
Endometriosis
What is endometriosis?
Endometriosis is defined as the presence of
endometrial-like ssue outside the uterus .Endometriosis
triggers a chronic inflammatory reac on resul ng in
pain and adhesions.
What causes endometriosis?
The cause of endometriosis remains unknown. There are
several theories, but none of them has been en rely
proven. The most accepted theory is centred on the
so-called retrograde menstrua on. During menstrua on,
pieces of endometrium arrive in the abdominal cavity
through the Fallopian tubes, adhere to the peritoneal
lining and develop into endometrio c lesions. The
hormone estrogen is crucial in this process. Subsequently,
most of the current treatments for endometriosis
a empt to lower estrogen produc on in a woman’s body
in order to relieve her of symptoms.

It has been argued that endometriosis is a gene c
disease, since some families show more pa ents with
endometriosis compared to other families. Other
sugges ons are an immune response triggering
inflamma on
Diagnosis;
What are the symptoms of endometriosis?
The classical symptoms of endometriosis are: -
Dysmenorrhea or painful menstrua on
- Nonmenstrual pelvic pain or pain occurring when a
woman is not menstrua ng.
- Dyspareunia or painful intercourse
- Infer lity
- Fa gue
- Cyclical intes nal complaints: periodic bloa ng,
diarrhoea or cons pa on
- Cyclical dyschezia, painful or difficult defeca on.

- Cyclical dysuria, painful urina on - Cyclical hematuria,
or the presence of blood in the urine
- Cyclical rectal bleeding
Cyclical symptoms are symptoms that develop a few days
before a woman’s menstrua on and disappear a few days
a er her menstrua on has stopped, or symptoms that
occur only during the menstrua on. The symptoms
reappear the next month, following the woman’s
menstrual cycle.
Examina on Most women with endometriosis exhibit no
abnormality or minimal findings on physical examina on.
Clues to the diagnosis include uterine, adnexal or pouch
of Douglas tenderness, a tender fixed adnexal mass or a
fixed retroverted uterus. The most sugges ve sign is
tenderness and nodularity in the pouch of Douglas or
uterosacral ligaments. In any pelvic examina on where
endometriosis is suspected, a conscious effort should be
made to palpate this area by running the vaginal fingers
behind the cervix and onto the pouch of Douglas. The
palpa on should then con nue laterally to define the

