Pelvic endoscopy
•
Laparoscopy
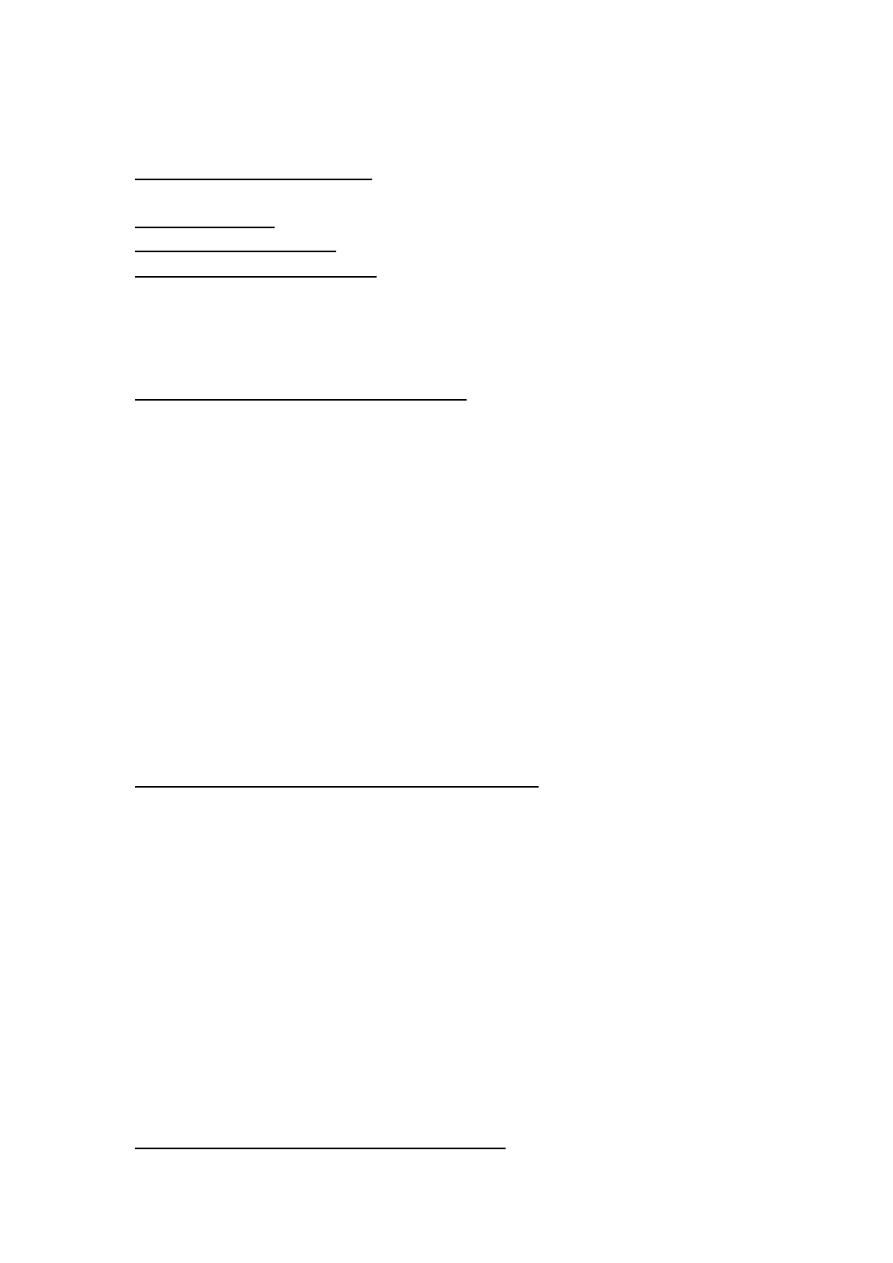
Laparoscope is an instrument for viewing the peritoneal cavity.
v
Benefits of laparoscopy
1. Decreased postoperative pain.
2. Earlier return to normal activities following surgery.
3. Fewer postoperative complications such as wound infection and
hernia, compared with open techniques.
