
BRUCELLOSIS
Brucellosis is an enzootic infection (i.e. endemic in
animals). Although six species of Brucella are known,
only four are important to humans: B. melitensis
(goats, sheep and camels), B. abortus (cattle), B. suis
(pigs) and B. canis (dogs).

B. melitensis is enzootic in the Middle East, Africa,
India, Central Asia and South America. B. abortus is
found in Africa, Asia and South America, and B. suis in
South Asia. B. melitensis causes the most severe
disease; B. suis is often associated with abscess
formation.

Infected animals may excrete brucellae in their milk
for long periods of time and human infection is
acquired by ingesting contaminated milk, cheese,
yoghurt and butter. Uncooked meat and offal may also
spread infection. Animal urine, faeces, vaginal
discharge and uterine products may act as sources of
infection through abraded skin or via splashes and
aerosols to the respiratory tract and conjunctiva.

Clinical features
Brucellae are intracellular organisms that can survive
for long periods within the reticulo-endothelial
system. This explains many of the features of clinical
brucellosis, including the chronicity of the disease and
the tendency to relapse even after adequate
antimicrobial therapy.

Acute illness is characterised by a high swinging
temperature, rigors, sweating, lethargy, headache, and
joint and muscle pains. Occasionally, there is delirium,
abdominal pain and constipation. Physical signs are
non-specific: for example, a palpable spleen or
enlarged lymph nodes. Enlargement of the spleen may
lead to hypersplenism and thrombocytopenia.
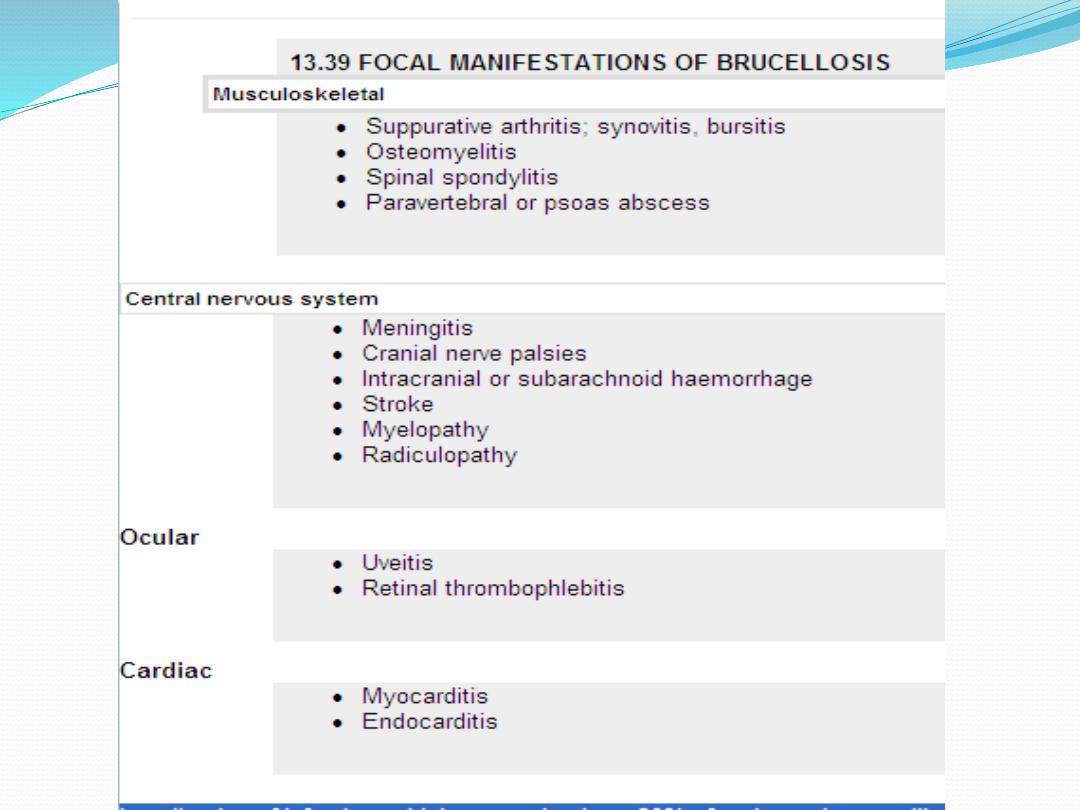
Localisation of infection, which occurs in about 30% of
patients, is more likely if diagnosis and treatment are
delayed.

Diagnosis
Definitive diagnosis of brucellosis depends on the
isolation of the organism. Blood cultures are positive
in 75-80% of infections caused by B. melitensis and
50% of those caused by B. abortus. The non-
radiometric 'Bactec' system gives a good isolation rate,
but if brucellosis is suspected, prolonged incubation
and blind subcultures are recommended. Bone
marrow culture should not be used routinely but may
increase the diagnostic yield, particularly if antibiotics
have been given before specimens are taken. CSF
culture in neurobrucellosis is positive in about 30% of
cases.
World-wide, the serum agglutination test is the
serological technique most commonly employed to
detect brucellosis. The test has many pitfalls and good
quality control is essential. Agglutination should be
carried out to a high dilution (at least 1/640) to avoid
the prozone phenomenon whereby non-agglutinating
IgG and IgA molecules completely block the
agglutinating reaction. Significant agglutination titres
may persist for months or years after recovery and in
endemic areas a single titre of 1/320 or a fourfold rise in
titre is needed to support a diagnosis of acute
infection. The test usually takes several weeks to
become positive but should eventually detect 95% of
acute infections. The pre-treatment of serum with 2-
mercaptoethanol helps to distinguish between IgG
and IgM responses.

The enzyme-linked immunosorbent assay (ELISA) also
identifies IgM and IgG antibodies; IgM decreases
rapidly within the first few months of illness. Specialist
laboratory techniques including the use of the anti-
human globulin (Coombs) test may be necessary to
distinguish chronic disease from past inactive
infection.

Management
Aminoglycosides show synergistic activity with
tetracyclines when used against brucellae. Standard
therapy therefore consists of doxycycline 100 mg 12-
hourly for 6 weeks, with streptomycin 1 g i.m. daily for
the first 2 weeks. The relapse rate with this treatment
is about 5%. An alternative oral regimen consists of
doxycycline 100 mg 12-hourly plus rifampicin 900 mg
(15 mg/kg) daily for 6 weeks, but failure and relapse
rates are higher, particularly with spondylitis.
Rifampicin may antagonise doxycycline activity by
reducing serum levels through enzyme induction.

Chronic illness should be treated for a minimum of 3
months and many authorities would extend this to 6
months, depending upon the condition of the patient
and the result of sequential serological tests. The
optimum therapy for neurobrucellosis is unknown,
and there is no current agreement on the combination
or number of drugs to use. Treatment should continue
for at least 3 months, and longer if CSF pleocytosis
persists.

THANK YOU FOR
LISTENING
