
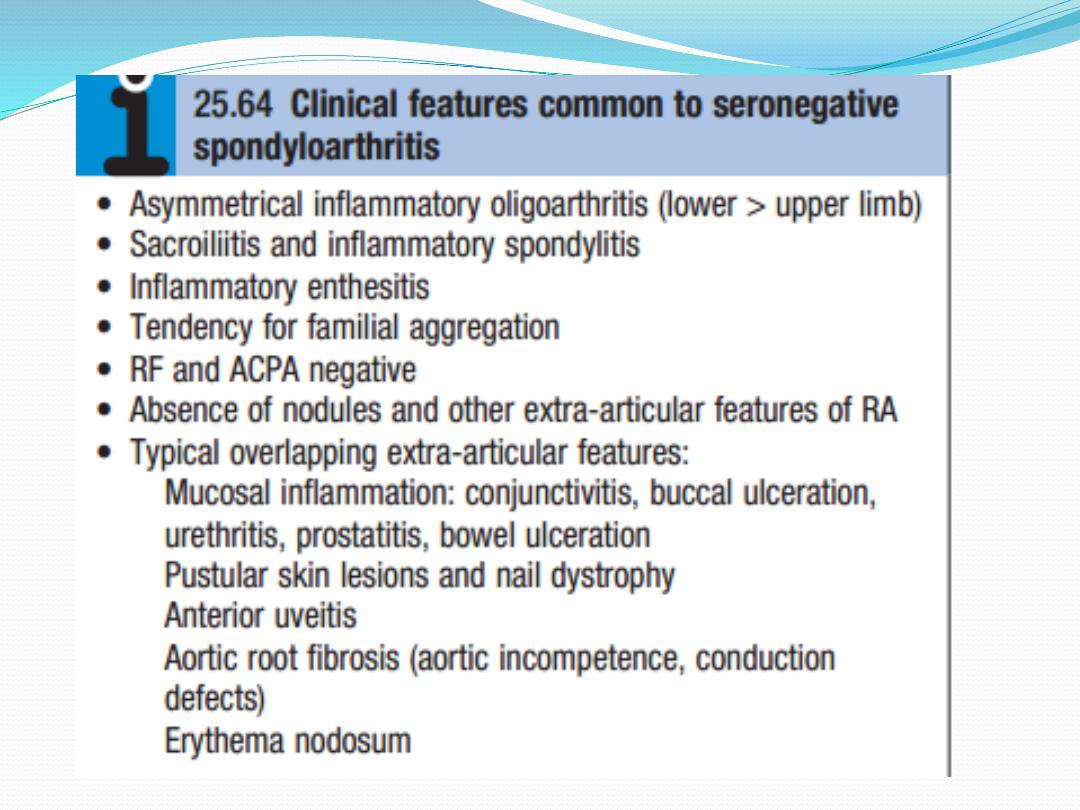
SERONEGATIVE
SPONDYLOARTHROPATHIES
These comprise a group of related inflammatory joint
diseases, which show considerable overlap in their
clinical features and a shared immunogenetic
association with the HLAB27 antigen . They include:
• ankylosing spondylitis
• axial spondyloarthritis
• reactive arthritis, including Reiter’s syndrome
• psoriatic arthritis
• arthropathy associated with inflammatory bowel
disease.

There is a striking association with carriage of the
HLAB27 allele, particularly for ankylosing spondylitis
(>95%) and reactive arthritis (90%), and especially
associated with sacroiliitis, uveitis or balanitis.
Understanding of the cause is incomplete but an
aberrant response to infection is thought to be
involved in genetically predisposed individuals. In
some situations, a triggering organism can be
identified, as in reactive arthritis following bacterial
dysentery or chlamydial urethritis, but in others the
environmental trigger remains obscure. Familial
clustering not only is common to the specific
condition occurring in the proband, but also may
extend to other diseases in the seronegative
spondyloarthopathy group.

Ankylosing spondylitis
Ankylosing spondylitis (AS) is characterised by a chronic
inflammatory arthritis predominantly affecting the
sacro iliac joints and spine, which can progress to bony
fusion of the spine. The onset is typically between the
ages of 20 and 30, with a male preponderance of about
3 : 1. In Europe, more than 90% of those affected are
HLAB27positive. The overall prevalence is less than
0.5% in most populations. Over 75% of patients are able
to remain in employment and enjoy a good quality of
life. Even if severe ankylosis develops, functional limita
tion may not be marked as long as the spine is fused in
an erect posture.
Pathophysiology
Ankylosing spondylitis is thought to arise from an as
yet illdefined interaction between environmental
pathogens and the host immune system in genetically
susceptible individuals. Increased faecal carriage of
Klebsiella aerogenes occurs in patients with
established AS and may relate to exacerbation of both
joint and eye disease. Wider alterations in the human
gut microbial environment are increasingly
implicated, which could lead to increased levels of
circulating cytokines such as IL23 that can activate
enthesial or synovial T cells.
The HLAB27 molecule itself is implicated through its
antigen presenting function (it is a class I MHC
molecule) or because of its propensity to form
homodimers that activate leucocytes. HLAB27
molecules may also misfold, causing increased
endoplasmic reticulum stress. This could lead to
inflammatory cytokine release by macrophages and
dendritic cells, thus triggering inflammatory disease.