bordering uterosacral ligaments. Nodularity in this area is
highly sugges ve of endometriosis. Posi ve findings are
o en are associated with more severe disease and
should increase clinical suspicion.
Ultrasound
Transvaginal ultrasound is not useful in diagnosing the
majority of cases of endometriosis as the peritoneal
implants and adhesions involved are not detectable. A
nega ve ultrasound could never be used as defini ve
evidence of the absence of endometriosis. However,
ultrasound remains a vital preopera ve inves ga on
because of its ability to detect ovarian endometriomas.
Endometriomas are described as having a ‘ground glass’
appearance on ultrasound as the thick altered blood
within the cyst has some echogenic proper es. The main
differen al is a haemorrhagic corpus luteum. Other
ultrasound clues are that endometriomas are o en
bilateral and the ovary is immobile to probing as it is fixed
to the pelvic side wall by inflammatory adhesions. Using
transvaginal, transrectal or renal ultrasound to define the
extent of deeply infiltra ng disease in the rectovaginal
septum, bladder or ureters, along with magne c
resonance imaging (MRI), is finding applica on in
preopera ve planning.
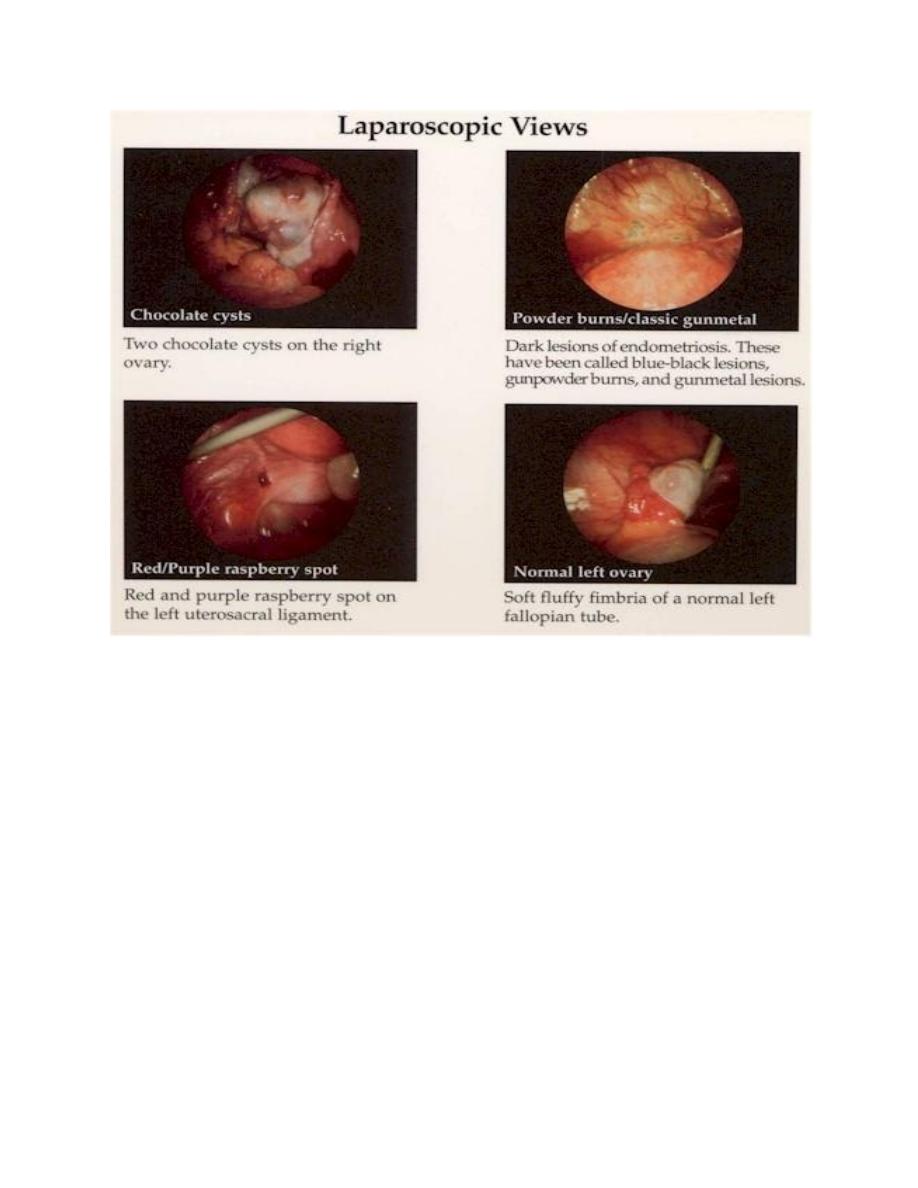
Laparoscopy
Laparoscopy is the gold standard inves ga on for the
diagnosis of endometriosis and now provides the main
tool of treatment. Visual recogni on is the means of
diagnosis, although histological confirma on is also
recommended as visual diagnosis alone varies in accuracy
Appearance:
Endometriosis May Appear
Brown
Black (“Powderburn”)
Clear (“Atypical”)
Endometriosis May Be Associated with Peritoneal
Windows
Differen al diagnosis
1. Ovarian cysts.
2. Pelvic inflammatory disease .

