Congenital
Abnormalities Of TheLarynx
Laryngomalacia (congenital laryngeal stridor)
Exaggerated infantile typeThe epiglottis is an omega shaped .
The aryepiglottic folds are approximated.
The laryngeal inlet is a cruciate slit, the edges of which are sucked together by each inspiration.
Clinical features
Inspiratory stridor at or soon after birth, croaking in character, diminished by rest, increased by exertion, less in prone position disappears in 2nd-5th years of life.
Diagnosis
history and examination.
Flexible fiberscope examination, or direct
laryngoscopy
Treatment
-Reassurance
-Tracheostomy may rarely needs
Subglottic stenosis
-Most cases are acquired
-Inspiratory stridor is unaffected by posture.
-The voice is normal.
-Feeding is difficult and failure to thrive occurs in severe cases.
=Direct laryngoscopy and bronchoscopy is required.
-If infant fails to thrive a tracheostomy is required.
-Laser treatment to vaporize the stenosis
Subglottic haemangioma
This condition is clinically indistinguishable from subglottic stenosis
Laser treatment is particularly effective.
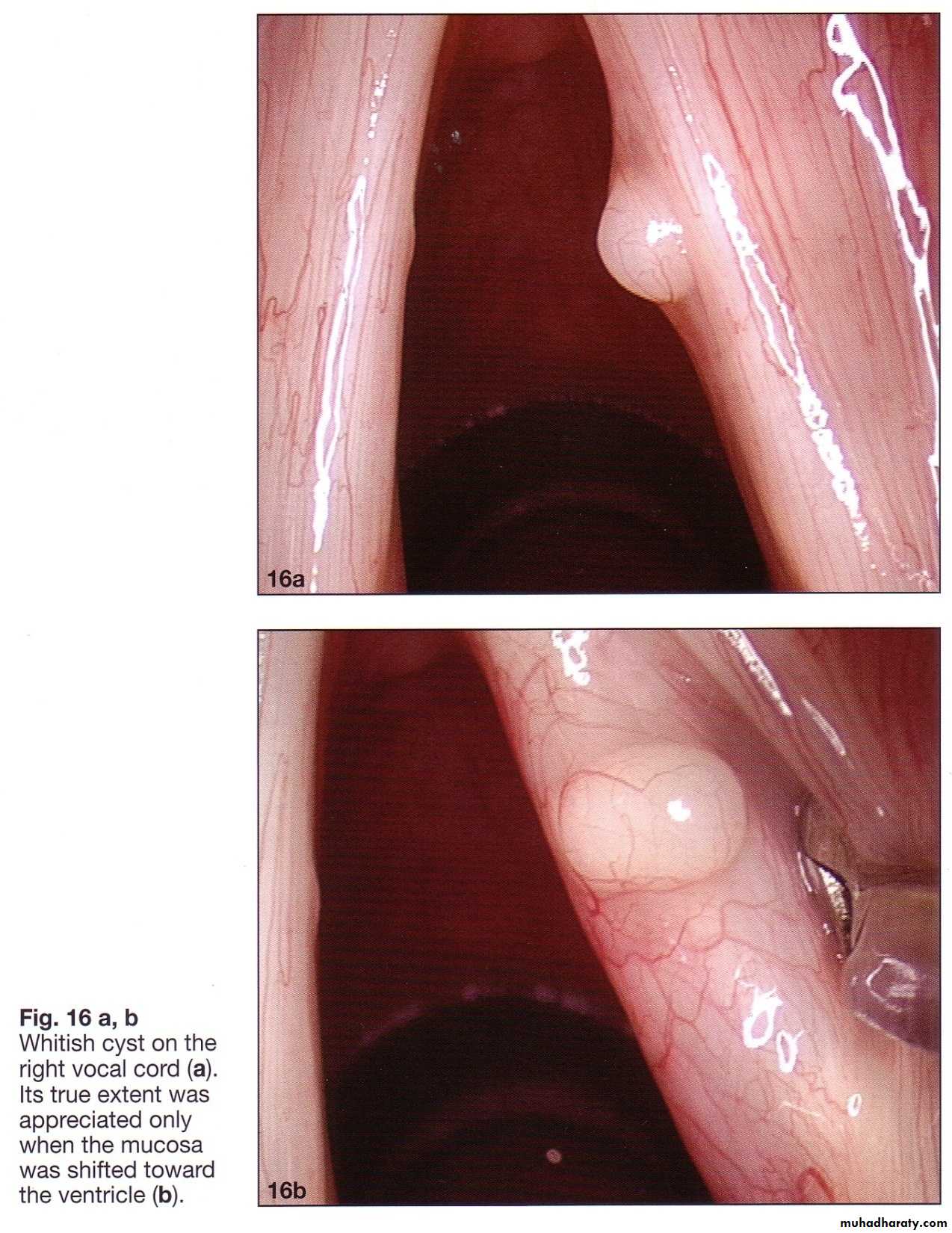
Laryngeal cyst
Small cysts // hoarseness or a muffled crylarger // inspiratory stridor.