Clinical features
The cardinal feature is low back pain and early morning
stiffness with radiation to the buttocks or posterior
thighs. Symptoms are exacerbated by inactivity and
relieved by movement. The disease tends to ascend
slowly, ultimately involving the whole spine, although
some patients present with symptoms of the thoracic
or cervical spine. As the disease progresses, the spine
becomes increasingly rigid as ankylosis occurs.
Secondary osteoporosis of the vertebral bodies frequently
occurs, leading to an increased risk of vertebral fracture.

Early physical signs include a reduced range of lumbar
spine movements in all directions and pain on
sacroiliac stressing. As the disease progresses, stiffness
increases throughout the spine and chest expansion
becomes restricted. Spinal fusion varies in its extent
and in most cases does not cause a gross flexion
deformity, but a few patients develop marked kyphosis
of the dorsal and cervical spine that may interfere with
forward vision.
This may prove incapacitating, especially when
associated with fixed flexion contractures of hips or
knees. Pleuritic chest pain aggravated by breathing is
common and results from costovertebral joint
involvement. Plantar fasciitis, Achilles tendinitis and
tenderness over bony prominences such as the iliac
crest and greater trochanter may all occur, reflecting
inflammation at the sites of tendon insertions
(enthesitis).

Up to 40% of patients also have peripheral arthritis.
This is usually asymmetrical, affecting large joints such
as the hips, knees, ankles and shoulders. In about 10%
of cases, involvement of a peripheral joint may
antedate spinal symptoms, and in a further 10%,
symptoms begin in childhood, as in the syndrome of
oligoarticular juvenile idiopathic arthritis.

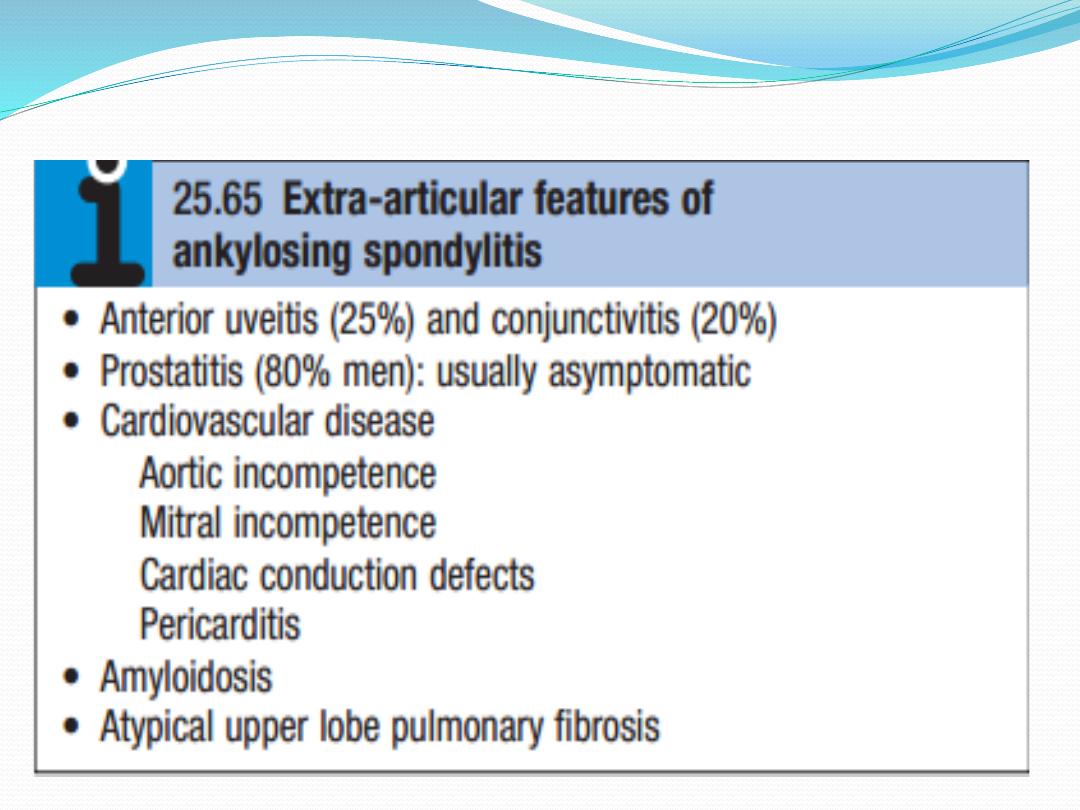
Fatigue is a major complaint and may result from both
chronic interruption of sleep due to pain, and chronic
systemic inflammation with direct effects of
inflammatory cytokines on the brain. Acute anterior
uveitis is the most common extraarticular feature,
which occasionally precedes joint disease. Other extra-
articular features are occasionally observed but are
rare.
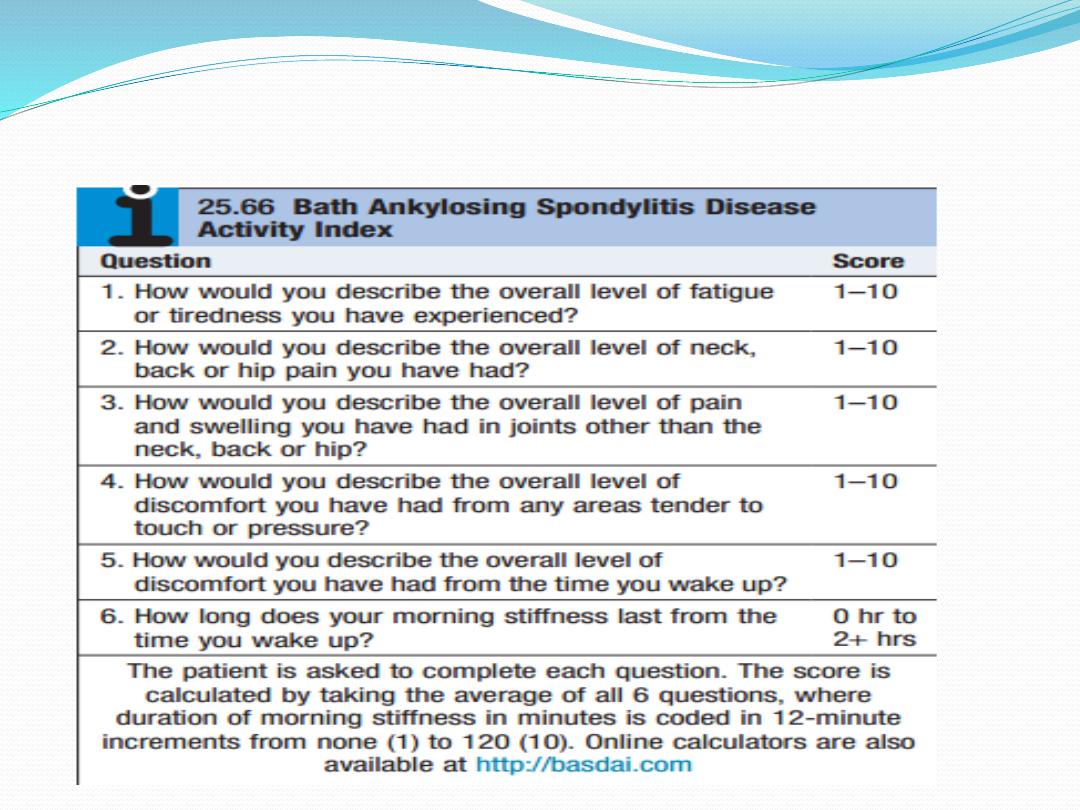
This is important in assessing eligibility for biological treatment.