3. Other causes of nodularity in Douglas pouch as
tuberculous peritoni s and metastases of ovarian
cancer.
4. Causes of haematuria , bleeding per rectum and acute
abdominal pain if the pa ent is presented by one of
these symptoms.
5. Asymmetrical enlarged uterus.
How can endometriosis be classified?
A staging system has been developed by the American
Society of Reproduc ve Medicine (ASRM) to stage
endometriosis and adhesions due to endometriosis.
Stages 1 & 2 (minimal to mild disease): Superficial
peritoneal endometriosis. Possible presence of small
deep lesions. No endometrioma. Mild filmy adhesions, if
present.
Stages 3 and 4 (moderate to severe disease): The
presence of superficial peritoneal endometriosis, deeply
invasive endometriosis with moderate to extensive
adhesions between the uterus and bowels and/or
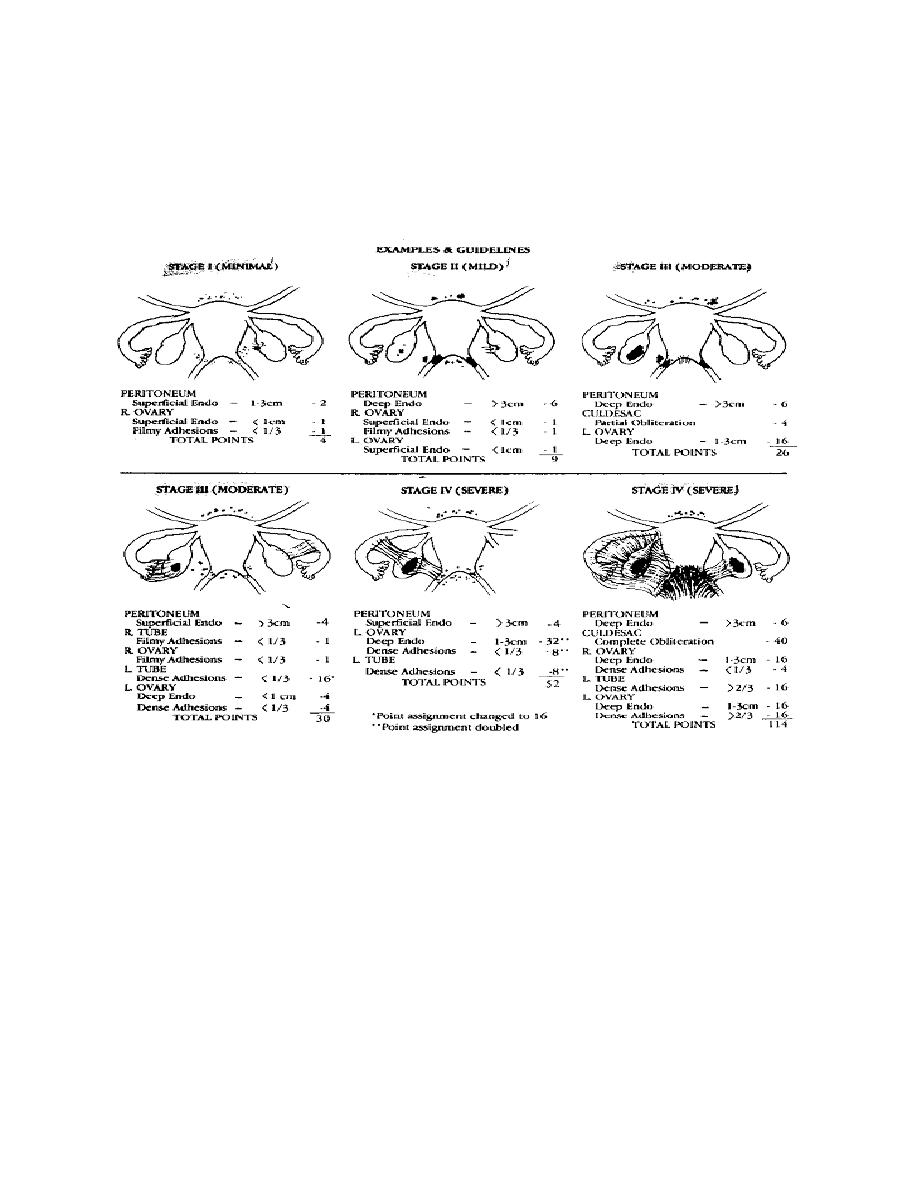
endometrioma cysts with moderate to extensive
adhesions involving the ovaries and tubes.
Apart from the classifica on system 3 subtypes of
endometriosis can be discerned according to localiza on:
superficial peritoneal endometriosis, cys c ovarian
endometriosis (endometrioma or ‘chocolate cysts’) and
deep endometriosis (also referred to as deeply infiltra ng
endometriosis). The different types of disease may