Dx:
-fibroptic flexible laryngoscope
Treat.
direct laryngoscopy is required to evacuate and uncap a cyst.
Laryngeal web
Almost in the anterior half of the glottis. The symptoms vary with the size of the web.
Hoarseness is usually present.
Inspiratory stridor occurs in severe cases.
rigid or fibro-optic laryngoscopy.
No treatment, in the milder forms.
Laser excision.
Tracheostomy. when stridor and dyspnea are
severe.
Vocal cord palsy
Caused by damage to the recurrent laryngeal nerve in neck or chest usually from birth trauma. Inspiratory stridor and hoarseness in a neonate.
Fibreoptic laryngoscopy is essential for diagnosis.
Treatment : cordoplasty
TRAUMATIC
CONDITIONS OF THE LARYNX1.Direc injuries
a. Compression(closed)injuriesAs in blows and strangulation.
Pathology
1.Bruising of skin may occur
2. Surgical emphysema
3. Sub mucosal haemorrhage
4. Perichondritis / if infection supervenes.
5. Fracture of the laryngeal cartilages
6. Adhesions
7. Stenosis
Clinical features
1. Dyspnoea may be marked.
2. Hoarseness or weakness of the voice, is common.
3.Dysphagia is a frequent symptom.
4.Haemoptysis is usually slight.
5.Pain is variable.
6.Tenderness may be elicited by palpation.
7. Crepitus is difficult to detect.
8. Submucosal haemorrhages can be seen on indirect laryngoscopy.
Diagnosis
The history and physical signs.
Plain X-rays or CT scan may confirm the presence of a fracture in a cartilage.
Treatment
The chief danger of these injuries is interference with respiration.1.Tracheostomy may be urgently required.
2. Systemic antibiotics
prophylactically in every case. They must be continued if perichondritis threatens or supervenes.
3.Incision and drainage are needed if abscess formation.
b. Penetrating (open) wounds
Usually fatal They are caused by gunshot injuries, stabs or cuts.Pathology
The laryngeal injuries are generally accompanied by damage to vital structures. These depend upon the direction of the injury ..
1.Oblique wounds usually involve the great vessels of the neck.
2. Anteroposterior wounds may cause death from involvement of the cervical spine
3. Transverse wounds may involve the larynx only. Survival is rare even in this type
Clinical features
1. Dyspnoea results fromHaemorrhage into the larynx and tracheobronchial tree
Swelling of the soft tissues of the larynx
Displacement of fractured cartilages
Mediastinal emphysema
• Perichondritis and/or stenosis
2. Haemorrhage may be massive and rapidly fatal.
Treatment
1.Clamping and ligature of divided vessels.
2.Intubation through the open wound may prevent asphyxia.
3.Tracheostomy should be performed as soon as the facilities are permit.
4. Removal of foreign bodies with excision of devitalized tissues and suturing of the mucosa.
5.Systemic antibiotics.
6.Fluids intravenously or by nasogastric tube.
No food must be given by mouth for at least 24 hours
2. Burns and scalds
Aetiology Inhalation of irritant fumes , steam or gases.
Swallowing of corrosive fluids.
Pathology
Oedema of the laryngeal inlet is the usual findingClinical features
Dyspnoea. Pain and dysphagia are usual.
Treatment Usually conservative.
1.Rest to bed, strict rest of the voice, and sedative drugs.
2.Steroids intravenous or intramuscular injection.
3.Antibiotics to prevent secondary infection.
4.Analgesic drugs.
5.Tracheostomy or laryngotomy must be performed if the airway is compromised.
3.Radiotherapy reactions
Severe local reactions in the larynx may follow radical irradiation
Dyspnoea
Discomfort on swallowing may result
Pain results from perichondritis or cartilage necrosis
Treatment
Preventive or curative.
1.Elimination of oral sepsis
2.Tracheostomy is rarely necessary
3.Systemic antibiotics when perichondritis is present or threatening.
4.Analgesic preparation
5.Laryngectomy in severe intractable cases where necrosis is present.
4.Inhaled foreign bodies
rare, but sharp foreign bodies, such as pins or glass, may be impacted in the larynx.Large foreign bodies, such as boluses of food, are almost immediately fatal when impacted in the larynx.
