Placenta previa Assist. prof. dr. Alaa AL-Naser
Objectives1.understand what placenta previa
2.describe the types &risk factors
3.learn what are sign and symptom
4.potential clinical implications and management
Placenta previa is used to describe a placenta that implanted over or very near the internal cervical os.
Placenta is disk shape and at full term measures about seven inches in diameter, central thickness 2.5 cm, and weight 450-500 g.
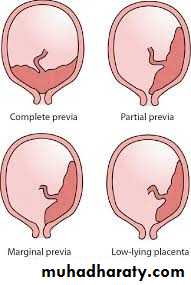
Four placental configurations have been defined
Complete(total) placenta previa
The placenta completely covers the internal os. A central placenta previa occurs when the internal os is approximately equidistant from the anterior and posterior placental edges.20- 30 percent of placenta previas are central.
Partial placenta previa The placental edge partially covers the internal cervical os.
Marginal placenta previa : The edge of placenta is adjacent to the internal os, but does not cover it.
Low-lying placenta
The placenta is implanted in the lower uterine segment, placental edge does not reach the internal os but in close proximity to it.
INCIDENCE
Placenta previa complicates approximately 4 per 1000 pregnancies that are over 20 weeks of gestation.
Risk factors
uterine factors include scarring of upper lining tissue of the uterus(prior caesarian deliveries, prior instrumentation such as D&C, any type of surgery involving the uterus)
Placenta previa occurs in 0.9 percent of women with one prior cesarean delivery, 1.7 percent of those who have had two prior cesarean deliveries, and 3 percent of those who have had three or more cesarean deliveries.
Increasing parity (the incidence of placenta previa is 0.2 percent in nulliparous versus up to 5 percent in grand multiparas.
Increasing maternal age (incidence is 0.03 percent in nulliparous women aged 20 to 29 years versus 0.25 percent in nulliparous women ≥40 years of age.
Maternal smoking carbon monoxide hypoxia induced compensatory placental hypertrophy.
Residence at higher altitudes(placenta grow larger to compensate for decreased function)Multiple gestation 40%of placenta previa in multifetal gestation.
Infertility treatment
Short interpregnancy interval
Nonwhite ethnicity
Low socioeconomic status
Cocaine use
CLINICAL MANIFESTATIONS
The characteristic clinical presentation of placenta previa is painless vaginal bleeding after 20 weeks of gestation; this occurs in 70 to 80 percent of patients. 10 to 20 percent of women present with uterine contractions associated with bleeding, while fewer than 10 percent are incidentally detected by ultrasound examination and remain asymptomatic.Bleeding is likely to occur during the third trimester because of development of the lower uterine segment and the increasing presence of uterine contractions, which dilate and efface the cervix. Changes in the cervix and lower uterine segment apply shearing forces at the inelastic placental attachment site, resulting in placental detachment and bleeding. Separation can also be caused by vaginal examination or coitus.
However, bleeding may begin earlier, and some abortions may result.
Bleeding initially is rarely so profuse is to prove fatal.
Hemorrhage from implantation site in placenta previa continue after delivery of placenta because lower uterine segment contract poorly.
Associated conditions
Placenta accreta : Placenta accreta complicates 5 to 10 percent of pregnancies with placenta previa. The presence of a placenta previa and one or more cesarean delivery scars places a woman at very high risk for placenta accrete, inecreta, percreta (abnormal firm attachment of placenta) and need for cesarean hysterectomy.