co-occur (i.e., a pa ent may have more than one type of
disease present in her pelvis).
Superficial peritoneal endometriosis: The most common
type is superficial peritoneal endometriosis. The lesions
involve the peritoneum, which is a thin film that cloaks
the inner surfaces of the pelvic cavity. The lesions are flat
and shallow and do not invade into the space underlying
the peritoneum.
Cys c ovarian endometriosis (ovarian endometrioma):
Less commonly women with endometriosis can develop
endometrioma in their ovaries. An endometrioma is a
cyst in which the wall of the cyst contains areas of
endometriosis. The cyst is filled with old blood. Because
of the colour, the cysts are also referred to as ‘chocolate
cysts’. Most women with endometrioma cysts will also
have superficial and/or deep disease present elsewhere
in the pelvis.
Deep endometriosis: Lastly, the least common subtype of
endometriosis is deep endometriosis. An endometriosis
lesion is defined as deep if it has invaded at least 5mm

beyond the surface of the peritoneum. Given the
peritoneum is very thin, deep lesions always involve
ssue underlying the peritoneum (the retroperitoneal
space).
Does endometriosis occur outside the pelvic cavity?
Although endometriosis is a gynecological disease,
associated with the menstrual cycle, it has been found in
almost any ssue of the body.
Endometriosis can affect the bowel, bladder, kidney and
pouch of Douglas, especially in deep endometriosis.
In rare cases endometriosis can also be found in the
lungs, in the chest on the diaphragm, in a scar of a
laparotomy, in the navel and in the groin. Endometriosis
can also lead to symptoms in women a er the removal of
the uterus.
The symptoms that women experience depend on the
localiza on of the endometrio c lesions, but are
classically cyclical. Cyclical shoulder pain may indicate
endometriosis on the diaphragm. Cyclical swelling and
some mes bleeding from the navel may be secondary to

umbilical endometriosis and is some mes misdiagnosed
as an umbilical hernia. The same applies to cyclical
swelling of the groin where an inguinal hernia is
diagnosed instead of endometriosis of the groin. Cyclical
signs of bladder dysfunc on should not automa cally
lead to an bio c therapy but rather to a suspicion of
endometriosis. In short all symptoms that are related to
the menstrual phase of the cycle should lead to a high
suspicion of the diagnosis endometriosis.
Treatment
Women with endometriosis have either pain, fer lity
problems or they have both.
Depending on the pa ent, the treatment will be
different. Your doctor will take several factors into
considera on when prescribing medical treatment or
advising surgical treatment. These factors include:
The preferences of the woman
The type of disease (peritoneal disease, ovarian cyst
or deep endometriosis)

The severity and type of pain symptoms
The wish to become pregnant immediately or at a later
stage
The costs and side-effects of some treatments
The age of the woman
The treatments she has already received.
The doctor (country, expert centre)
Medical treatments for endometriosis include hormonal
treatments or pain medica on (analgesics).
Hormonal treatments in clinical use are:
- hormonal contracep ves(cyclical use or con nuously)
- progestagens (oral or in an Intra Uterine Device)
- an -progestagens,
- GnRH agonists
- aromatase inhibitors
Surgery
Peritoneal implants can be removed by excision,
diathermy abla on or laser vaporiza on.
Treatment of
women with severe symptoma c disease involving
oblitera on of the pouch of Douglas and involvement of
the bowel, bladder or ureters should be referred to
centres specialising in complicated opera ve laparoscopy.
This surgery will o en be performed in consulta on with
a colorectal surgeon or urologist and
may involve bowel or bladder resec ons or
reimplanta on of ureters. Oophorectomy and
hysterectomy have become less common measures as
modern surgical treatment has concentrated on removal
of disease and restora on of normal anatomy...
Infer lity
There is no evidence to suggest that hormone treatment
is effec ve in trea ng infer lity in mild or severe
endometriosis. It should not be offered as treatment in
this situa on.18 In minimal to mild endometriosis,
surgical removal plus adhesiolysis appears to improve

fer lity when compared to diagnos c laparoscopy
alone.19–20 While evidence in these trials has some
weakness, it would seem a reasonable treatment. Where
success is not achieved referral for assisted reproduc ve
treatment in the form of ovula on induc on with
intrauterine insemina on or in vitro fer lisa on (IVF) is
appropriate. There is no reasonable data to answer this
ques on where the disease is moderate or severe. As the
disease becomes more severe pregnancy rates fall.
Where there is anatomical distor on of the pelvis
rec fying this at the me of surgery would seem
prudent. Early referral to assisted reproduc ve treatment
is suggested.
