Physical Properties of the Lungs
Lecture 3Dr. Suroor Mohamed
• Objectives: Respiratory Physiology
• Elastic recoil of the lung (surface tension).• Surfactant (Chemical composition, functions and factors affecting its production).
• Define compliance, and diseases affected on it.
• Dead space ( physiological & anatomical one).
Physical properties that affect lung function:
◦ Compliance.◦ Elasticity.
◦ Surface tension
Compliance
● Distensibility (stretchability): Ease with which the lungs can expand.
● Change in lung volume per change in transpulmonary pressure. ΔV/ΔP
● 100 x more distensible than a balloon.
◦ Compliance is reduced by factors that produce resistance to distension.
Elasticity
● Tendency to return to initial size after distension.
● High content of elastin proteins. (Very elastic and resist distension &Recoil ability.
● Elastic tension increases during inspiration and is reduced by recoil during expiration
Elastic recoil tendency of the lung. The lungs have a continual elastic tendency to collapse
and therefore to pull away from the chest wall. It is caused by two different factors:
The presence of elastic fibers (elastin) throughout the lungs which are stretched by lung inflation and therefore attempt to shorten. They account for about one third of the recoil tendency.
The surface tension of the fluid lining the alveoli which is more important, accounts for about two
thirds of the recoil tendency, and causes a continual elastic tendency for the alveoli to collapse. The surface tension is caused by intermolecular attraction between the surface molecules of the alveolar fluid that is each molecule pulls on the next one.
Surface Tension
● Force exerted by fluid in alveoli to resist distension.
⚫ Lungs secrete and absorb fluid, leaving a very thin film of fluid.
◦ This film of fluid causes surface tension.
◦ Fluid absorption is driven (osmosis) by Na+ active transport
◦ Fluid secretion is driven by the active transport of Cl out of the alveolar epithelial cells.
● H20 molecules at the surface are attracted to other H20 molecules by attractive forces. Force is directed inward, raising pressure in alveoli
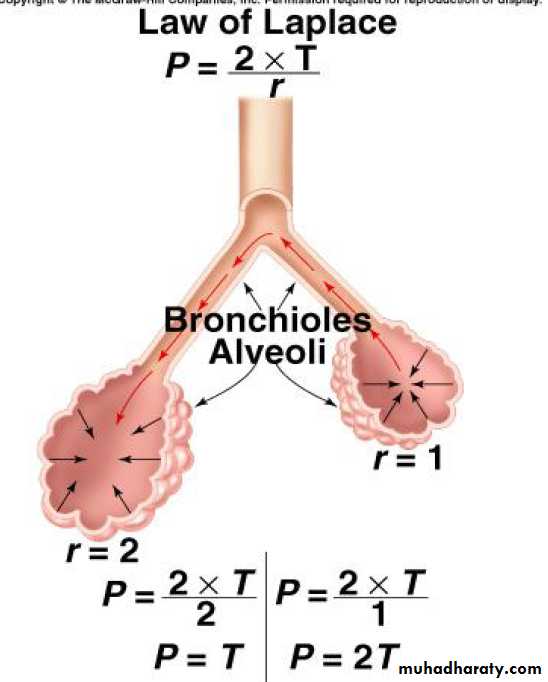
Law of Laplace:
◦ Pressure in alveoli is directly proportional to surface tension; and inversely
proportional to radius of alveoli.
◦ Pressure in smaller alveolus would be greater than in larger alveolus, if surface tension were the same in both.
• Elastic behavior of the lungs
• Reasons for recoil of lung:• Tissue elasticity (1/3rd )
• Surface tension (2/3rd)
• Surface Tension
• Alveoli lined by thin film of fluid Secreted by the epithelial cells → Surface tension
• Tendency to reduce the size of the alveolus due to intermolecular attraction.
