy: for secondary bacterial infection.
4- Treatment of post-herpetic neuralgia: gabapentin, carbamazepine, amitriptyline, or
topical capsaicin cream.
Human Papilloma Virus (HPV)
HPV is a DNA virus, with more than 100 recognizable serotypes.
HPV infect the skin causing warts, which transmitted by direct contact.
Types of warts:
Many types of wart have been identified, varying in shape and site affected, as well as the
serotype of human papillomavirus, these include:
1- Common wart (Verruca vulgaris): aised with rough surface, most common on hands.
2- Flat wart (Verruca plana): a small, smooth, flattened, skin-coloured or light brown.
Lesions are multiple, painless and mostly on a face of children.
3- Genital wart (Condyloma acuminata): papillomatous cauliflower-like lesions, with a
moist macerated surface on the genitalia.
4- Filiform or Digitate wart: a thread- or finger-like wart, most common on the face.
5- Plantar wart: these have a rough surface, which protrudes slightly from the skin.
6- Periungual wart: warts that occurs around the nails.
7- Mosaic wart: a group of tightly clustered warts, commonly on the soles.
Course:
● Warts commonly occur in children and young adults, but they may appear at any age.
● Their course is highly variable; most resolve spontaneously in months, and others may
last years or a lifetime. Such spontaneous resolution, sometimes heralded by a punctate
blackening (black dots) caused by capillary thrombosis.
● Mosaic warts are slow to resolve and often resist all treatments.
●
Warts persist and spread in immunocompromised patients (especially with
lymphoreticular disease).
●
Warts may spread by autoinoculation, scratching (koebner phenomenon).
Complications:
1- Pain: some plantar warts are very painful.
2- Secondary bacterial infection.
5
3- Malignant change: generally it is rare, but may occur in the following conditions:
A- Certain genital strains (16&18), predispose to cervical or penile carcinoma (SCC).
B- In immunocompromised patients (as renal transplantation),especially on exposed areas.
C-
Epidermodysplasia verruciformis: a rare inherited disorder, in which there is a
impairment of cell-mediated immunity with universal wart infection.
Treatment of warts:
1-Topical: caustic material (salicylic acid, lactic acid, or TCA), imiquimode,
podophylline, or 5-Flourouracil.
2- Intralesional: 2% zinc sulphate, or interferon alfa.
3- Physical: curettage &/or electrodesication, cryotherapy, CO2 laser, or excision.
4- Systemic: oral zinc sulphate, cimetidine, retinoids, interferon, or BCG vaccination.
5- Others, include:
A- Antiviral therapy: recently cidofovir (Vestide) treatment is promising, it can be used
systemically(IV) or topically, or by intralesional injection, it is very expensive.
B-
Treatment by suggestion:
Many myths and some studies claiming that warts can be
effectively treated by suggestion.
Vaccination: prophylactic vaccination to prevent (not treat) genital wart (6,11,16&18)
.
Two types available:
(1) Cervarix
. (
2) Gardasil
.
Poxvirus
The poxviruses are double-stranded DNA viruses. They are the largest animal viruses and
can be seen with light microscopy. It have 3 main genuses: orthopox causing smallpox
which is eradicated since 1978, molluscipox causing MC, and parapox causing orf.
Molluscum Contagiosum (MC):
Presentation and course:
The incubation period ranges from 2 to 6 weeks. Individual lesions are shiny, pearly or
pink in color, smooth surface, firm, dome shaped papule, averaging 3-5 mm. A central
punctum, which may contain a cheesy core, gives the lesions their characteristic
umbilicated look. The most commonly involved sites are the face and the genital areas.
Multiple lesions are common, and often several members of one family are affected. They
may spread by autoinoculation, scratching (koebner phenomenon), or touching a
contaminated fomites. Untreated lesions usually clear in 6–9 months.
Treatment
● Treatment options: curettage, cauterization, cryosurgery, cantharidin, imiquimod,
tretinoin, chemical solutions (phenol, lactic acid, TCA, or KOH), or CO2 laser.
●
The antiviral agent cidofovir has recently been shown to effectively resolve molluscum
lesions (used either intravenously or topically).
Orf:
Presentation and course:
The incubation period is 5 to 6 days. Lesions are pustular nodules with a violaceous or
erythematous surround. It can be transmitted to those handling infected animals (especially
the animal's head). The condition clears up spontaneously in about a month.
Treatment: A topical antibiotic helps to prevent secondary infection; otherwise no active
therapy is needed.
