Enteric (Typhoid and Paratyphoid ) Fever
TUCOM
Internal Medicine
5
th
year
21-1-2020
Dr. Hasan. I. Sultan
Enteric (Typhoid and Paratyphoid ) Fever
Enteric fever is a systemic disease characterized by fever and
abdominal pain due to infection by S. Typhi or S. Paratyphi
serotypes A, B, and C.
Salmonellae are gram negative, flagellated, aerobic bacilli. It
infect both humans and animals but serotypes S. Typhi
and S. Paratyphi infect human only. Killed by
pasteurization or food irradiation.
Most commonly, food-borne or waterborne transmission
results from fecal contamination by ill or asymptomatic
chronic carriers. The incubation period is typically about
10–14 days but can be longer.

Pathogenesis:
After a few days of bacteraemia, the bacilli
localise, mainly in the lymphoid tissue of the small
intestine, resulting in typical lesions in the Peyer’s patches
and follicles. These swell at first, then ulcerate and usually
heal. After clinical recovery, about 5% of patients become
chronic carriers (i.e. continue to excrete the bacteria after
1 year); the bacilli may live in the gallbladder for months
or years and pass intermittently in the stool and, less
commonly, in the urine.
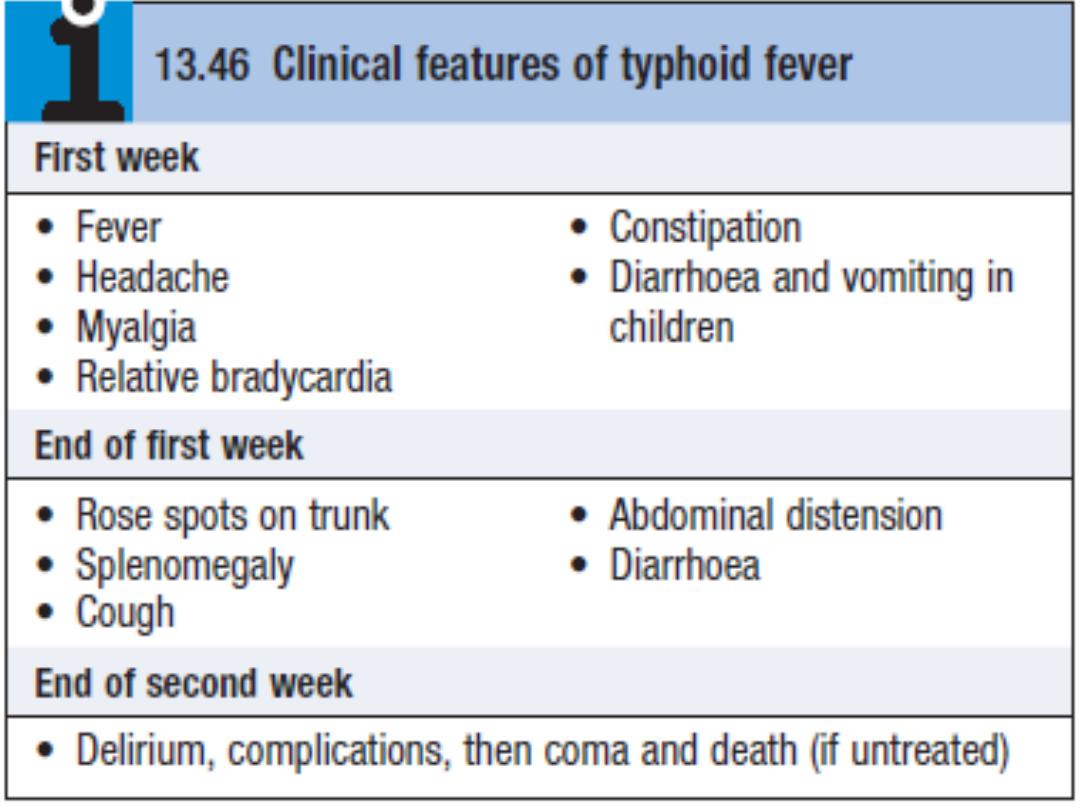
Clinical features
Typhoid fever:
• The incubation period
is about 10–14 days
• The onset
may be insidious. The temperature rises in a
stepladder fashion for 4 or 5 days with malaise, headache,
drowsiness and aching in the limbs. Constipation may be
present, although in children diarrhoea and vomiting may
be prominent early in the illness. The pulse is often slower
than would be expected from the height of the
temperature, i.e. a relative bradycardia.
• At the end of the first week
, a rash may appear on the
upper abdomen and on the back as sparse, slightly raised,
rose-red spots, which fade on pressure. It is usually visible
only on white skin. Cough and epistaxis occur.
• Around the 7th–10th day
the spleen becomes palpable.
Constipation is then succeeded by diarrhea and
abdominal distension with tenderness. Bronchitis and
delirium may develop.
• If untreated, by the end of the 2nd week
the patient may
be profoundly ill.
Paratyphoid fever:
The course tends to be shorter and milder than that of
typhoid fever and the onset is often more abrupt with acute
enteritis. The rash may be more abundant and the intestinal
complications less frequent.
Clinical features are outlined in the box below.