Investigations
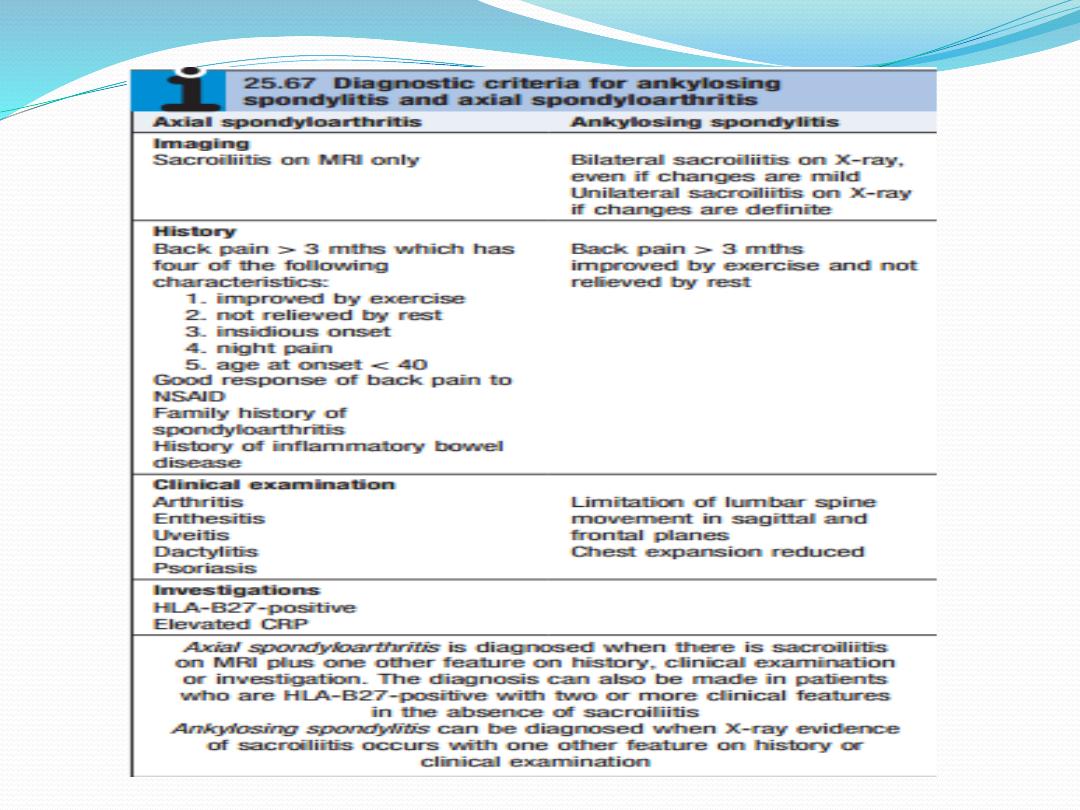
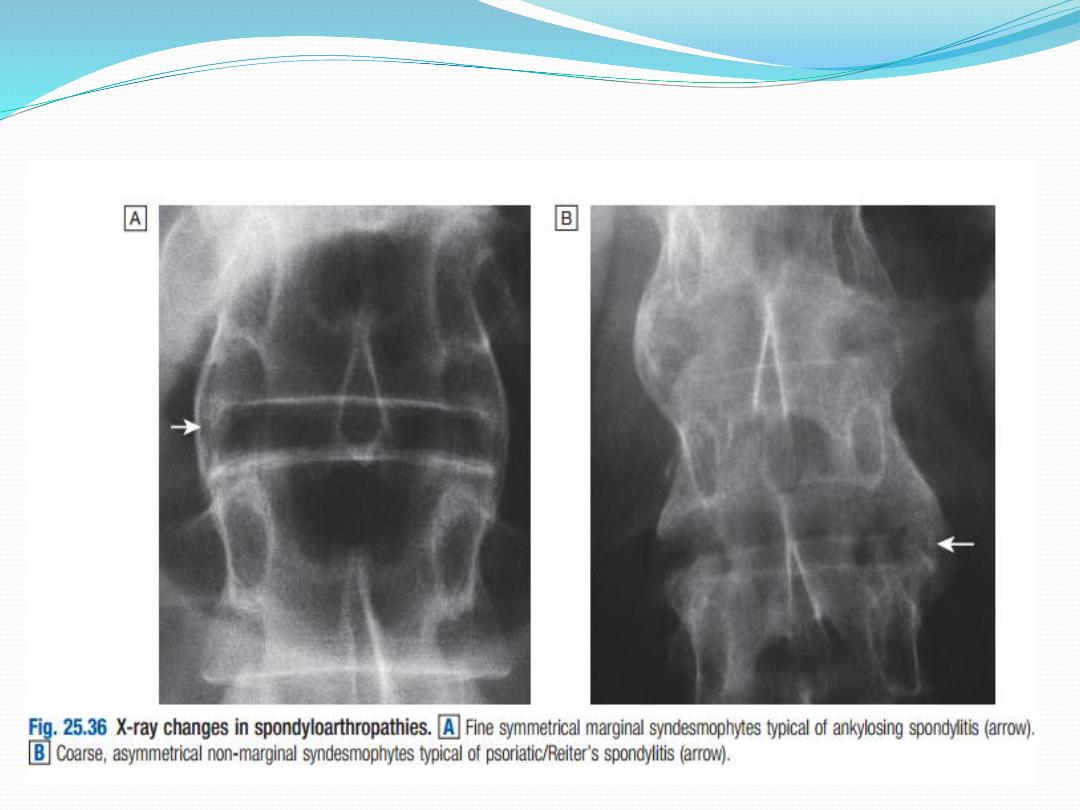
In established AS, radiographs of the sacroiliac joint
show irregularity and loss of cortical margins,
widening of the joint space and subsequently sclerosis,
joint space narrowing and fusion. Lateral
thoracolumbar spine Xrays may show anterior
‘squaring’ of vertebrae due to erosion and sclerosis of
the anterior corners and periostitis of the waist.
Bridging syndesmophytes may also be seen. These are
areas of calcification that follow the outermost fibres
of the annulus.