4. Small scars.
v
Indications of laparoscopy
1. Tubal sterilization.
2. Acute or chronic pelvic pain.
3. Ectopic pregnancy.
4. PID.
5. Endometriosis.
6. Adnexal torsion.
7. Sub fertility.
8. Congenital pelvic abnormality.
9. Abnormal pelvic ultrasound.
10. Unexplained pelvic mass.
11. Staging for ovarian malignancy.
12. Hysterectomy and myomectomy
13. Urogynelogical procedures
v
Contraindications for laparoscopy
1. Mechanical or paralytic bowel obstruction.
2. Generalized peritonitis.
3. Diaphragmatic hernia.
4. Major Intraperitoneal hemorrhage (shock).
5. Severe cardio respiratory disease.
6. Massive obesity.
7. Inflammatory bowel disease.
8. Large abdominal mass.
9. Advanced pregnancy.
10. Multiple abdominal incisions.
11. Irreducible external hernia.

v
Complications of laparoscopic surgery
It is estimated that up to 50% of laparoscopic complications are entry-
related, and most injury-related litigations are trocar-related.
A. Intra-operative
1. Bowel injury.
2. Vascular injury.
3. Bladder injury.
4. Ureteric injury.
5. Surgical emphysema.
6. Anesthetic complication.
B. Post-operative
1. Unrecognized visceral or vascular injury.
2. VTE.
3. Infection.
4. Port site hernia.
5. Entry –related complications of laparoscopy
6. Laparoscopic injuries frequently occur during the blind insertion
of Veress needles, trocars and cannulae through the abdominal
wall.
7. Co
2
gas embolism
v
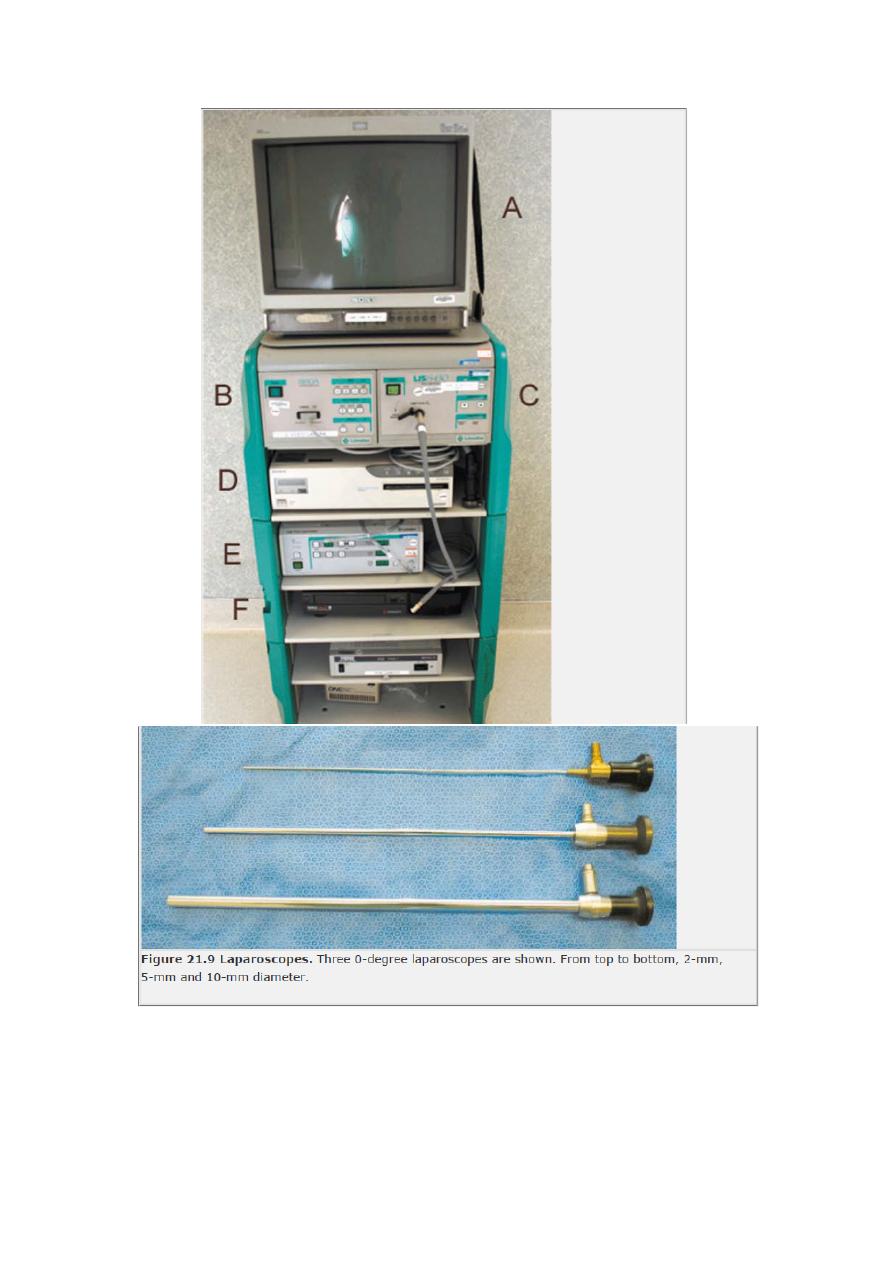
Technique
The procedure is performed with the patient in a modified dorsal
lithotomy position(with knee crutches) usually under general anasthesia.
