
SYSTEMIC LUPUS ERYTHEMATOSUS
TUCOM
Dep. of Medicine
5th year
Dr. Hasan I. Sultan
25/ 4/ 2019

Learning objectives:
1. Define Systemic lupus erythematosus (SLE).
2. Review the pathophysiology and causes of SLE.
3. Clarify the clinical features of SLE.
4. Outline the investigations of SLE.
5. Review the Revised American Rheumatism
Association diagnostic criteria for SLE.
6. Outline the treatment of SLE.
7. Show the prognosis of SLE.
Systemic lupus erythematosus (SLE)
SLE: Is a multisystemic autoimmune disease that results
from immune system mediated tissue damage that
involved the skin, joints, kidney, central nervous system,
cardiovascular system, serosal membranes, and the
hematologic and immune systems.
It is a rare disease with a prevalence that ranges from about
0.03% in Caucasians to 0.2% in Afro-Caribbeans. 90% of
affected patients are female and the peak age at onset is
between 20 and 30 years, with considerable increase
morbidity and a mortality.

Pathophysiology
The cause of SLE is incompletely understood, but there is a
form of interactions among genetic, immunological,
environmental, and hormonal factors.
Genetic factors:
There is a higher concordance in
monozygotic twins and the disease is strongly associated
with polymorphic variants at the HLA locus. In a few
instances, SLE is associated with inherited mutations in
complement components C1q, C2 and C4.
Immunological factors:
SLE may occur because of defects in
apoptosis or in the clearance of apoptotic cells, which
causes inappropriate exposure of intracellular antigens on
the cell surface, leading to polyclonal B- and T-cell
activation and autoantibody production.

Environmental factors:
that cause flares of lupus, such as UV
light and infections (particularly viruses), increase
oxidative stress and cause cell damage. Certain drugs,
including procainamide and hydralazine, can induce a
lupus-like syndrome, but the symptoms usually abate
after discontinuing use of the drug.
The female preponderance of SLE implies a role for
hormonal factors
in the disease.
Clinical features
1- General:
Symptoms such as fever, weight loss and mild
lymphadenopathy may occur during flares of disease activity,
whereas others such as fatigue and low-grade joint pains can
be constant and not particularly associated with active
inflammatory disease.
2- Arthritis:
Arthralgia is a common symptom, occurring in 90% of
patients. Tenosynovitis may also occur ,but clinically apparent
synovitis with joint swelling is rare. Joint erosions do not
occur.
3- Raynaud’s phenomenon:
is common in SLE along with
arthralgia or arthritis.
4- Renal involvement:
is one of the main determinants of
Prognosis. The typical renal lesion is a proliferative
glomerulonephritis, characterized by heavy hematuria,
proteinuria and casts on urine microscopy
.

5- Skin Rash:
is common in SLE and is classically precipitated by
exposure to UV light. Many distinct types occur:
•
The classic butterfly facial rash (up to 20% of patients). This
is erythematous, raised and painful or itchy, and occurs
over the cheeks with sparing of the nasolabial folds.
•
A discoid rash characterised by hyperkeratosis and
follicular plugging, with scarring alopecia if it occurs on the
scalp.
•
Diffuse, usually non-scarring alopecia, which may also
occur with active disease.
•
Urticarial eruptions.
•
Livedo reticularis which is also a feature of
antiphospholipid syndrome and can become frankly
vasculitic, if severe.
6- Cardiovascular:
The most common manifestation is
pericarditis. Myocarditis and Libman–Sacks endocarditis can
also occur.

7- Lung involvement:
is common and most frequently
manifests as pleurisy or pleural effusion.
8- Neurological:
More specific features of cerebral lupus
include visual hallucinations, chorea, organic psychosis,
transverse myelitis and lymphocytic meningitis.
9- Haematological:
Neutropenia, lymphopenia,
thrombocytopenia or haemolytic anaemia may occur, due
to antibody mediated destruction of peripheral blood
cells. The degree of lymphopenia is a good guide to
disease activity.
10- Gastrointestinal:
Mouth ulcers may occur and may or
may not be painful. Mesenteric vasculitis is a serious
complication, which can present with abdominal pain,
bowel infarction or perforation.