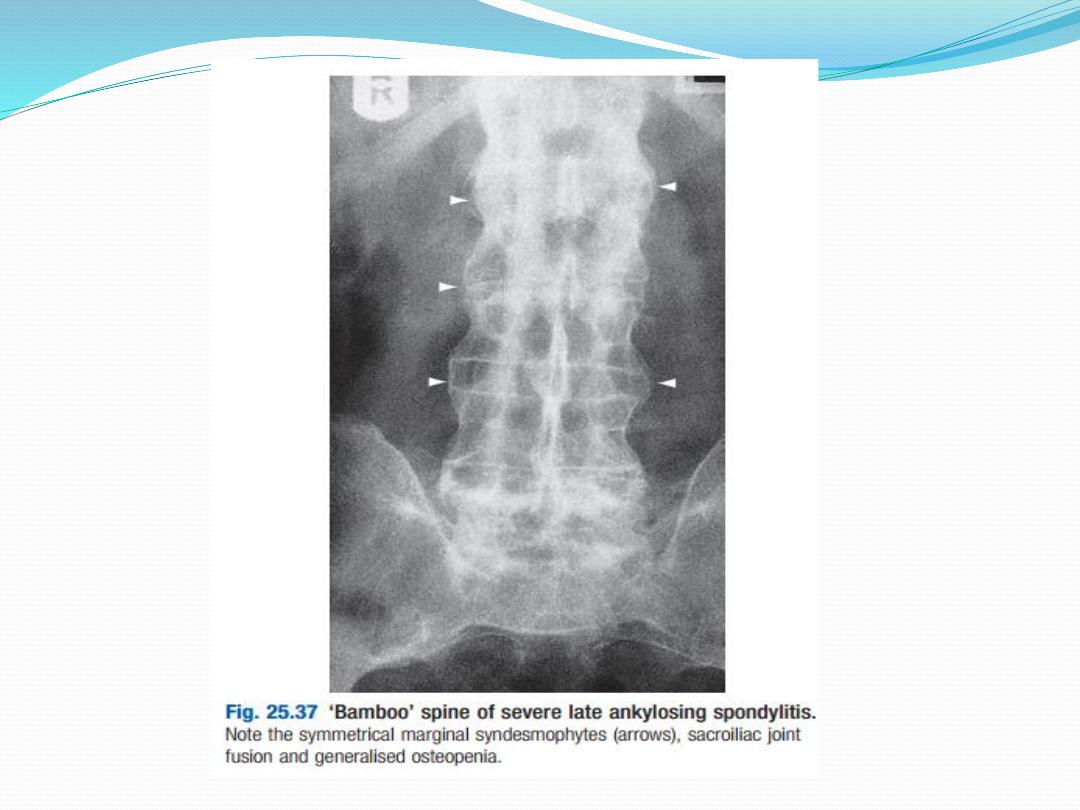
In advanced disease, ossification of
the anterior longitudinal ligament
and facet joint fusion may also be
visible. The combination of these
features may result in the typical
‘bamboo’ spine.