Clinical features
Dyspnoea & Cough
Hoarseness or aphonia may appear due to oedema.
Perichondritis and stenosis follow when the foreign body is retained or causes severe trauma.
Treatment
A 'bear hug' (Heimlich's manoeuver) from behind with hands clasped just below the xiphisternum may expel the object.
Removal by direct laryngoscopy as soon as possible.
Tracheostomy or laryngotomy may be necessary in an emergency
Systemic antibiotics should be given to prevent bronchopulmonary infection.
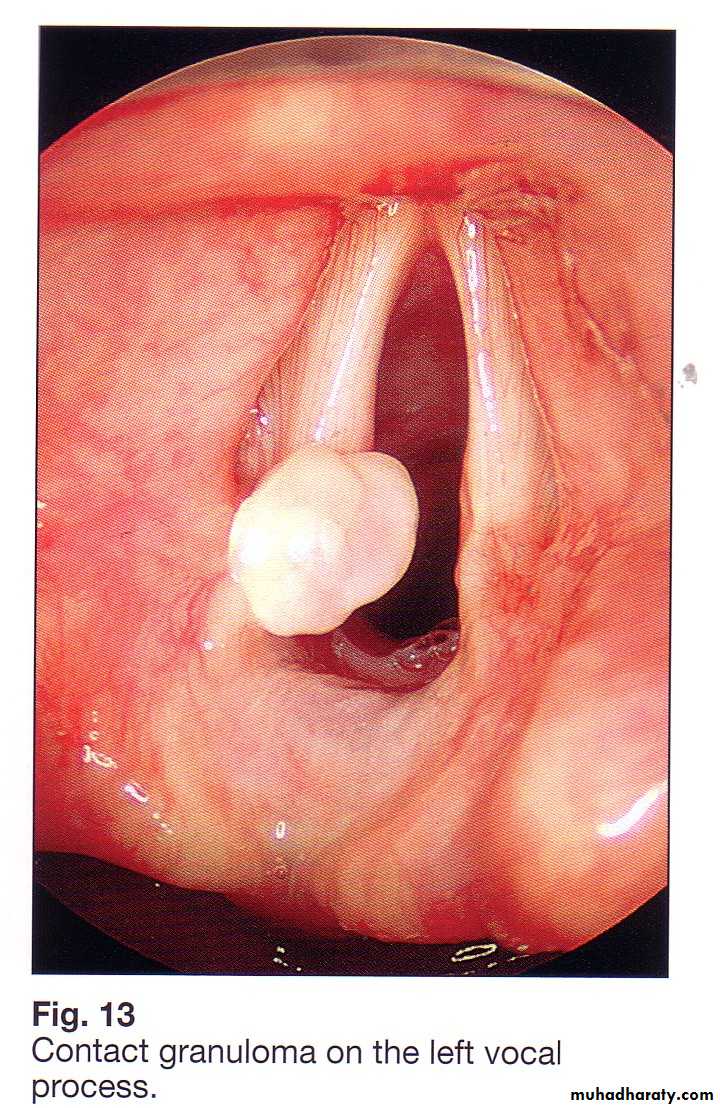
5.Intubation injuries
Aetiology
1.Rough intubation
2.Prolonged intubation
3.Too large a tube.
Pathology
Superficial abrasions.
Granulomatous formation esp. the vocal processes of the arytenoid cartilages. F/M:(4:1) .
Subglottic oedema. In children, rarely in adults.
Clinical features
Hoarseness
Dyspnoea, Sometimes.
Treatment
Voice rest may suffice.
Endoscopic removal of granulomas .
Tracheostomy for dyspnoea.
6.Acute submucosal haemorrhages on the vocal cords
(acute haemorrhagic laryngitis)
Aetiology
The haemorrhages after coughing, shouting, weight-lifting and injuries to the larynx.
Clinical features
Hoarseness occurs suddenly after a vocal strain.
Pain may occur.
The haemorrhages may be single or multiple and the remainder of the cords may be injected. Rarely the whole of one cord is involved. The haemorrhages may organize into the granulomatous or fibrous nodules.
