~1
~
Third Stage Internal Medicine Dr. Fadhil
Clinical Immunology 7
Anaphylaxis
What is anaphylaxis?
An acute systemic allergic reaction
The result of a re-exposure to an antigen that elicits an IgE mediated response
Usually caused by a common environmental protein that is not intrinsically harmful
Often caused by medications, foods, and insect stings
It is a Type I hypersensitivity
Examples of allergens: food- like peanuts, tomato, mango, shellfish; venoms; medications
– antisera, dextran& penicillin.
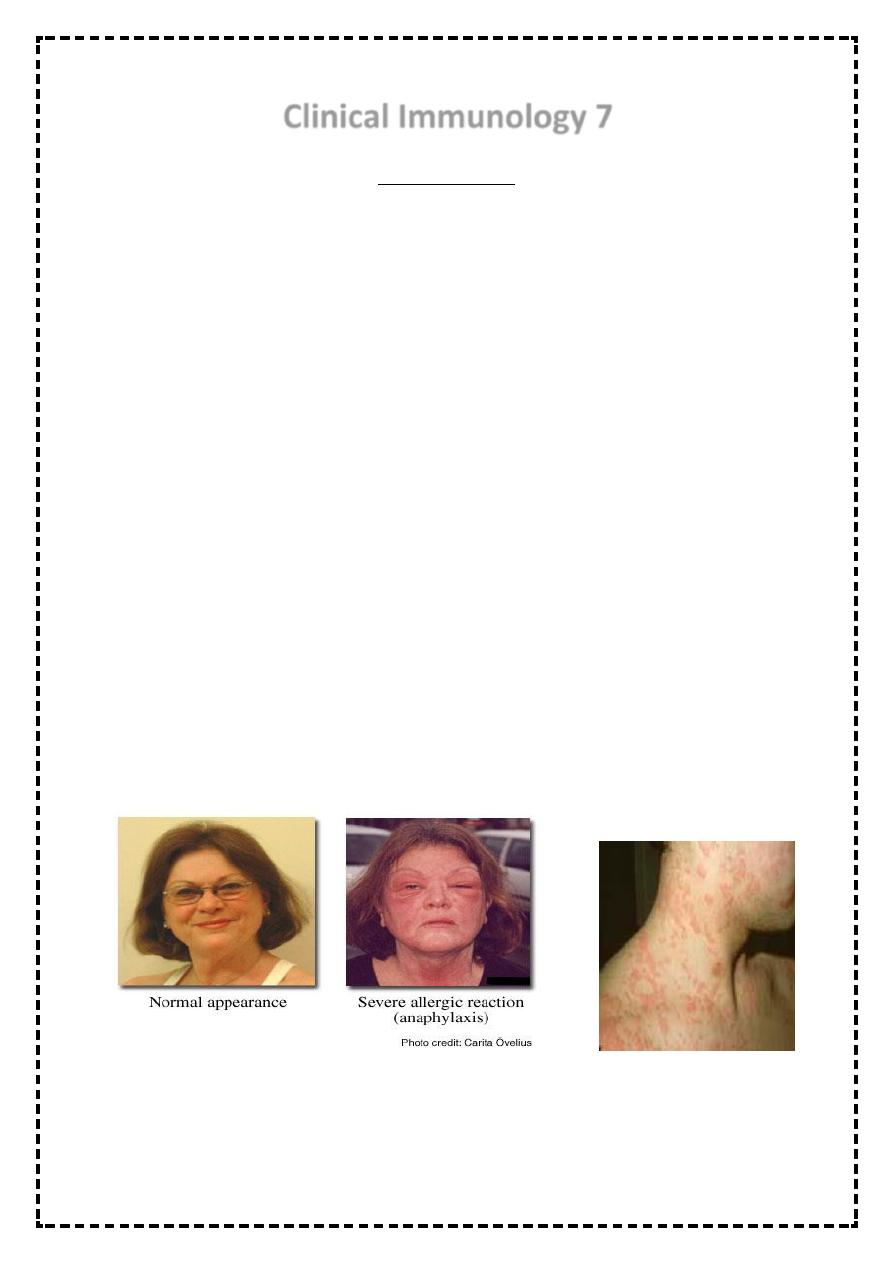
The initial symptoms may appear innocuous: tingling, warmth and itchiness. The ensuing
effects on the vasculature give vasodilatation and edema. The consequence of these may
be no more than a generalized flush, with urticaria and angioedema.
Symptoms
Peripheral vasodilation
– vascular permeablility (edema)
Bronchospasm
Cardiac arrhythmias
Smooth muscle contractions
• More serious sequelae are hypotension, bronchospasm, laryngeal edema and cardiac
arrhythmia or infarction. Death may occur within minutes.
• Early recognition and treatment are essential.
~2
~
• Cutaneous manifestations of pruritus &urticaria with or without angioedema are
characteristic of this disease.
• Other features include drowsiness, loss of consciousness ,conjunctival injection, flushing ,
stridor, sweating, warm peripheries due to profound vasodilatation, hypotension ,
wheeze, cardiac arrhythmias, diarrhea , &abdominal pain.