Erosive changes may be seen in the symphysis pubis,
the ischial tuberosities and peripheral joints.
Osteoporosis and atlantoaxial dislocation can occur as
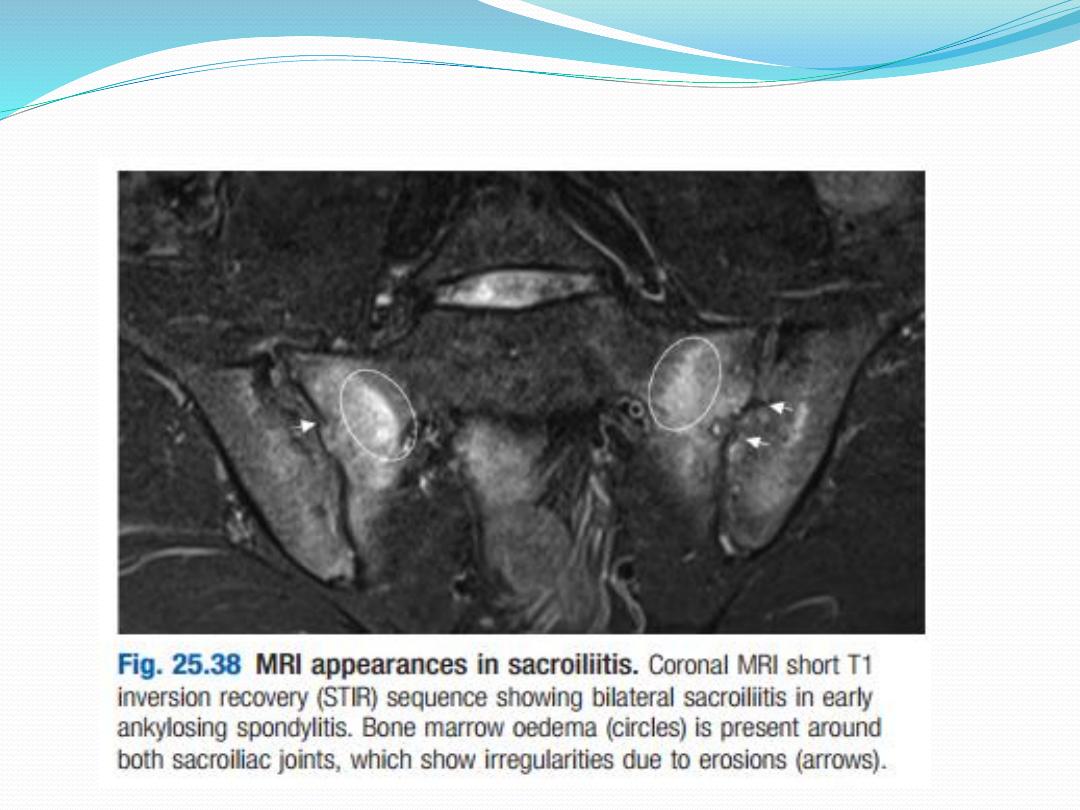
late features. Patients with early disease can have
normal Xrays, and if clinical suspicion is high, MRI
should be performed. This is much more sensitive for
detection of early sacroiliitis than Xray and can also
detect inflammatory changes in the lumbar spine.

The ESR and CRP are usually raised in active disease
but may be normal. Testing for HLAB27 can be
helpful, especially in patients with back pain
suggestive of an inflammatory cause, when other
investigations have yielded equivocal results.
Autoantibodies such as RF, ACPA and ANA are
negative.

Management
The aims of management are to relieve pain and stiff
ness, maintain a maximal range of skeletal mobility
and avoid the development of deformities. Education
and appropriate physical activity are the cornerstones
of management. Early in the disease, patients should
be taught to perform daily back extension exercises,
including a morning ‘warmup’ routine, and to
punctuate prolonged periods of inactivity with regular
breaks.

Swimming is ideal exercise. Poor posture must be
avoided. NSAIDs and analgesics are often effective in
relieving symptoms and may alter the underlying
course of the disease. A longacting NSAID at night is
helpful for alleviation of morning stiffness. Peripheral
arthritis can be treated with methotrexate or
sulfasalazine, but these drugs have no effect on axial
disease.

AntiTNF therapy should be considered in patients who
are inadequately controlled on standard therapy with a
BASDAI score of ≥4.0 and a spinal pain score of ≥4.0.
AntiTNF therapy frequently improves symptoms but
has not been shown to prevent ankylosis or alter
natural history of the disease. Other biological
interventions using agents developed for RA have been
disappointing, suggesting fundamental differences in
disease pathogenesis.

