
Gestational Trophoblastic
Disease (GTD)

GTD Overview
• Heterogeneous
group of related lesions
• Arise from abnormal proliferation of
trophoblast of
the placenta
• Can
follow any gestational event
– abortion,
miscarriage, ectopic, normal pregnancy
• Unique
because the maternal lesions arise from
fetal (not maternal) tissue
• Most GTD lesions produce
(B-hCG)
• Can be cured
even in the presence of widespread
metastases
Overview
Hydatidiform Mole:
• Complete
• Partial
** Benign
Gestational Trophoblastic Neoplasia (GTN):
• Persistent/Invasive Mole
• Choriocarcinoma
• Placental-Site Trophoblastic Tumor (PSTT)
** Malignant
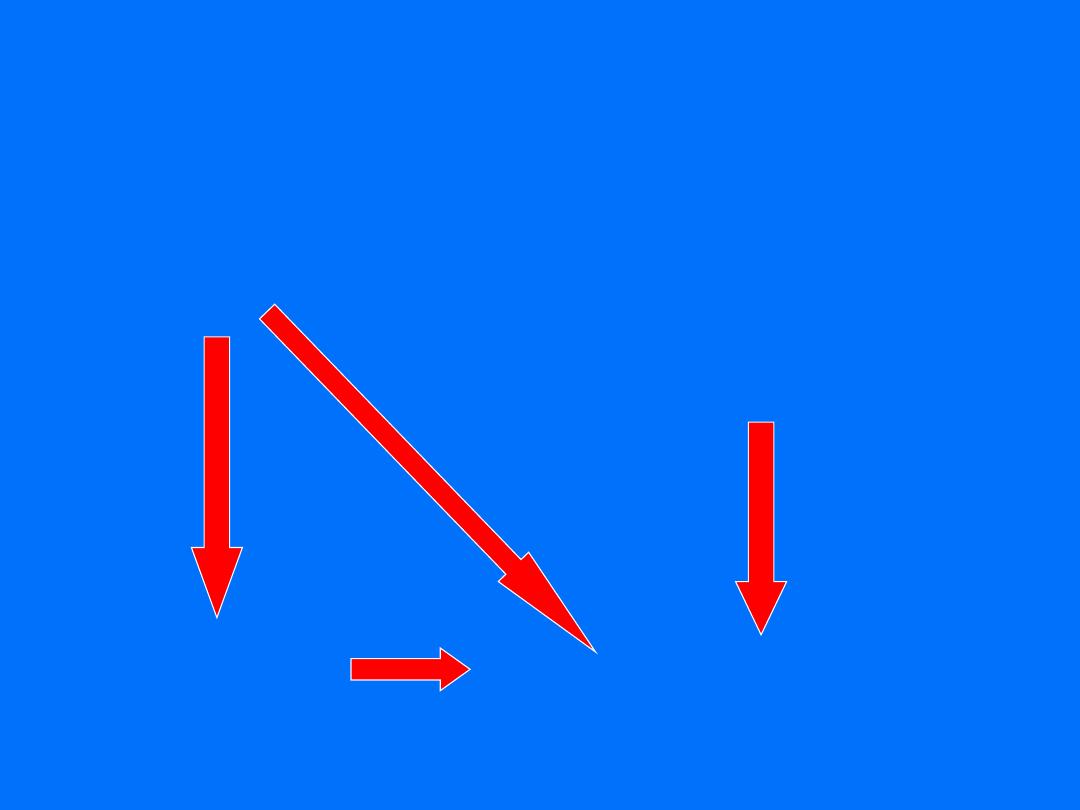
Relationship of HM. IM. CH
hydatidiform therapeutic or
mole
spontaneous abortion
term pregnancy
ectopic
invasion mole choriocarcinoma.

Hydatidiform mole

Hydatidiform Mole
• North America: 0.6-1.1 per 1000 pregnancies
• Asia: 2-10 per 1000 (3x Western countries)
• Difference possibly related low dietary intake
of carotene (vitamin A deficiency) and animal
fat
• More common at reproductive extremes in
age (>35y or <20y)