• Law of Laplase
• In spherical structures (alveoli) the distending pr equal 2 times the tension divided by the radius
• Large alveoli (large radii) have low collapsing pr and are easy to keep open
• Small alveoli (small radii) have high collapsing pressures and are more difficult to keep open
• In the absence of surfactant, the small alveoli have a tendency to collapse (atelactasis)
•
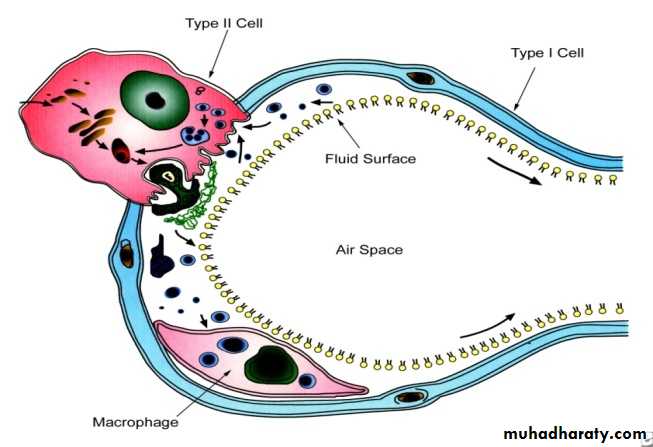
• Surfactant :
• Is phospholipid material that a surface tension lowering agent present in the alveolus between the alveolar fluid and air• Secreted by type II alveolar cells
• Consists primarily of the Dipalmitoyl phosphatidyl choline (DPPC), other lipids, and proteinsSurfactant
• ●Lowers surface tension. Reduces attractive forces of hydrogen bonding by
• becoming interspersed between H20 molecules. Surface tension in alveoli is reduced.
• ● As alveoli radius decreases, surfactant’s ability to lower surface tension increases.
• ● Disorders: RDS. ARDS
DPPC
62%
Phosphatidylglycine
5%
Other phospholipids
10%
Neutral lipids
13%
Proteins
8%
Carbohydrate
2%
Functions of Surfactant
• ↓Surface tension → ↓ distending pressure from 15 to 3mmHg →• It maintains alveolar stability (prevents over distension or collapse of alveoli)
• Alveolar surface tension is inversely proportional to the number of surfactant molecules per unit area.
• ↑ Diameter of the alveolus (inspiration) → ↓ the number of surfactant molecules per unit area →↑surface tension → prevents overdistension
• ↓Diameter of alveoli(expiration) →↑number of surfactant molecules per unit area→↓ surface tension →prevents collapse
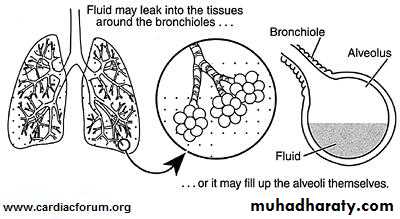
• Surfactant prevents pulmonary edema and keeps the alveoli dry.
• If surfactant was not present in the alveoli, the unopposed surface tension in the alveoli will produce a 20mm Hg force favoring transudation of fluid from the blood into the alveoli leading to pulmonary edema• In newborn infants, surfactant prevents hyaline membrane disease or infant respiratory distress syndrome (IRDS)
• In the fetus, development of surfactant is completed only by 31-32 weeks of intrauterine life. If birth occurs before this stage of development →lungs fail to expand (IRDS). Treatment : bovine surfactant
• Surfactant increases lung compliance (Distensibility)
• It reduces the work of breathing (↓ elastic recoil of lung)• Factors affecting surfactant:
• 1) Prematurity:• 2) Hormones:
• Thyroid hormones surfactant
• Glucocorticoids ( cortisone) surfactant
• Insulin surfactant
• Fetal hyperinsulinemia occurs in diabetic mothers incidence of IRDS in infants born to diabetic mothers.
• 3) Smoking surfactant
• 4) Bronchial obstruction surfactant
• 5) Pulmonary arterial obstruction surfactant
• 6) Long term O2 therapy (100%) surfactant
• RESPIRATORY DEAD SPACE (RDS)
• The portion of tidal volume that does not take part in gas exchange :
• Anatomical dead space
• Physiological dead space
• Anatomical dead space (ADS):
• It is the volume of air in the respiratory passage from nose to the terminal bronchiole.
• It is normally equal in millilitres to your B.WT in pounds. 68 kg male (150 lb ) anatomical dead space 150 mL
• It may be measured by Fowler's method (analysis of the single- breath N2 curves).