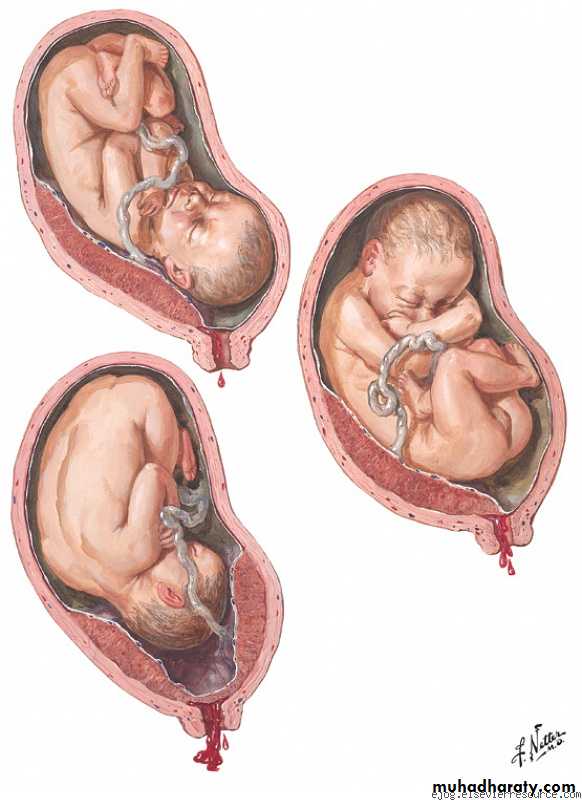
Malpresentation : The large volume of placenta in the lower portion of the uterine cavity may predispose the fetus to assume a non-cephalic presentation.
(PPROM) : Antepartum bleeding due to decidual hemorrhage is the most common symptom of placenta previa and is a risk factor for PPROM.
Intrauterine growth restriction : This association was present after controlling for maternal age, education, parity, smoking, alcohol and illicit drug use, adequacy of prenatal care, maternal race, and obstetrical complications.
Vasa previa and velamentous umbilical cord : Vasa previa (the fetal vessels course through the membrane and present at the cervical os. velamentous umbilical cord insertion are often associated with low-lying placentas and marginal previas.
Congenital anomalies
Amniotic fluid embolism
Coagulation defect coagulopathy is rare with placenta previa even when there is extensive separation from the placental site, because throboplastin which incites intravascular coagulation that common characterizes placental abruption readily escape through cervical canal than being forced into maternal circulation.
Postpartum endometritis
DIAGNOSIS
Placenta previa or abruption should always be suspected in woman with uterine bleeding during the latter half of pregnancy.the absence of abdominal pain and uterine contractions has been used to distinguish placenta previa from abruptio placentae, some women with placenta previa have painful uterine contractions in addition to bleeding, thus the diagnosis of placenta previa must be determined by sonographic examination.
the diagnosis is seldom be established firmly by clinical examination unless a finger passed through the cervix and the placenta is palpated. Such digital cervical examination is never permissible unless woman in operating room with all preparations for immediate C/S, even gentlest digital examination can cause torrential hemorrhage.
Ultrasonography
Trans abdominal ultrasonography is used for initial placental localization, identification of echogenic placental tissue overlying or proximate to the internal cervical os (a distance greater than 2 cm from the os excludes the diagnosis of previa, although the placenta may be low lying). with the patient's bladder partially full. Specific situations that need to be appreciated when performing sonographic examination for placenta previa include
An over-distended bladder can compress the anterior lower uterine segment against the posterior lower uterine segment to give the appearance of a previa (false positive). The diagnosis of placenta previa should not be made without confirming placental position after the patient has emptied her bladder..
A posterior previa can be missed near term if the fetal head is low in the pelvis since acoustic shadowing from the fetal calvarium may obscure the placental location. In these cases, the cervix may be better visualized by placing the patient in Trendelenburg position and/or gently pushing the fetal head cephalad.
The placental location may also be obscured by a hematoma or a lower uterine segment contraction
Trans vaginal — If trans abdominal ultrasound examination shows a placenta previa or the findings are uncertain, a trans vaginal sonogram should be performed to better define placental position(gentle vaginal probe used to avoid cervical slipping)
Trans labial (trans perineal) ultrasound imaging is an alternative technique that provides excellent images of the cervix and placenta.
