1
Non neoplastic epithelial disorders ( vulvar dystrophies ) :
Definition :
A group of benign vulval epithelial growth disorders .
Classification
1. Squamous cell hyperplasia ( previously called hyperplastic dystrophy ) not
attributable to any associated skin lesion .
2. Lichen sclerosus ( previously called hypoplastic dystrophy ) .
3. Other dermatoses : Squamous cell disorder attributable to a specific skin lesion as
psoriasis .
If both squamous cell hyperplasia and lichen sclerosus are present , they are
reported separately ( previously known as mixed dystrophy ) .
Etiology :
The cause of non neoplastic vulval epithelial disorders is not understood , but the
following factors are discussed :
I- Chronic mechanical skin irritation aided by warmth and humidity .
II- Deficiency of some nutritional factors as folic acid , iron , vitamin B
12
or
vitamin B
2
.
III- Autoimmune disorder
:
Such as in achlorhydria.
IV- Somatostatin and substance P :
These peptides are reported to be secreted by the epidermal cells to suppress skin
overgrowth . If these substances are deficient , overgrowth will occur while if they
are abnormally elevated , skin atrophy will result .
V- Chalones :
A group of tissue specific proteins suggested to be important in controlling the
rate of skin growth . However , the chemical nature of these substances could not
identified .
VI- Other theories as allergy , metabolic disorders as DM , hormonal
changes at menopause , fungal HPV or HSV infections .
Pathology :
I- Squamous cell hyperplasia ( found mainly in premenopausal age ) :
* Grossly :
2
- The lesion appears usually as a well demarcated raised whitish area previously
called "leukoplakia" .
- As the condition is associated with pruritus , the gross picture can be markedly
modified by scratching , so the lesion may appear pinkish with small fissures
and scratching marks .
- Although the lesion is primarily vulval , the perineum and the inner sides of the
thigh can be also affected .
- The malignant potential for this lesion is 5% . So cellular atypia and
malignant lesion should be excluded before the final diagnosis is set .
* Microscopically :
1. Hyperplasia affecting all epidermal layers
2. Deepening of rate pegs ( rate ridges ) due to acanthosis .
3. The dermis shows hyalinization , collagenization , loss of elastic fibers and chronic
inflammatory cell infiltration .
II- Lichen sclerosus ( most cases occur in early menopausal years but can
occur in any age , it is the most common white lesion on the vulva ) :
* Grossly
: The lesion usually affects the labia and spreading inwards to affect the
vaginal introitus , but perianal skin , under the breast or the lower abdomen may
also be affected . The skin is thin and wrinkled ( parchment-like appearance ) ,
taking the bluish-white color , and in advanced stages, there is loss of
subcutaneous fat leading to flattening of the labia and narrowing of subcutaneous
fat leading to flattening of the labia and narrowing of the vaginal introitus .
* Microscopically :
1. Atrophy of all layers of the epidermis leading to flattening of the rete pegs , but
with hyperkleratosis .
2. Subepithelial homogenous acidophilic zone .
3. The dermis shows hyalinization , collagenization , loss of elastic fibers and chronic
inflammatory cell infiltration .
Diagnosis :
I- Symptoms :
1. Asymptomatic in early stages .
2. Pruritus which is the most common presentation .
3. Superficial dyspareunia specially in lichen in lichen sclerosus .
4. Vulval soreness .
5. Slight bleeding due to extensive tissue excoriation .
6. Leukoplakia in hyperplastic type .
7. Vaginal discharge may be associated .
3
II- Signs :
1. The gross picture of the lesion is evident .
2. Associated predisposition as DM or allergy .
3. HPV or HSV infections .
III- Investigations :
1. Toluidene blue directed biopsy .
2. Colposcopy and colposcopically directed biopsy .
3. Investigating predisposing factors as DM , allergy , autoimmune disorders (specially
achlorhydria) , and lower genital infection ( monilia , HPV or HSV)… etc.
Treatment :
I- General measures as in vulvitis .
II- Treatment of any predisposing factors .
III- Specific treatment of squamous cell hyperplastic type :
1. Any of the fluorinated corticoids topically 2-3 times / day for 4Ws +
antiallergics . This is the main therapy with 90% success .
2. Skinning vulvectomy or laser vaporization are done in resistant cases .
IV- Specific treatment for lichen sclerosus :
1. Testosterone propionate 2% cream twice / day for at least 6 months . Lifelong
maintenance may be needed .
2. Esterogen in postmenopausal cases . Although estrogen has no effect on
epidermal metabolism , it improves the vascularity of the dermis .
3. Clobetasol ( Dermovate ) : Corticosteroid appears to be very effective in
controlling resistant lesions . It causes suppression of the immune activity in
the vulval skin .
4. Oral retinoids : 20 – 30 mg/ day for 16 Ws . It gives 65% success rate .
V- Follow up ( mandatory for early detection of malignancy ) :
1. Self examination using a mirror in squatting position .
2. Regular vulval examination by a gynecologist .
3.immediate investigation fo any suspiciuos lesion.