Etiology
• There is no convincing evidence that age , sex , race ,occupation, or geographic location
predispose a human to anaphylaxis except through exposure to an immunogen.
• According to most studies ,atopy does not predispose individuals to anaphylaxis from
penicillin or insect venom.
Diagnosis
• depends largely on an accurate history of appearance of symptoms within minutes of
exposure to an offending immunogen.
• At postmortem ,evaluation for an IgE in the heart blood of a dead patient had proven the
etiology of systemic anaphylactic reaction as a cause of death.
Treatment
• 1-prevention of further exposure to an allergen.
• 2- ensure an airway potency.
• 3- oxygen
• 4- restoration of BP by lying the patient in a flat position & giving I.V. fluid.
• 5- giving adrenaline which is a life saving drug, o.5 mg intramuscularly repeated every 5
minutes if shock persists.
• Antihistamines like chlorpheneramine 10-20mg slow IV. High doses of steroids like 100mg
IV hydrocortisone repeated on need.
• B2-agonist nebulizers are used if there is sever bronchospasm.
• If hypoxia is severe, assisted ventilation may be required.
• Desensitization has a well- established place in the management of this disorder,
particularly if the exposure is unavoidable or unpredictable as in insect stings.
Angioedema & Urticaria
~3
~
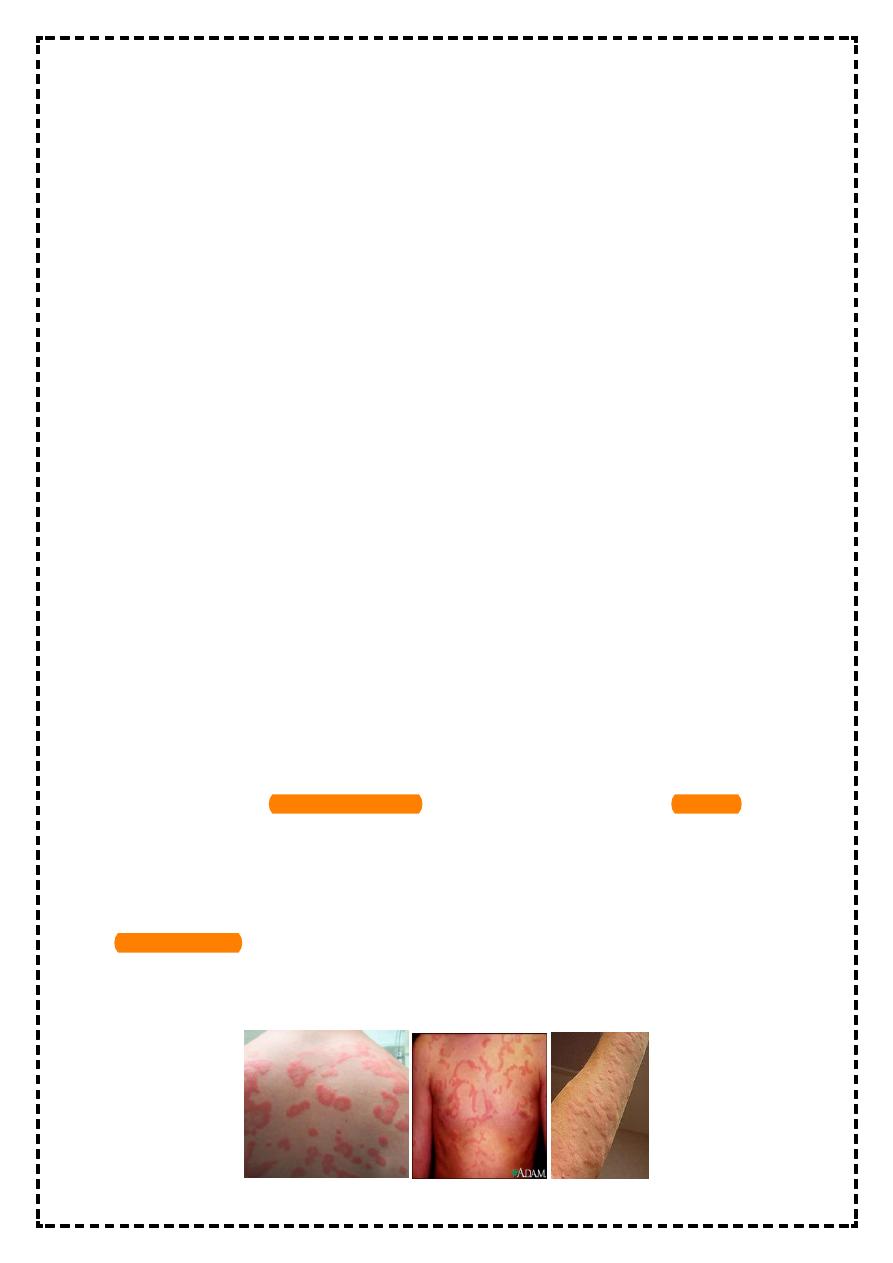
Urticaria
The term urticaria is widely used to describe an eruption of wheals. It is now also increasingly
being used to define a disease characterized by short-lived itchy wheals, angio-oedema or both
together.