Magnetic resonance imaging (MRI) has been used to provide a more precise method of placental localization, detection of posterior placenta previa, its high cost, limited availability, can be helpful in the setting of accreta and percreta.
Placental migration: 18-20 weeks gestation 12% of placenta low lying, of those non covering the os previa not persist and no Hg.
Those covering the os at mid pregnancy 40% persisted, special those with previous uterine scar.
MANAGEMENT
Women with P.P may considered in one of the following categories:
The fetus is preterm and there are no other indications for delivery.
The fetus is reasonably mature.
Labor has ensured.
Hemorrhage is so sever as to mandate delivery despite gestational age.
ASYMPTOMATIC PLACENTA PREVIA
General principles of management of asymptomatic placenta previa after 20 weeks of gestation include, serial trans vaginal ultrasound evaluations at four-week intervals (beginning at 28 weeks of gestation) to reevaluate placental location. Development of the lower uterine segment over time often relocates the stationary lower edge of a marginal or low-lying placenta away from the internal os. Avoidance of coitus and digital cervical examination in the second and third trimester, avoid exercise and decrease their physical activity in the third trimester, since physical activity may provoke uterine contractions and bleeding..
Counseling to seek immediate medical attention if contractions or vaginal bleeding occur
ACUTE CARE OF SYMPTOMATIC PLACENTA PREVIA
An actively bleeding placenta previa is a potential obstetrical emergency. These women should be admitted to the Labor and Delivery Unit for maternal and fetal monitoring, anti-shock garments may restore an adequate blood pressure in women who are hemodynamically unstable from hemorrhage.
Establish intravenous access and administer crystalloid
One or two large bore intravenous lines are inserted and crystalloid (Ringers lactate or normal saline) is infused to maintain hemodynamic stability and adequate urine output (at least 30 mL/hour).Blood bank and laboratory monitoring
A blood type and antibody screen should be performed. If bleeding is heavy or increasing, cross-matching two to four units of packed red blood cells.
transfusion of blood products in a woman with an actively bleeding placenta previa should be guided by the rate of bleeding and changes in hemodynamic parameters (eg, blood pressure, maternal and fetal heart rates, peripheral perfusion, and urine output), as well as the hemoglobin. A reasonable approach is to transfuse a hypotensive patient whose blood pressure fails to respond after two liters of crystalloid have been infused.
A maternal coagulation profile is checked if there is a suspicion of coexistent abruption or after massive blood loss or transfusion
When the placental and cord anatomy are unknown or difficult to discern, we perform either an Apt test or Kleihauer-Betke analysis to determine whether fetal bleeding from ruptured vasa previa or velamentous cord is also occurring
Fetal monitoring
The fetal heart rate is continuously monitored. Loss of reactivity, persistent minimal variability, fetal tachycardia, recurrent late decelerations, or a sinusoidal heart rate are nonreassuring signs suggesting the potential presence of fetal hypoxia or anemia.
Maternal monitoring
We use a cardiac monitor and automated blood pressure cuff to follow maternal heart rate and blood pressure. Urine output is evaluated hourly with a Foley catheter attached to a urimeter. Vaginal blood loss can be estimated by weighing or counting perineal pads
Tocolysis
We do not administer tocolysis to actively bleeding patients. Tocolysis may be considered if contractions are present.
Indications for delivery : Delivery is indicated if any of the following occur:
A non-reassuring fetal heart rate tracing unresponsive to maternal oxygen therapy, left-sided positioning, and intravascular volume replacement
Life-threatening refractory maternal hemorrhage
Significant vaginal bleeding after 34 weeks of gestation
Cesarean delivery is the delivery route of choice.
General anesthesia is typically administered for emergency cesarean delivery, especially in hemodynamically unstable women or if the fetal status is non-reassuring.
CONSERVATIVE MANAGEMENT AFTER AN ACUTE BLEED
Most women who initially present with symptomatic placenta previa respond to supportive therapy and do not require immediate delivery.