an intrauterine manipulator is inserted to help in visualization of pelvic
organs. A pneumoperitonium is created by inserting a Veress needle in to
the peritoneum cavity through a subumbilical fold and insufflations with
either CO2 or nitrous oxide.
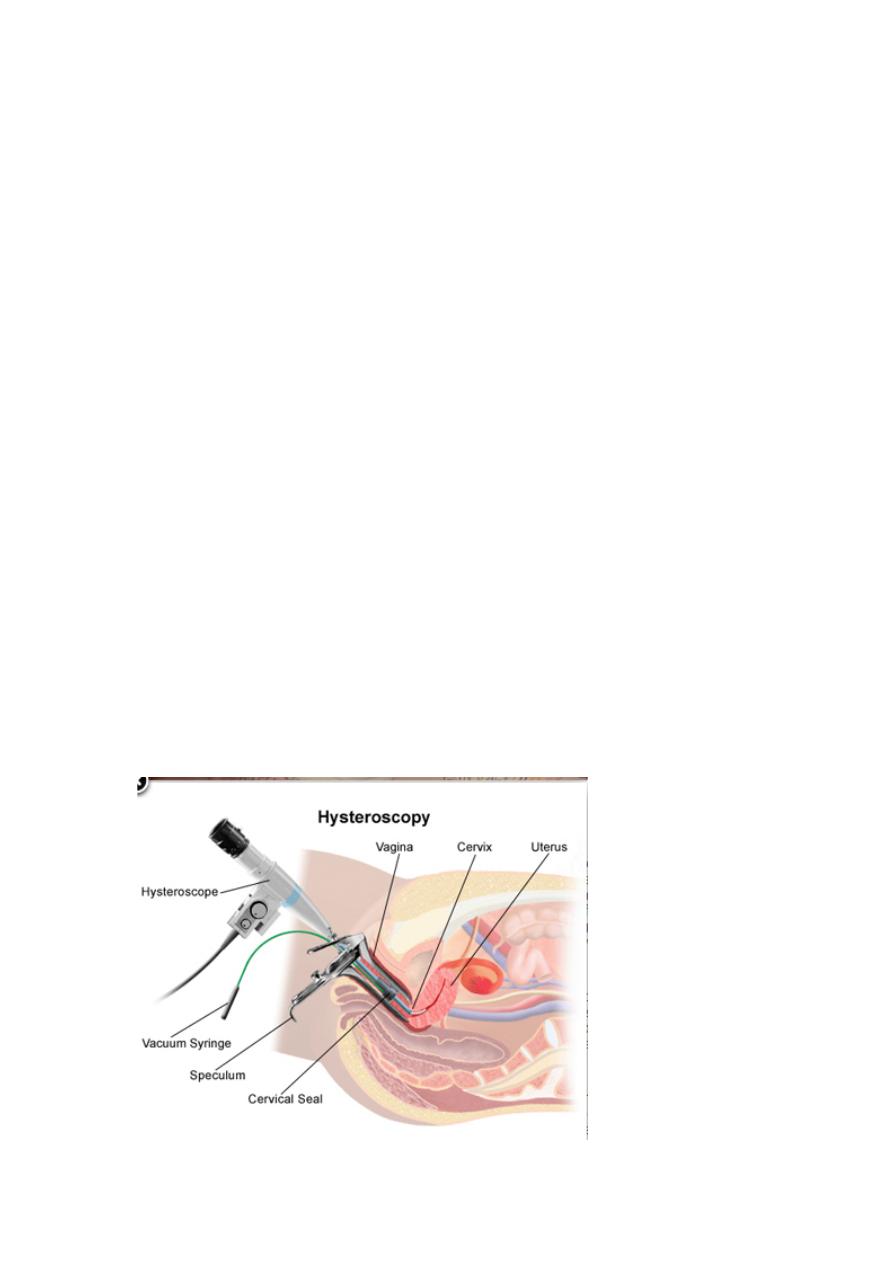
• Hysteroscopy