Butterfly (malar) rash of systemic lupus
erythematosus, sparing the nasolabial folds.
Discoid lupus presents with
red, inflamed, coin-shaped
patches of skin with a
scaling and crusty
appearance, most often on
the scalp, cheeks, and ears.
Hair loss may occur if the
lesions are on the scalp
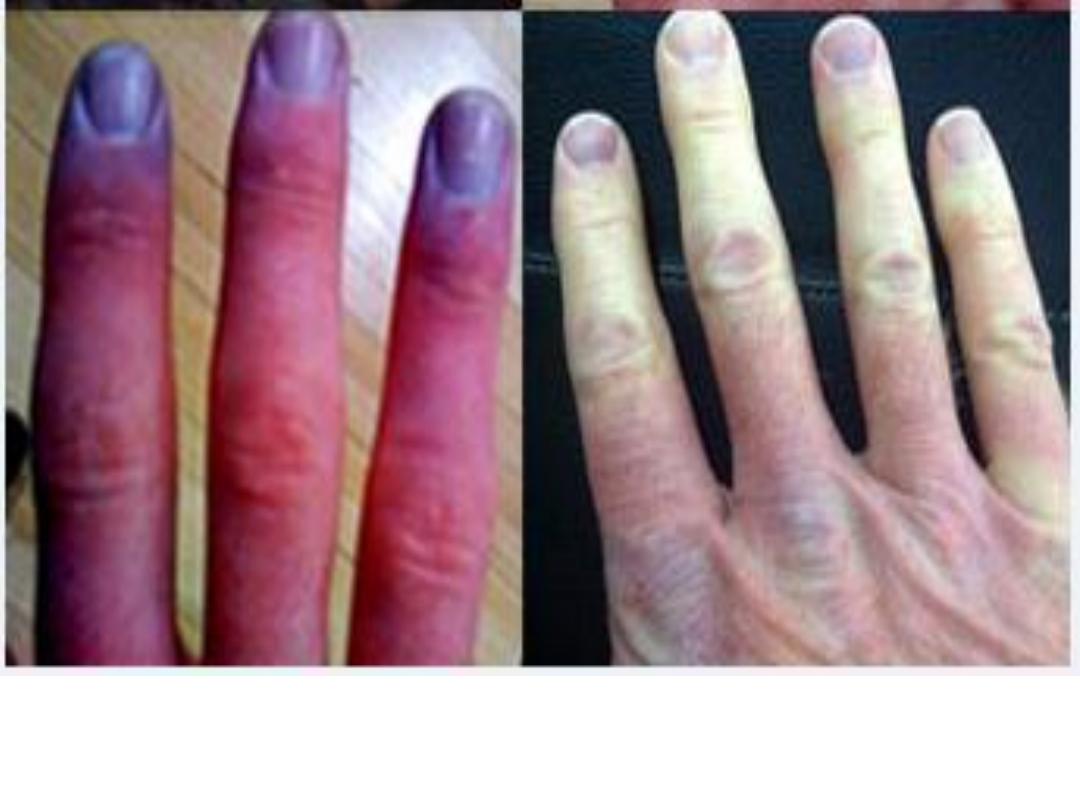
Raynaud phenomenon manifests as recurrent symmetrical vasospasm
of the fingers in response to cold exposure. characterized by pallor,
cyanosis then congestion (redness), which is painful.

Livedo reticularis (systemic lupus erythematosus
and anti-phospholipid syndrome).
Investigations
The diagnosis is based on a combination of clinical features
and laboratory abnormalities. To fulfil the classification criteria
for SLE, at least 4 of the 11 factors must be present or have
occurred in the past.
Patients should be screened for ANA and antibodies to
extractable nuclear antigens. Patients with active SLE almost
always test positive for ANA. Anti-dsDNA antibodies are
characteristic of severe active SLE. Autoantibodies associated
with SLE are shown in table in the next slide.
patients with active disease tend to have low levels of C3 and C4.
A raised ESR, leucopenia and lymphopenia are typical of active
SLE, along with anaemia, haemolytic anaemia and
thrombocytopenia.
Antibody
%
Clinical Utility
Antinuclear
antibodies
98
Best screening test; repeated negative tests
make SLE unlikely
Anti-dsDNA
70
High titers are SLE-specific and correlate with
disease activity, nephritis and vasculitis
Anti-Sm
25
Specific for SLE; no definite clinical
correlations
Anti-Ro (SS-A)
30
Not specific for SLE; associated with sicca
syndrome, subacute cutaneous lupus, and
neonatal lupus with congenital heart block
Antihistone
70
More frequent in drug-induced lupus than in
SLE
Antiphospholi
pid
50
for cardiolipin, predisposes to clotting, fetal
loss and thrombocytopenia
Autoantibodies in Systemic Lupus Erythematosus (SLE)
Revised American Rheumatism Association criteria for
systemic lupus erythematosus
1- Malar rash:
Fixed erythema, flat or raised, sparing the
nasolabial folds
2- Discoid rash:
Erythematous raised patches with adherent
keratotic scarring and follicular plugging
3- Photosensitivity Rash:
due to unusual reaction to sunlight
4- Oral ulcers:
Oral or nasopharyngeal ulceration, which may
be painless
5- Arthritis:
Non-erosive, involving two or more peripheral
joints
6- Serositis:
Pleuritis (history of pleuritic pain or rub, or
pleural effusion) or pericarditis (rub, ECG evidence or
effusion)