Treatment
Vocal rest. // microlarryngeal surgical removal
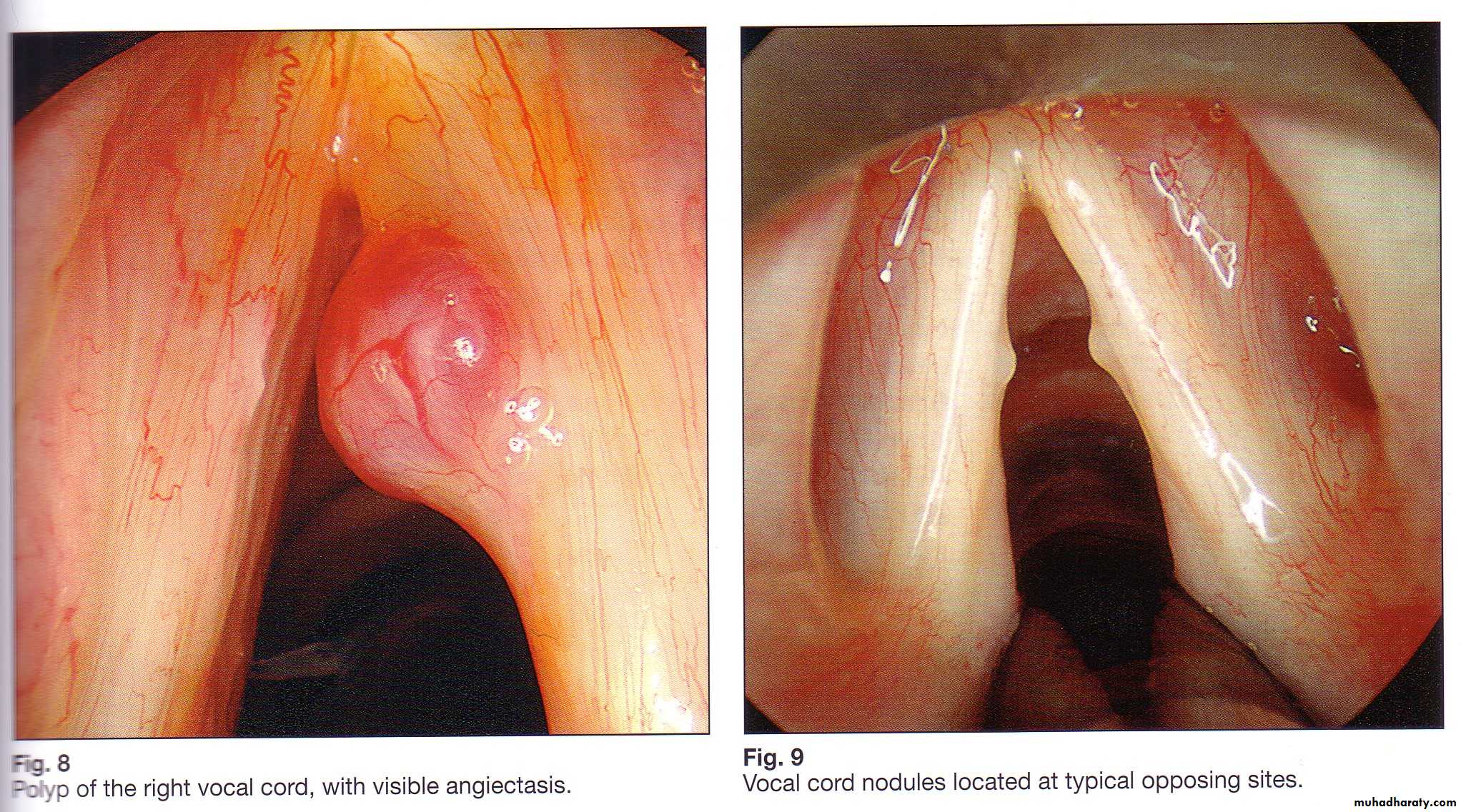
7.Singer's nodes ; vocal nodules
Voice abusers; singers ,actors, teachers, mothers of young children and persons talking to the deaf ,more common in women and in singers who sing above their natural range.Pathology
Localized hyperkeratosis. The site is constant, at the junction of the anterior third and posterior two-thirds of the free edge of one or both vocal cords. The nodules never become neoplastic.
Clinical features
Increasing hoarseness. suddenly or slowly and insidiously
Vocal fatigue.
Nodules are more commonly bilateral and symmetrical, vary in size from pinhead to that of a grape-pip.
Treatment
Vocal rest
Removal by direct laryngoscopy
Speech therapy helps to re-educate voice production
8.Contact 'ulcer'
AetiologyAn uncommon , almost in male adults esp. singers and street vendors and results from the hammering of one vocal process of the arytenoid cartilage against the other.
Coughing is always detrimental.
Clinical features
Discomfort in the throat ;slight or severe.
Huskiness; slight or severe `
Vocal fatigue.
Referred otalgia may occur.
‘Kiss ulcer' is the common finding on indirect laryngoscopy. the granuloma of one side fitting into the 'ulcer' crater of the other.
Treatment
Vocal rest for 2 or 3 weeks may be necessary.
Steroids have proved successful
Removal of thickened epithelium by microlaryngoscopy.