Rose spots," the rash: red, maculopapular rash located primarily on
the trunk and chest.
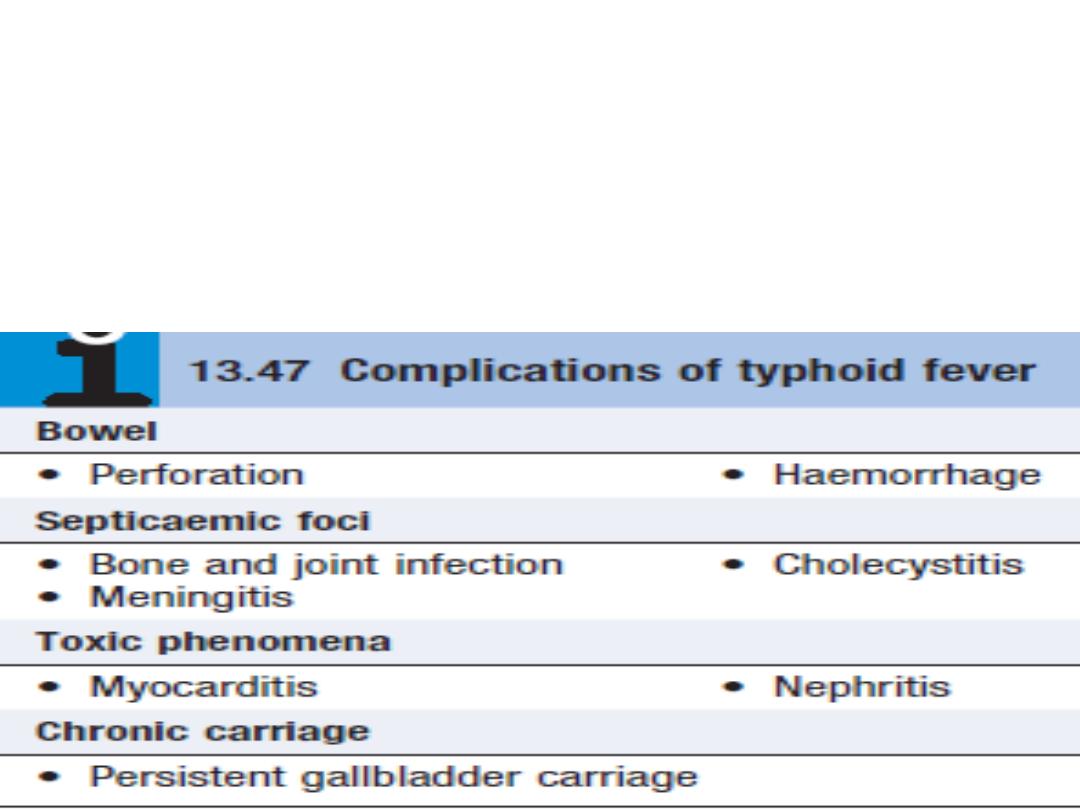
Complications
Hemorrhage from, or a perforation of, the ulcerated Peyer’s
patches may occur at the end of the second week or
during the third week of the illness.
Bone and joint infection is common in children with sickle-
cell disease.

Investigations
Note:
The definitive diagnosis of enteric fever requires the
isolation of S. Typhi or S. Paratyphi from blood, bone
marrow, rose spots, stool, or intestinal secretions.
• In the first week:
there is typically a leucopenia and blood
culture is the most important diagnostic method.
• In the second week and third weeks:
The faeces contain
the organism more frequently.
• Bone marrow cultures:
should be considered in suspected
cases with negative blood cultures.
• The serologic tests Widal test
is available. But this test is
not sensitive or specific to replace culture-based methods
for the diagnosis of enteric fever
• Polymerase chain reaction and DNA probe assays
to
detect S. Typhi in blood are being developed.

Management
The fluoroquinolones are the drugs of choice (e.g.
ciprofloxacin 500 mg twice daily) if the organism is
susceptible, but resistance is common
Extended-spectrum cephalosporins (ceftriaxone and
cefotaxime) are useful alternatives but have a slightly
increased treatment failure rate.
Azithromycin (500 mg daily) is an alternative when
fluoroquinolone resistance is present but has not been
validated in severe disease.
Treatment should be continued for 14 days.
Chronic carriers were formerly treated for 4 weeks with
ciprofloxacin. Cholecystectomy may be necessary.

Prevention:
• Improved sanitation and living conditions reduce
the incidence of typhoid.
• Travellers to countries where enteric infections are
endemic should be inoculated with one of the
three available typhoid vaccines (two inactivated
injectable and one oral live attenuated).

Thanks