Local corticosteroid injections can be useful for
persistent plantar fasciitis, other enthesopathies and
peripheral arthritis. Oral corticosteroids may be
required for acute uveitis but do not help spinal
disease. Severe hip, knee or shoulder restriction may
require surgery. Total hip arthroplasty has largely
removed the need for difficult spinal surgery in those
with advanced deformity.
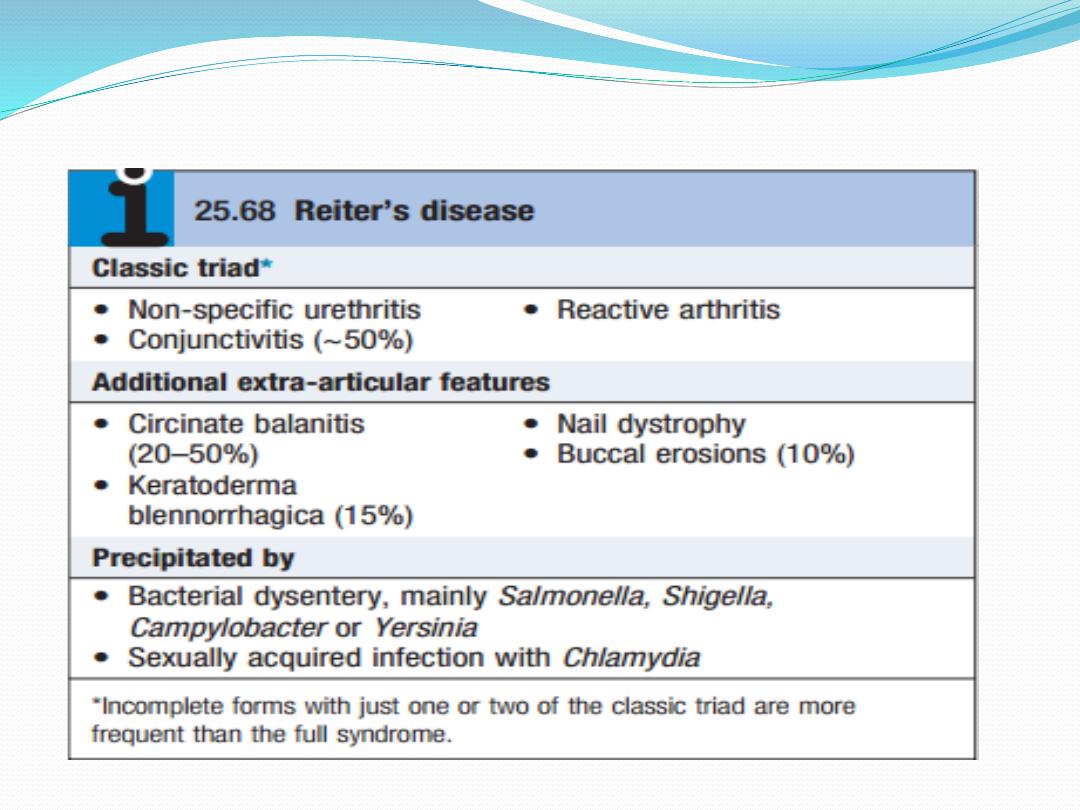
Reactive arthritis
Reactive arthritis (previously known as Reiter’s
disease)
is predominantly a disease of young men, with a male
preponderance of 15 : 1. It is the most common cause
of inflammatory arthritis in men aged 16–35 but may
occur at any age. Between 1 and 2% of patients with
nonspecific urethritis seen at genitourinary medicine
clinics have reactive arthritis . Following an epidemic
of Shigella dysentery, 20% of HLAB27positive
men developed reactive arthritis.

Clinical features
The onset is typically acute, with an inflammatory oligo
arthritis that is asymmetrical and targets lower limb joints,
such as the knees, ankles, midtarsal and MTP joints. It
occasionally presents with single joint involvement and no
clear history of an infectious trigger. There may be
considerable systemic disturbance, with fever and weight
loss. Achilles tendinitis or plantar fasciitis may also be
present. The first attack of arthritis is usually selflimiting,
but recurrent or chronic arthritis develops in more than
60% of patients, and about 10% still have active disease 20
years after the initial presentation. Low back pain and
stiffness are common and 15–20% of patients develop
sacroiliitis. Spondylitis, chronic erosive arthritis, recurrent
acute arthritis and uveitis are the major causes of longterm
morbidity.