• Pulmonary ventilation and alveolar ventilation:
• Pulmonary ventilation (RMV )= TV × RR• = 50012 = 6 L/min
• Alveolar ventilation=TV-ADS × RR
• = 500-150 × 12= 4.2L
• Wasted ventilation = ADS × RR
• = 150 12 = 1.8L/min
• Rapid shallow breathing produces much less alveolar ventilation than slow deep breathing at the same RMV
RR
30/min
10/min
Alveolar ventilation
(200-150)30 =
50 30 =
1500ml
(600-150)10=
450 10=
4500ml
Tidal volume
200mL
600mL
RMV
6L
6L
• Total (physiologic) dead space
• Physiological dead space = anatomic dead space + alveolar dead space
• Alveolar dead space is the air in the non functioning alveoli (underperfused or nonperfused alveoli and overventilated alveoli)
• Normally alveolar dead space air is about 5-10mL → physiological dead space = anatomic dead space
• Increase in physiological dead space is seen in pulmonary embolism and COPD.
• Total dead space is calculated by Bohr equation from the PCO2 of expired air (PEco2), the PCO2 of arterial blood (PaCO2), and tidal volume (VT)
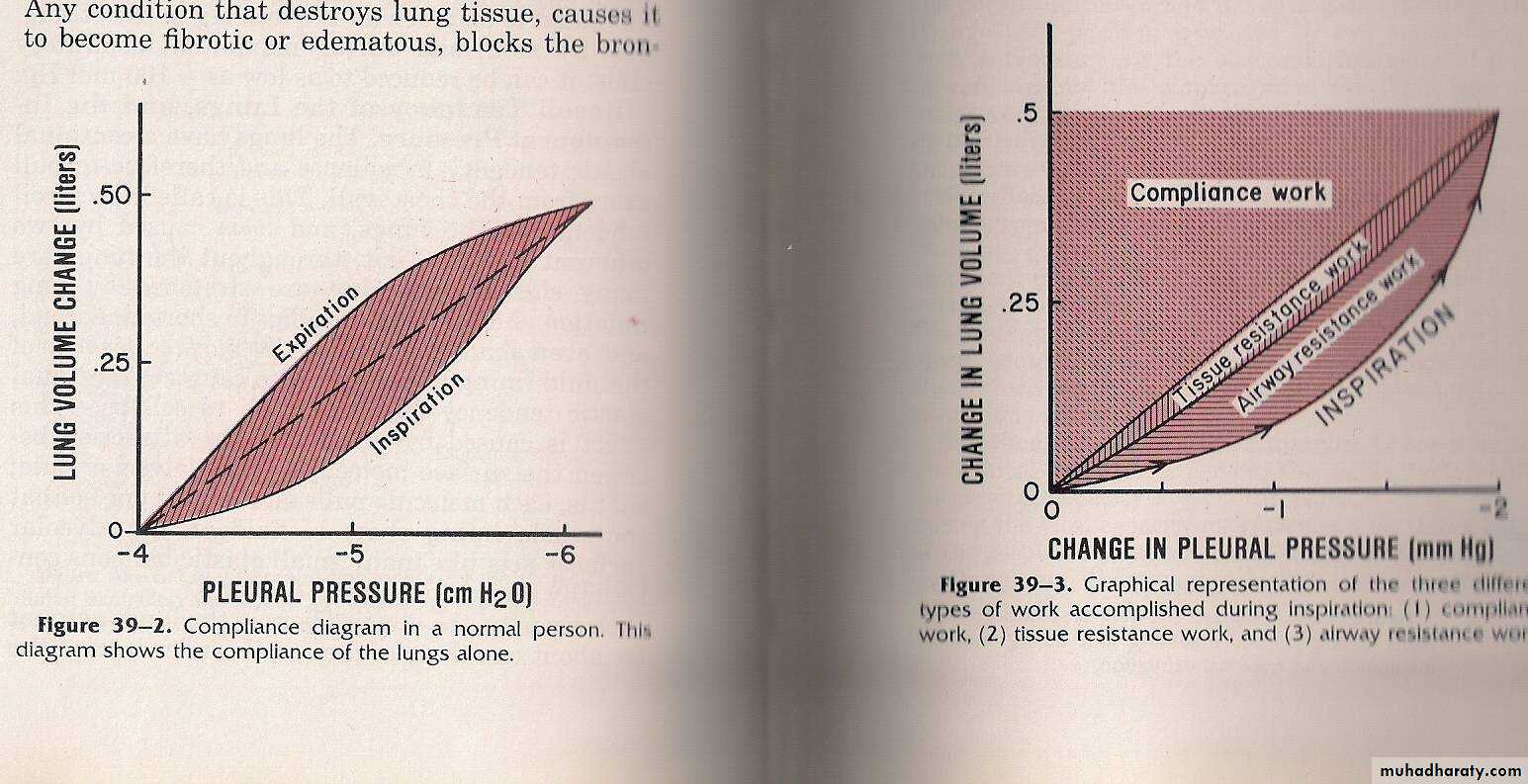
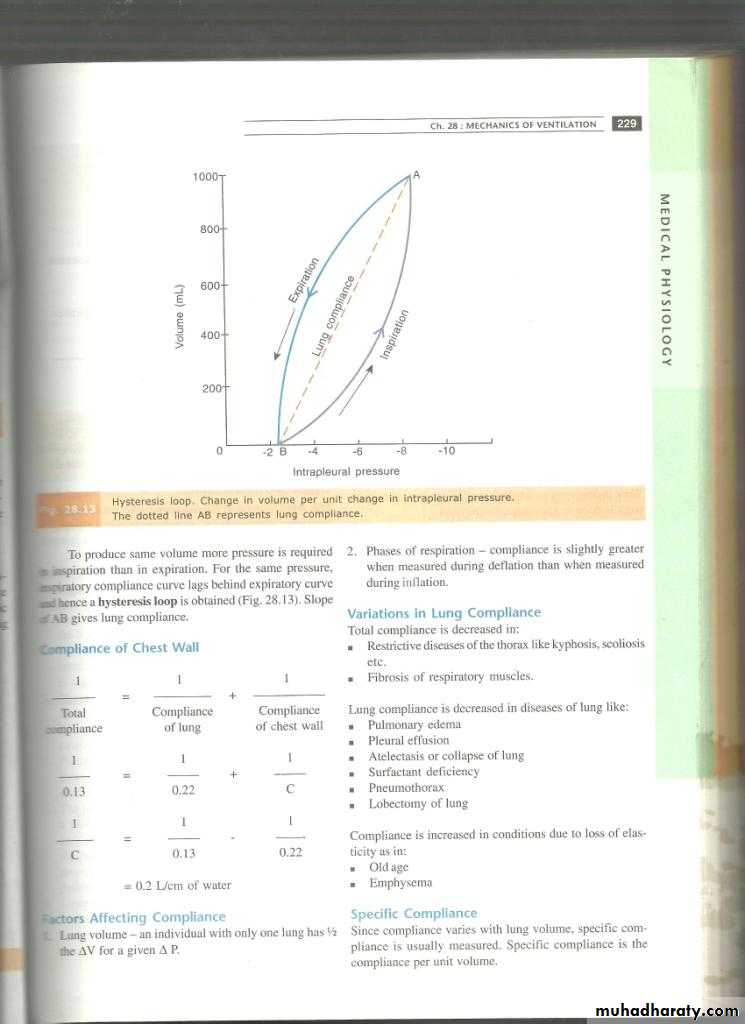
Compliance(pressure- volume relationship)
• Definition: Change in lung volume per unit change in airway pressure• Compliance = V/ P
• Compliance is a measure of the distensibility or the ease with which the lungs and thoracic wall can be expanded
• Total compliance is the compliance of thorax and lungs together = 0.13 L/ cm H2O (≈ 0.735559 mm Hg)
• For every cm H2O pressure change, the lungs and thorax expand by 0.13 L.
• When the compliance of thorax and lungs are taken separately, the value will be more than total compliance.
• At FRC, compliance of thorax alone is 0.22 L/cm H2O and that of lungs alone is also 0.22 L/ cm H2O
• Compliance of lung alone:
• Volume changes are plotted against transpulmonary pressure changes, i.e., intra-esophageal pressure changes are recorded during inspiration and expiration.• To produce same volume more pressure is required in inspiration than in expiration.