Hydatidiform Mole
Risk Factors:
• History of previous GTD
– If one previous mole, 1% chance of recurrence
(vs. 0.1% in general population)
– If 2 previous moles, risk of recurrence increases
to 16-28%
• Smoking
• Vitamin A deficiency
• Blood type:
– A or AB are at slightly higher risk than those with
type B or O
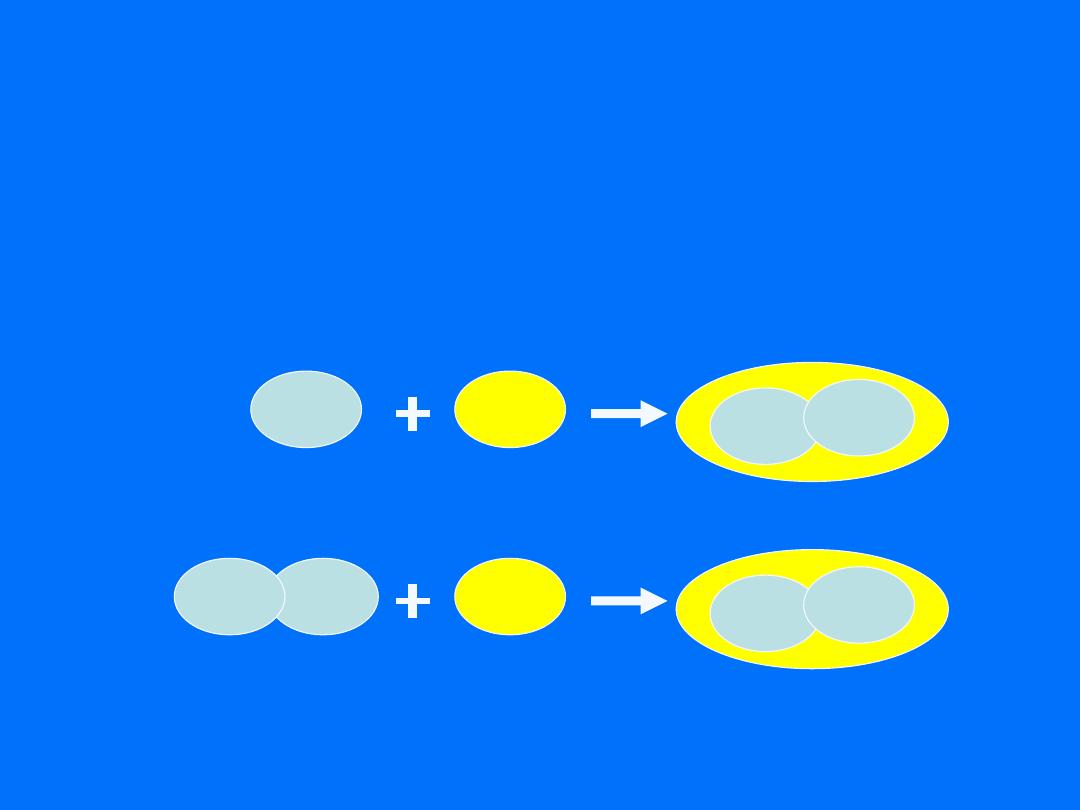
Hydatidiform mole
1. Complete mole
23X
sperm
empty egg
23X
23X
46,XX
23X
sperm
empty egg
23Y
23X
46,XY
23Y
sperm
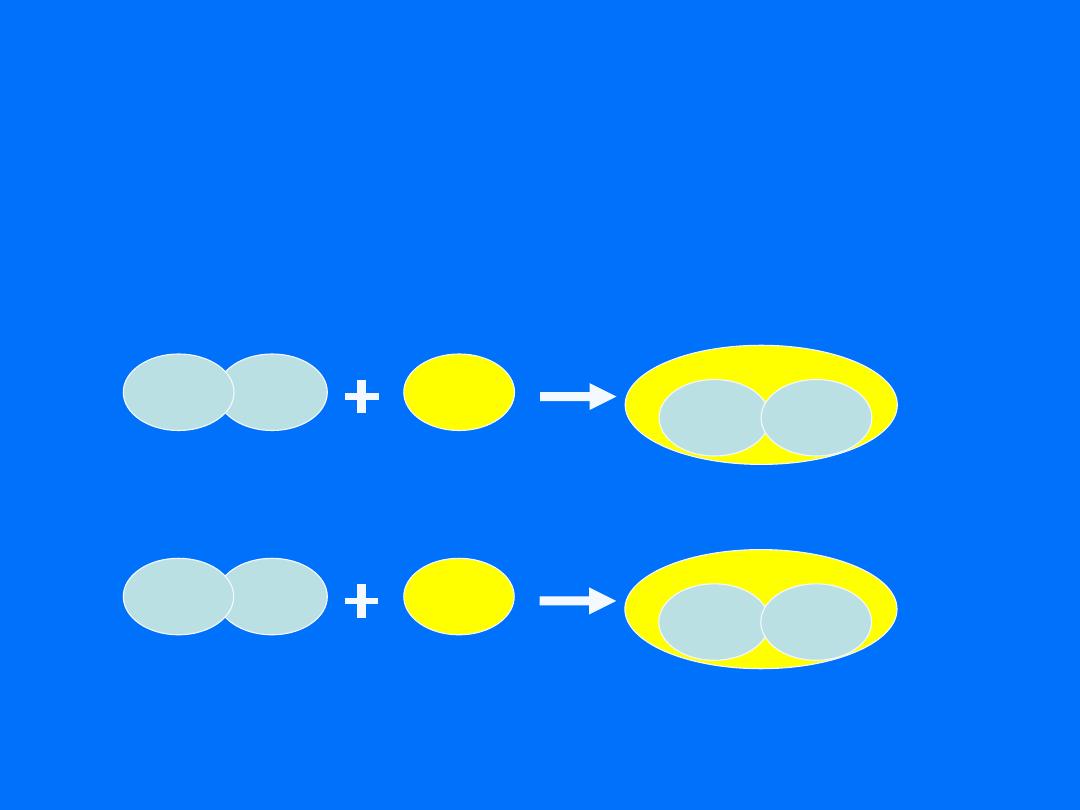
Hydatidiform mole
2. Partial mole
23X
sperm
normal egg
23Y
23X
69,XXY
23Y
sperm
23X
23X
23X
sperm
Normal egg
23X
23X
69,XXX
23X
sperm
23X
23X