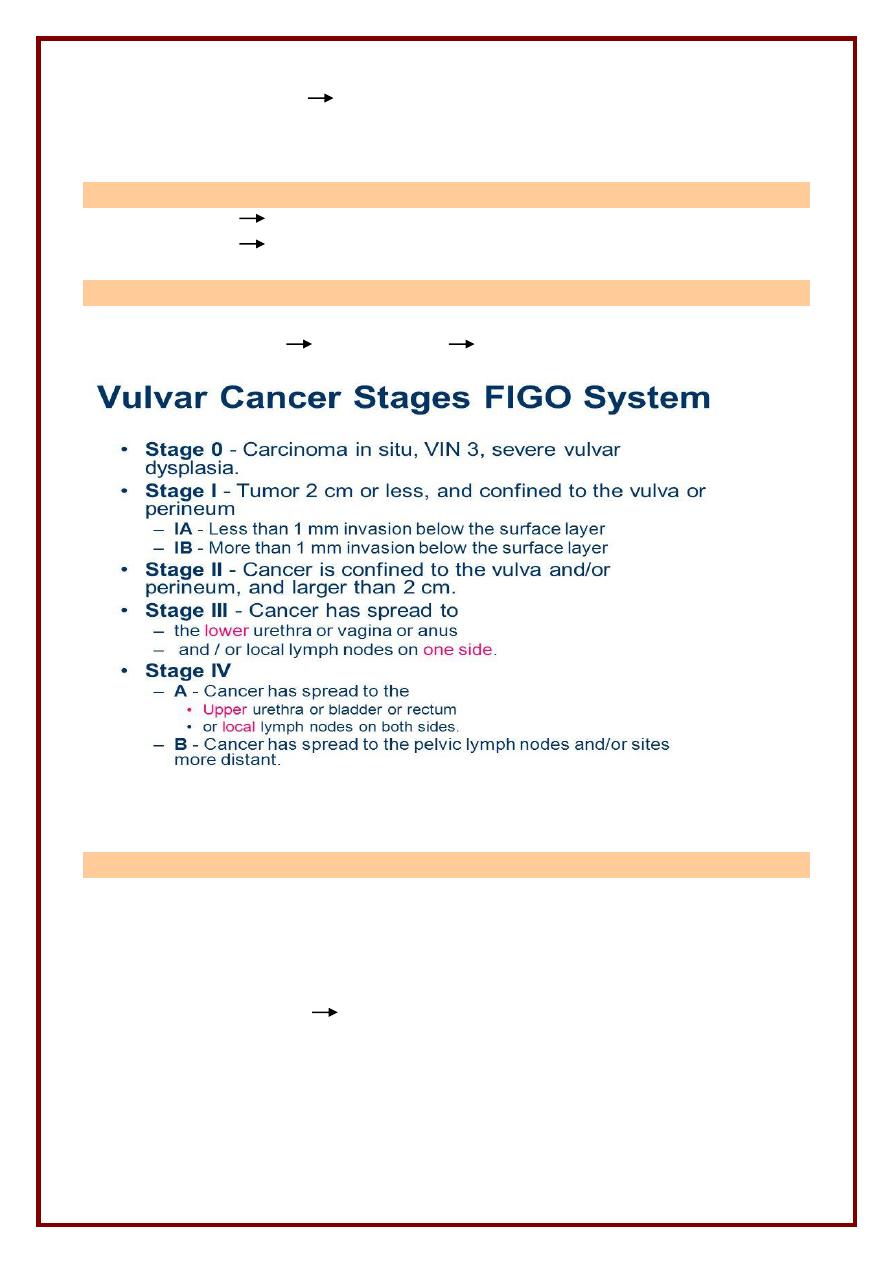
Vulval intraepithelial neoplasia
Abnormal cells develop in the celllayers covering the skin of vulva,it is not
malignant but may be turned to malignant
Most common type,associated with HPV infection may be
VIN 1 less than one third of skin has abnormal cells
4
VIN 2 less than 2 third of skin has abnormal cells
VIN 3 more 2 third of skin has abnormal cells.
Symptoms
Pain, itching, chang the colour of vulva
Diagnosis
By speculum , colposcopy, direct biosy
Treatement
1) Follow up.
2) Imiquimod cream.
3) Laser therapy.
4) Surgery.
Invasive Vulvur Carcinoma
Predisposing Factor
* Age 60 – 70 years 4% ( the 4
th
genital tract tumor )
* Vulvar dystrophy in 50% of cases .
* Chronic irritation infection , mechanical ( pruritis vulvae ) , chemical
Pathology
Mac. Cauliflower ………. ulcer ………. infiltrating
Mic. Squamous cell Carcinoma ( usually well differentiated )
Spread
Local vagina , perineum , urethra , bladder , rectum , bones .
5
Lympbatic ( mainly ) there is cross-over between the 2 sides
Superficial and deep inguinal lymph nodes
Femoral L.N.
Eternal and common iliac L.N.
Clinical picture
1. Symptoms feeling of mass ……….. discharge …….. bleeding
2. Signs Mass ……… ulcer …………… LN enlargement
Investigations
Any suspicious area ( change in color / contour )
Colposcopy Toluidie blue biopsy ( punch , multiple )
Treatment
* Surgery
Surgical removal of affected skinalong with 1cmrim of normal tissue arround it
+ Removal of affected lymph node.
Sentinel lymph node biopsy can be done instead of L.N. dissection.
* Radiation
1) no clear margin during histopathology.
2) L,N. dissection not done because the patient is not healthy enough.
3) cancer near vagina, urethra and anus.
4)surgery can not be done beacause of medical health of patient.
* Prognosis
6
Cancer of Clitoris or that reaching Urethra or Vagina have bad prognosis
( early vascular spread , direct spread to LN of Cl)