v
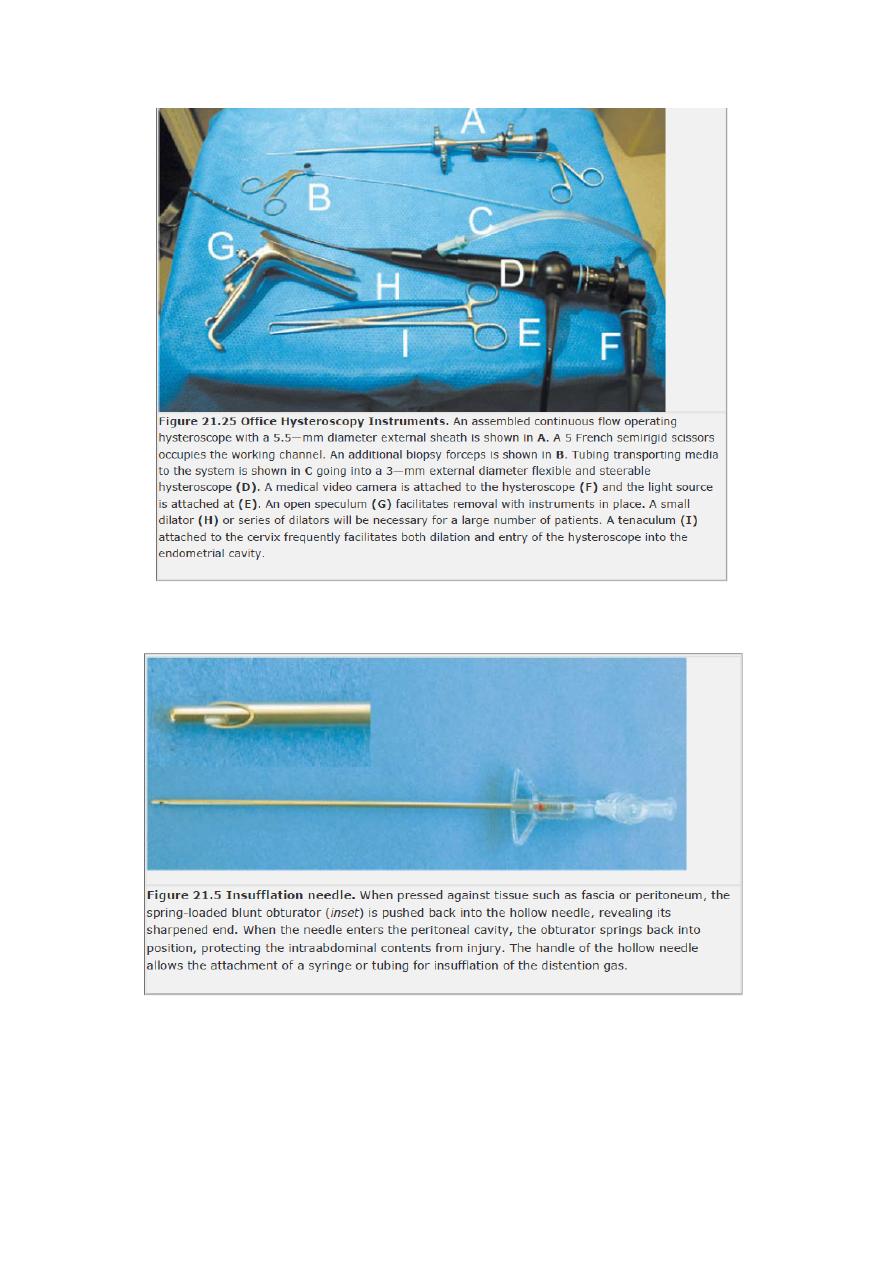
Equipment for hysteroscopy
1. Hysteroscope: both rigid &flexible.
2. Uterine distension:
a. gas (CO2).
b. Low-viscosity fluids: normal saline, 5% dextrose,
1.5%glycine, 3% sorbitol, 5%manitol.
c. high viscosity fluid: e.g hyskon.once absorbed, causes
haemolysis.