Several extraarticular features may occur. Circinate
balanitis starts as vesicles on the coronal margin of the
prepuce and glans penis, later rupturing to form superficial
erosions with minimal surrounding erythema, some
coalescing to give a circular pattern. Lesions are often
painless and may escape notice. Keratoderma
blennorrhagica begins as discrete waxy, yellowbrown
vesicopapules with desquamating margins, occasionally
coalescing to form large crustyplaques. The palms and
soles are particularly affected but spread may occur to the
scrotum, scalp and trunk.
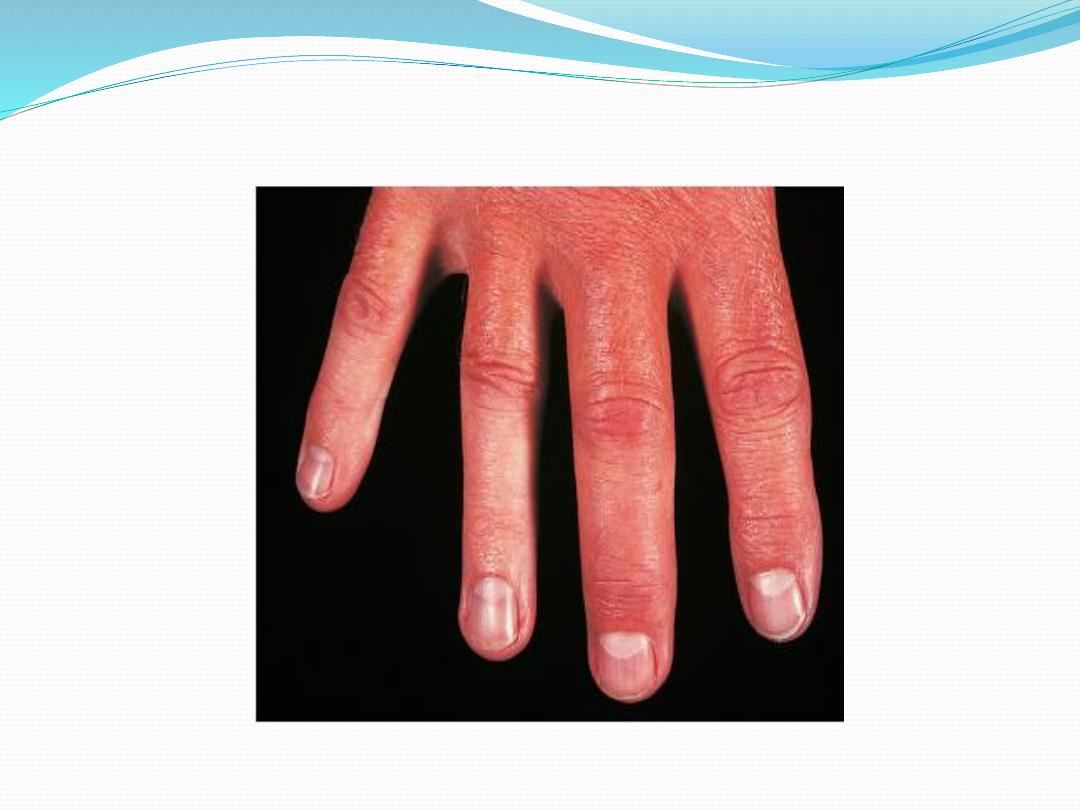
These lesions are indistinguishable from pustular
psoriasis. Nail dystrophy with subungual hyperkeratosis is
common and indistinguishable from psoriatic nail
dystrophy.

Mouth ulcers manifest as shallow red painless
patches on tongue, palate, buccal mucosa and lips,
lasting only a few days. Conjunctivitis may accompany
the first acute episode. Uveitis is rare with the first
attack but occurs in 30% of patients with recurring or
chronic arthritis.
Other complications are rare but include aortic
incompetence, conduction defects, pleuropericarditis,
peripheral neuropathy, seizures and
meningoencephalitis.
Investigations
The diagnosis is usually made clinically but joint aspiration
may be required to exclude crystal arthritis and articular
infection. Synovial fluid is leucocyte rich and may contain
multinucleated macrophages (Reiter’s cells). ESR and CRP
are raised during an acute attack.
Urethritis may be confirmed in the ‘two glass test’ by
demonstration of mucoid threads in the first void
specimen that clear in the second. High vaginal swabs may
reveal Chlamydia on culture. Except for post Salmonella
arthritis, stool cultures are usually negative by the time the
arthritis presents, but serum agglutinin tests may help
confirm previous dysentery. RF, ACPA and ANA are
negative.

In chronic or recurrent disease, Xrays show
periarticular osteoporosis, joint space narrowing and
proliferative erosions. Another characteristic feature is
periostitis, especially of metatarsals, phalanges and
pelvis, and large, ‘fluffy’ calcaneal spurs. In contrast to
AS, radiographic sacroiliitis is often asymmetrical and
sometimes unilateral, and syndesmophytes are
predominantly coarse and asymmetrical, often
extending beyond the contours of the annulus (‘non-
marginal’) . Xray changes in the peripheral joints and
spine are identical to those in psoriasis.

Management
The acute attack should be treated with rest, oral
NSAIDs and analgesics. Intraarticular steroids may be
required in patients with severe synovitis. Nonspecific
chlamydial urethritis is usually treated with a short
course of doxycycline or a single dose of azithromycin,
and this may reduce the frequency of arthritis in
sexually acquired cases. Treatment with DMARDs
should be considered for patients with persistent
marked symptoms, recurrent arthritis or severe
keratoderma blennorrhagica. Anterior uveitis is a
medical emergency requiring topical, subconjunctival
or systemic corticosteroids.

Psoriatic arthritis
Psoriatic arthritis (PsA) occurs in 7–20% of patients
with psoriasis and in up to 0.6% of the general
population. The onset is usually between 25 and 40
years of age. Most patients (70%) have preexisting
psoriasis but in 20% the arthritis predates the
occurrence of skin disease. Occasionally, the arthritis
and psoriasis develop synchronously.

Clinical features
The presentation is with pain and swelling affecting
the joints and entheses. Several patterns of joint
involvement are recognised but the course is generally
one of intermittent exacerbation followed by varying
periods of complete or nearcomplete remission.
Destructive arthritis and disability are uncommon,
except in the case of arthritis mutilans.