Urticaria is a superficial swelling of the skin (epidermis and mucous membranes) that results in a
red, raised, itchy rash. It is also known as hives, nettle rash, or wheals.
• Urticaria is described as ‘acute’ if it lasts less than 6 weeks and ‘chronic’ if it persists
beyond this period.
Angio-oedema
• Angio-oedema is a deeper form of urticaria oedema in the dermis and submucosal or
subcutaneous tissues due to increased vascular permeability.
• Can involve the face, eyelids and/or lips.
• Less commonly the tongue and larynx.
• Onset can be dramatic.
• Final events in the pathogenesis involves degranulation of cutaneous mast cells which
releases a number of inflammatory mediators ( including histamine) which in turn make
the dermal and sub dermal capillaries leaky.
• In most cases the underlying cause is unknown. Occasionally these conditions are
secondary to viral or parasitic infections, drug reactions ( e.g. NSAIDs, penicillin, ACE
inhibitors, opiates), food allergy (e.g. to strawberries& seafood), or rarely SLE.
• There is evidence for an autoimmune etiology in some of ‘idiopathic’ cases.
• Urticaria/angioedema is commoner in atopic individuals and usually presents in children
and young adults.
Clinical features:
• Urticaria produces cutaneous swellings or wheals developing acutely over a few minutes.
They can occur anywhere on the skin and last between minutes and hours before
resolving spontaneously.
• Lesions are intensely itchy and show no surface change or scaling. They are normally
erythematous but if very acutely swollen, they may appear flesh- colored or whitish and
people often mistake them for blisters.
• Angioedema with subcutaneous involvement presents as soft tissues swelling ( edema)
especially around the eyes, the lips and the hands but this is rarely itchy.
Investigations:-
~4
~
• The history is the most useful factor in the diagnosing urticaria. The physical urticaria
should be reproducible by applying the relevant stimulus.
• Urticaria & angioedema may appear separately or together as cutaneous manifestations
of localized non pitting edema, A similar process may occur at mucosal surfaces of upper
respiratory & gastrointestinal tracts.
Classification of angioedema& urticaria
can be either:
*immune mediated - IgE on mast cells and basophils cross-link with the allergen and activates
the cells e.g.- urticaria induced by
a- medication (penicillin), pollens, food, , helminthes)
b- physical(dermographism: linear wheals after brisk stroke with a firm object., cold, exercise,
cholinergic drugs)
*complement mediated - mast cells are activated directly by complements ( mainly by C3a, C4a,
and C5a) e.g.
a-hereditary angioedema:type-1, type-2.
b- acquired angioedema: Type-1, type-2.
c-necrotizing vasculitis
d-serum sickness
e- reactions to blood products
*non-immune mediated - activation of mast cells by non IgE mechanisms e.g.
a-direct mast cells releasing agents: opiates, antibiotics, radio-contrast media
b-agents altering arachidonic acid metabolism: aspirin(NSAIDs), benzoates
*autoimmune mediated - circulating auto-antibodies activate mast cells
The mechanisms above lead to degranulation of dermal mast cells in response to a number of
stimuli, which causes vasodilatation, dermal oedema and a perivascular infiltrate of lymphocytes
and eosinophils . If deeper it causes angioedema.
Substances released in urticaria include; histamine, prostaglandin D2, leukotrienes C4 and D4,
platelet activating factor & cytokines.
* Most cases remain idiopathic
Treatment:-
~5
~
• Any underlying cause should be treated
appropriately. Patients should avoid salicylates and opiates as they can degranulate mast cells.
• Oral antihistamines (H1 blockers) are the most useful in the treating the idiopathic cases.
Therapy should be started with regular use of a non-sedating antihistamine( e.g.
cetirizine 10 mg daily or loratidine 10 mg daily).
• If control provokes difficult, addition of a sedating antihistamine, an H2- blocker or
dapsone may be helpful. Steroids are kept for troublesome urticaria& high doses may be
needed.
Hereditary angioedema(HAE)
• Characterized by recurrent self limiting attacks, involving the skin, subcutaneous tissues,
upper respiratory tract or GIT.
• The attacks may be precipitated by local trauma(eg. dental procedures, infection)& last
for 2 days.
• It is an autosomal dominant disorder ; caused by decreased production of C-1 inhibitor
protein which is a complement component that inhibits the activation of the classical
pathway & kinin cascade. Activation of which gives rise to local pain & swelling. HAE is
also called inherited C-1 inhibitor deficiency.
• It usually not associated with urticaria & allergic diseases.
• It usually present in adolescents& early adulthood. Family history is found in 80% of
cases.
TREATMENT
• Attenuated androgen( danasol)& fresh frozen plasma which contains high concentration
of C-1 inhibitor. Anti-fibrinolytic agent, tranexamic aminocaproic acid( cyclocapron) can
be used as a prophylactic agent in such patients.