Select women with placenta previa may be discharged if
1. bleeding has stopped for a minimum of 48 hours and there are no other pregnancy complications.
2.Be able to return to the hospital within 20 minute.
3.Have an adult companion available 24 hours a day who can immediately transport the woman to the hospital if there is light bleeding or call an ambulance for severe bleeding.
4.Be reliable and able to maintain bed rest at home
5.Understand the risks entailed by outpatient management
Iron supplementation may be needed for optimal correction of anemia. Stool softeners and a high-fiber diet help to minimize constipation and avoid excess straining that might precipitate bleeding
A course of antenatal corticosteroid therapy should be administered to symptomatic women between 24 and 34 weeks of gestation to enhance fetal pulmonary maturity. We do not administer steroids to asymptomatic women or those whose first bleed is after 34 weeks of gestation.
Rh(D)-negative women should receive Rh(D)-immune globulin with the initial bleeding episode.
PPROM can occur despite the presence of a complete placenta previa. In these cases, each condition is managed independently. tocolytics may be given to hemodynamically stable, uninfected women to allow administration of antenatal corticosteroids prior to 32 weeks of gestation
DELIVERY
Timing
Severe persistent hemorrhage is an indication for delivery, regardless of gestational age. In women who are asymptomatic or clinically stable, most clinicians perform amniocentesis at 36 weeks of gestation to assess fetal pulmonary maturity and then schedule cesarean delivery if the results predict mature lungs.
Route
Complete previaA cesarean delivery is always indicated when there is sonographic evidence of a complete placenta previa and a viable fetus. Vaginal delivery may be considered in rare circumstances, such as in the presence of a fetal demise or a previable fetus, as long as the mother remains hemodynamically stable.
Low-lying placenta
there is a reasonable possibility of vaginal delivery without hemorrhage when the placenta is more than 20 mm from the internal os, so a trial of labor is appropriate if there are no other contraindications to vaginal birth .
Marginal previa
vaginal delivery could occasionally be performed safely in women with marginal previa because the fetal head tamponades the adjacent placenta, thus preventing hemorrhage.
Procedure
Two to four units of packed red blood cells should be available for the delivery. Appropriate surgical instruments for performance of a cesarean hysterectomy should also be available since there is at least a 5 to 10 percent risk of placenta accreta, even in the absence of a prior cesarean deliveryThe surgeon should try to avoid disrupting the placenta when entering the uterus=hemorrhage from fetal vessels can result in significant neonatal anemia, sonographic localization is helpful in determining the position of the hysterotomy incision . If the placenta is in an anterolateral location, a vertical incision can be made in the lower uterine segment on the opposite side from the placenta. If the placenta wraps around the cervix from the anterior to posterior lower uterine segment in the midline, a transverse or vertical incision may be possible above it, although this often results in extension into the upper uterine segment. When incision of the placenta is unavoidable, the infant should be delivered rapidly and the cord promptly clamped.
OUTCOME
1.Hemorrhage
The risks of antepartum, intrapartum, and postpartum hemorrhage are all significantly increased in women with placenta previa . Rapid, significant loss of intravascular volume can lead to hemodynamic instability, decreased oxygen delivery, decreased tissue perfusion, cellular hypoxia, organ damage, and death.
2.Maternal mortality
The maternal mortality rate is less than 1 percent in industrialized countries, but remains high in developing countries where maternal anemia, lack of medical resources, and home births are common
3.Neonatal morbidity and mortality
Neonatal morbidity and mortality rates in pregnancies associated with placenta previa have fallen over the past few decades because of the introduction of conservative obstetrical management, the principal causes of neonatal morbidity and mortality are related to preterm delivery, rather than fetal anemia, hypoxia, or growth restriction.
4. The recurrence rate of placenta previa is 4 to 8 percent.
5. Ceaserian hysterectomy if placenta accreta.
.
.