Asymmetrical inflammatory oligoarthritis
affects
about 40% of patients and often presents abruptly
with a combination of synovitis and adjacent
periarticular inflammation. This occurs most
characteristically in the hands and feet, when synovitis
of a finger or toe is coupled with tenosynovitis,
enthesitis and inflammation of intervening tissue to
give a ‘sausage digit’ or dactylitis . Large joints, such as
the knee and ankle, may also be involved, sometimes
with very large effusions.

Symmetrical polyarthritis
occurs in about 25% of
cases. It predominates in women and may strongly
resemble RA, with symmetrical involvement of small
and large joints in both upper and lower limbs.
Nodules and other extraarticular features of RA are
absent and arthritis is generally less extensive and
more benign. Much of the hand deformity often
results from tenosynovitis and soft tissue contractures.

Distal IPJ arthritisis
an uncommon but characteristic
pattern affecting men more often than women. It
targets finger DIP joints and surrounding periarticular
tissues, almost invariably with accompanying nail
dystrophy


Psoriatic spondylitis
presents a similar clinical picture
to AS but with less severe involvement. It may occur
alone or with any of the other clinical patterns
described above and is typically unilateral or
asymmetric in severity.

Arthritis mutilansis
a deforming erosive arthritis
targeting the fingers and toes that occurs in 5% of
cases of PsA. Prominent cartilage and bone
destruction results in marked instability. The encasing
skin appears invaginated and ‘telescoped’ (‘main en
lorgnette’) and the finger can be pulled back to its
original length.

Nail changes include pitting, onycholysis, subungual
hyperkeratosis and horizontal ridging. They are found
in 85% of those with PsA and only 30% of those with
uncomplicated psoriasis, and can occur in the absence
of skin disease. The characteristic rash of psoriasis
may be widespread, or confined to the scalp, natal
cleft and umbilicus, where it is easily overlooked.
Conjunctivitis can occur, whereas uveitis is mainly con
fined to HLAB27positive individuals with sacroiliitis
and spondylitis.

Investigations
The diagnosis is made on clinical grounds. Autoantibodies
are generally negative and acute phase reactants, such as
ESR and CRP, are raised in only a proportion of patients
with active disease. Xrays may be normal or show erosive
change with joint space narrowing. Features that favour
PsA over RA include the characteristic distribution of
proliferative erosions with marked new bone formation,
absence of periarticular osteoporosis and osteosclerosis.
Imaging of the axial skeleton often reveals features similar
to those in chronic reactive arthritis, with coarse,
asymmetrical, nonmarginal syndesmophytes and
asymmetrical sacroiliitis. MRI and ultrasound with power
Doppler are increasingly employed to detect synovial
inflammation and inflammation at the entheses.

Management
Therapy with NSAID and analgesics may be sufficient
to control symptoms in mild disease. Intraarticular
steroid injections can control synovitis in problem
joints. Splints and prolonged rest should be avoided
because of the tendency to fibrous and bony ankylosis.
Patients with spondylitis should be prescribed the
same exercise and posture regime as in AS.

Therapy with DMARDs should be considered for persistent
synovitis unresponsive to conservative treatment.
Methotrexate is the drug of first choice since it may also
help skin psoriasis, but other DMARDs may also be
effective, including sulfasalazine, ciclosporin and
leflunomide. DMARD monitoring should take place with
particular attention to liver function since abnormalities
are common in PsA. Hydroxychloroquine is generally
avoided, as it can cause exfoliative skin reactions. AntiTNF
treatment should be considered for patients with active
synovitis who respond inadequately to standard DMARDs.
This is effective for both PsA and psoriasis. Other
biological treatments, such as ustekinumab, are emerging,
which target the IL12/23 receptor. Ustekinumab is highly
effective in the treatment of psoriatic skin disease and is
often effective in PsA.

The retinoid acitretin is effective for skin lesions and,
anecdotally, may also help arthritis, but it is
teratogenic so must be avoided in young women. It
also causes mucocutaneous side effects,
hyperlipidaemia, myalgias and extraspinal
calcification. Photochemotherapy with
methoxypsoralen and longwave ultraviolet light
(psoralen +UVA, PUVA) is primarily used for skin
disease, but can also help those with synchronous
exacerbations of inflammatory arthritis.

Enteropathic arthritis
An acute inflammatory oligoarthritis occurs in around
10% of patients with ulcerative colitis and 20% of
those
with Crohn’s disease. It predominantly affects the
large
lower limb joints (knees, ankles, hips) but wrists and
small joints of the hands and feet can also be involved.
The arthritis usually coincides with exacerbations of
the underlying bowel disease, and sometimes is
accompanied by aphthous mouth ulcers, iritis and
erythema nodosum.

It improves with effective treatment of the bowel
disease, and can be cured by total colectomy in
patients with ulcerative colitis. Patients with
inflammatory bowel disease may also develop
sacroiliitis (16%) and AS (6%), which are clinically and
radiologically identical to classic AS. These can
predate or follow the onset of bowel disease and there
is no correlation between activity of the spondylitis
and bowel disease.
The arthritis often remits with treatment of the bowel
disease but DMARD and biological treatment is
occasionally required.

THANK YOU FOR
LISTENING