3. Mechanical instruments: such as scissors, grasping and biopsy
forceps and monopolar electrodes.
4. Resectoscope
5. Laser hysteroscopy:
6. Intrauterine morcellator
v
Diagnostic hysteroscopy
Indications of diagnostic hysteroscopy
1. Abnormal menstruation age ˃40 years.
2. Abnormal menstruation not responsive to medical treatment (age
<40y)
3. Intermenstrual bleeding despite normal cervical smear.
4. Post-coital bleeding despite normal cervical smear.
5. Postmenopausal bleeding (persistent or endometrial thickness ≥4
mm.
6. Abnormal pelvic ultrasound findings (e.g endometrial polyps, sub
mucousfibroids).
7. Subfertiliy.
8. Recurrent miscarriage.
9. Sherman’s syndrome.
10. Congenital uterine anomaly.
11. Lost IUCD.
Contraindications of diagnostic hysteroscopy
1. Pelvic infection.
2. Pregnancy.
3. Cervical cancer.
4. Heavy uterine bleeding.
The hysteroscoipic view is best in the immediate postmenstrual phase,
but a diagnosis is usually possible at any time, even during menstruation.
v
Technique
The patient should be in lithotomy position with the hips well flexed and
the buttocks slightly over the edge of the table to allow
unimpeded access. The perineum and vaginas are usually washed with a
warmed antiseptic solution. Agentle bimanual examination should be
done to determine the size and position of the uterus.
Complications of diagnostic hysteroscopy
Diagnostic hysteroscopy is a safe procedure, and complications are
uncommon.
1. Vasovagal reaction. When negotiating the cervix or distending the
uterine cavity.
2. Uterine perforation rare.
3. Infection & excessive bleeding rare
Operative hysteroscopy
Indications
1. Adhesiolysis
2. Endometrial ablation/resection (has been superseded by the newer
second-generation ablative techniques).
3. Metroplasty
4. Myomectomy (intracavity or sub mucous fibroids and < 3-5 cm in
diameter).
5. Polypectomy
6. Proximal fallopian tube cannulation
7. Removal of IUCD
8. Target biopsy
9. Treatment of cervical and interstitial pregnancy
10. Treatment of missed abortion
11. Tubal sterilization
Complications of operative hysteroscopy
A. early
1. Uterine perforation;
2. Fluid overload with low –viscosity fluids particularly those which are
electrolyte-free.
Apart from cardiac, and pulmonary effects, major electrolyte imbalance
lead to build –up of free fluid in the brain, hyponatremia, hypo-
osmolality,
cerebral
oedema,
and cellular necrosis.
Clinically characterized by nausea, vomiting, seizures, coma and even
death.
3. Hemorrhage
4. Gas embolism
5. Infection.
6. Cervical trauma
7. Electrosurgical burns.
B-late complications
1. Intrauterine adhesions
2. Uterine rupture in pregnancy (after metroplasty or myomectomy)
3.Hematometra after endometrial ablation
4. Post ablation sterilization syndrome (after endometrial ablation).
Developed painful swelling of the fallopian tubes secondary to retrograde
menstruation.
5. Pregnancy (after endometrial ablation).
6. Cancer (after endometrial ablation).
Cystoscopy
Cystoscopy involves passing a small-diameter telescope, either flexible or
rigid, through the urethra into
the bladder. A cystoscope with an operative
channel can be used to biopsy any abnormality, perform bladder neck
injection, retrieve stones and resect
bladder tumours.
Indications
•
Haematuria.
•
Recurrent urinary tract infection.
•
Sterile pyuria.
•
Short history of irritative symptoms.
•
Suspected bladder abnormality (e.g. diverticulum, stones, fistula).
•
Assessment of bladder neck.
Complications
•
Urinary tract infection.
•
Rarely, bladder perforation.