Intra-pleural pressure
• Inspiratory compliance < expiratory compliance → (hysteresis loop)
Compliance of chest wall
1 1 1---------- = ---------------- + -----------------
Total Compliance Compliance
Compliance of lung of chest wall
1 1 1
--------- = ----------- + ---------0.13 0.22 C
1 1 1
--------- = ----------- - ------------C 0.13 0.22
= 0.2L / cm H2O
Variations in lung compliance
scoliosis
kyphosis
4.pneumothorax
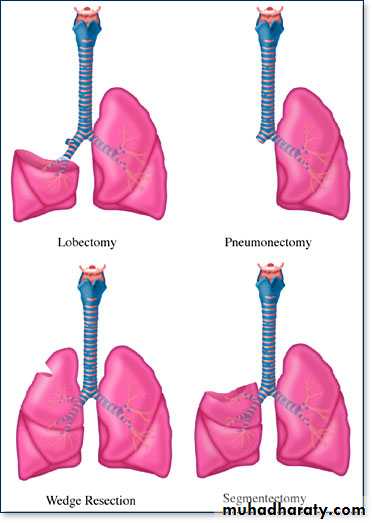
3. Lobectomy
&pneumoctomy1.Pulmonary edema
Compliance is ↑ in conditions due to loss of elasticity (old age & emphysema)
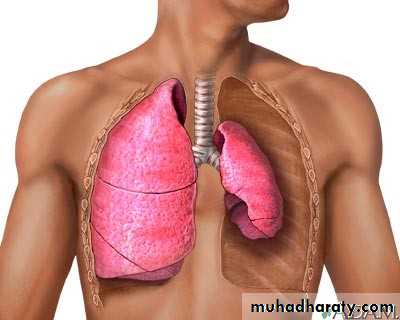
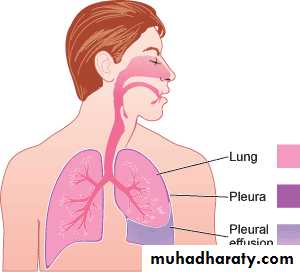
2. Pleural effusion
• Lung compliance is ↓
• in diseases of lung
• ↓Total compliance:
• Restrictive diseases of the thorax (kyphosis, scoliosis )
• Fibrosis of respiratory muscles
5. Pulmonary fibrosis
• Emphysema is generally caused by smoking.
• The alveoli have broken, leaving spaces where gas exchange cannot take place.
• Compliance decreases, so It is difficult to expel the air in the lungs.
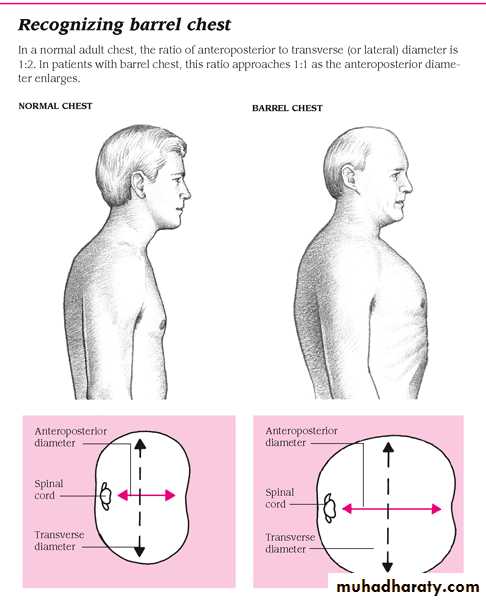
• When the ribs are continually raised with each breath, they eventually remain in the upright position, causing a barrel chest
• Work of breathing
• Work is done only in inspiration and forced expiration• No work is done in normal quiet expiration.
• Work = Force × Displacement
• = Pressure × Volume
• During inspiration, all dimensions of thorax increase and certain amount of work has to be done by the respiratory muscles to overcome 3 factors:
• Compliance work or elastic work (65%): This work is done to overcome elastic resistance, i.e., work done in stretching the elastic tissues of chest wall and lungs.
• Tissue Resistance Work (7%): This work is done to overcome inelastic tissue resistance or viscous resistance, i.e., in moving inelastic tissues.
• Airway Resistance Work (28%): overcome frictional force of air moving through the respiratory passages.
• In pulmonary diseases all three types of work:
• Pulmonary fibrosis compliance work and tissue resistance work .• Airways obstruction Airway resistance work
• Airway resistance work: During heavy breathing (air flow through respiratory passages at very high velocity).
• Expiratory work occur and sometimes become greater than inspiratory work in heavy breathing, increased airway resistance or increased tissue resistance.
• In bronchial asthma increase in airway resistance many folds during expiration but much less so during inspiration.