7- Renal disorder:
Persistent proteinuria > 0.5 g/day or
cellular casts (red cell, granular or tubular)
8- Neurological disorder:
Seizures or psychosis, in the
absence of provoking drugs or metabolic derangement
9- Haematological disorder:
Haemolytic anaemia or
leucopenia* (< 4 × 109/L) or lymphopenia* (< 1 × 109/L) or
thrombocytopenia* (< 100 × 109/L) in the absence of
offending drugs
10- Immunological disorder:
Anti-DNA antibodies in
abnormal titre or presence of antibody to Sm antigen or
positive antiphospholipid antibodies
11- ANA disorder:
Abnormal titre of ANA by
immunofluorescence
A person has SLE if any 4 out of these 11 features are present serially
or simultaneously.
*On two separate occasions.
Management
The therapeutic goals are to educate the patient about the
nature of the illness, to control symptoms and to prevent
organ damage.
Patients should be advised to avoid sun and UV light
exposure and to employ sun blocks cream (sun protection
factor 50)= which blocks an estimated 98 percent of UV
rays.
1- Mild to moderate disease:
Patients with mild disease
restricted to skin and joints can sometimes be managed
with analgesics, NSAID and hydroxychloroquine (200–400
mg daily). Frequently, however, corticosteroids are also
necessary (prednisolone 5–20 mg/day), often in
combination with immunosuppressants such as
methotrexate, azathioprine or mycophenolate mofetil
(MMF).

• The monoclonal antibody belimumab (targets the β-cell
growth factor) recently been shown to be effective in
patients with active SLE who have responded
inadequately to standard therapy.
2- Life-threatening disease:
High-dose corticosteroids and
immunosuppressants are required for the treatment of
renal, CNS and cardiac involvement. A commonly used
regimen is pulse methylprednisolone (10 mg/kg IV),
coupled with cyclophosphamide (15 mg/kg IV), repeated
at 2–3-weekly intervals for six cycles.
Mycophenolate mofetil has been used successfully in
combination with high-dose steroids for renal
involvement in SLE, with results equivalent to those of
pulse cyclophosphamide but fewer adverse effects.

Belimumab in combination with standard therapy significantly
decreases disease activity in SLE patients and is safe and well
tolerated.
3- Maintenance therapy:
Oral prednisolone 10–15 mg/day,
azathioprine (2–2.5 mg/kg/day), methotrexate (10–25
mg/week) or MMF (2–3 g/day) should also be prescribed. The
long-term aim is to continue the lowest dose of glucocorticoid
and immunosuppressant to maintain remission.
Cardiovascular risk factors, such as hypertension and
hyperlipidaemia, should be controlled and patients should be
advised to stop smoking.
Patients with SLE and the antiphospholipid antibody syndrome,
who have had previous thrombosis, require life-long warfarin
therapy.
SLE patients are at risk of osteoporosis and hypovitaminosis D,
and should be screened with biochemistry and DXA scanning
accordingly.

Prognosis
Survival in patients with SLE in the United States is
approximately 95% at 5 years, 90% at 10 years, and 78%
at 20 years.
Poor prognosis (~50% mortality in 10 years): renal
impairment, hypertension, nephrotic syndrome, anemia,
hypoalbuminemia, hypocomplementemia and male sex.
Drug-Induced Lupus
This is a syndrome of positive ANA associated with symptoms
such as fever, malaise, arthritis or intense arthralgias/
myalgias, serositis, and/or rash.
Has less female predilection than SLE, rarely involves kidneys or
brain, is rarely associated with anti-dsDNA, is commonly
associated with antibodies to histones, and usually resolves
over several weeks after discontinuation of the offending
medication.
The most frequent are the antiarrhythmics procainamide,
disopyramide, and propafenone; the antihypertensive
hydralazine; several angiotensin-converting enzyme inhibitors
and beta blockers; the antithyroid propylthiouracil; the
antipsychotics chlorpromazine and lithium; the
anticonvulsants carbamazepine and phenytoin; the antibiotics
isoniazid

Thanks