Hydatidiform Mole
Clinical Manifestations:
• Vaginal bleeding
(97%)
/anemia
• Enlarged uterus (size > dates)
• Pelvic pain
• Theca lutein cysts
• Hyperemesis gravidarum
• Hyperthyroidism
• Preeclampsia <20 weeks gestation
• Vaginal passage of hydropic vesicles
• Partial mole usually presented as incomplete or
missed abortion

Diagnosis
• Complete :
U/S usually very sensitive – generalized
swelling (snow-storm )
• partial mole
U/S may detect focal cystic spaces of varying
diameter
Diagnosis on histology of curettings
Complete vs. partial mole
Partial
Complete
Feature
Triploid
(69,xxx or 69,
xxy)
Diploid(usually
46,xx or rarely
46,xy)
Karyotype
focal
diffuse
Swelling of chorionic villi
focal
diffuse
Trophoblastic hyperplasia
Present
absent
Embryonic tissue
usually<
100,000
Often > 100,000
hCG
<5%
15 - 20%
Trophoblastic sequelae
Rare
Up to 25%
Theca lutein cysts
Rare
Up to 25%
Medical complications
Small for dates
50% large for dates
Uterine size

Hydatidiform Mole Treatment
• Evaluate for coexisting conditions:
- History and physical
- CBC, coagulation profile, serum chemistry
- thyroid function
- blood type and cross match
- chest radiography
- pelvic ultrasonography
• Evacuation of mole
-
Suction curettage
-
Hysterectomy
if completed childbearing
• If Rh negative, give rhogham

Hydatidiform Mole Treatment
chemotherapy
HM don’t need usually chemotherapy
because HM is benign disease.

Follow-Up Care – Molar Pregnancy
• 80% of patients cured by evacuation
• Follow B-hCG levels every two weeks until 3 consecutive tests
negative
• Then monthly B-hCG every month for 6-12 months
• More than half of patients will have complete regression of
hCG to normal within 2 months of evacuation.
• Avoid pregnancy for at least 6 months after first normal B-hCG
(oral contraceptive pills is preferable)
• Subsequent Pregnancies:
– Send placenta for pathology
– Check B- hCG 6 weeks postpartum

Prognosis
• Complete mole has the latent risk of local
invasion or telemetastasis
• The high-risk factors includes
– β-HCG>100000IU/L
– uterine size is > 20 weeks size.
– the luteinizing cyst is >6cm
– If >40 years old,the risk of invasion and metastasis
may be 37%, If >50 years old,the risk of invasion
and metastasis may be 56%.
– repeated mole: the morbidity of invasion and
metastasis increase 3~4 times

Gestational Trophoblastic Neoplasia
(GTN)
• Persistent/Invasive Mole
• Choriocarcinoma
• Placental-Site Trophoblastic Tumor (PSTT)
** Malignant

Risk Factors for GTN After Mole
• Preevacuation uterine size greater than
gestationl age or larger than 20 weeks
gestation
• Theca-lutein cysts larger than 6 cm
• Age > 40 years
• Serum hCG levels > 100,000 mIU/mL
• Previous hydatidiform mole

Invasive Mole
• Myometrial invasion by hydatidiform mole
• Formerly known as
chorioadenoma destruens
• 1 in 15,000 pregnancies
• 10-17% of hydatidiform moles will progress to
invasive moles

Persistent Mole
Definition of persistent molar disease and need for
chemotherapy (at least one of the following):
– B-hCG plateau for ≥ 4 values for ≥ 3 weeks
– B-hCG increase of ≥ 10% for ≥ 3 values for ≥ 2
weeks
– B-hCG persistence 6 months after molar
evacuation
– Histopathologic diagnosis of choriocarcinoma
– Presence of metastatic disease

Choriocarcinoma
• Most aggressive type of GTN
• Abnormal trophoblastic hyperplasia
• Absence of chorionic villi
• Direct invasion of myometrium
• Most often develops from a
complete
hydatidiform mole
• Vascular spread to distant sites:
– Lungs
– Brain
– Liver
– Pelvis and vagina
– Spleen, intestines, and kidney

Choriocarcinoma
• May come from any type of pregnancy
- 25% follow abortion or tubal pregnancy
- 25% with term gestation
- 50% from hydatidiform moles
• 2-3% of moles progress to choriocarcinoma
• Incidence 1 in 40,000 pregnancies
– Rarely, choriocarcinomas can develop in other parts of the
body in both men and women. These are not related to
pregnancy as ovaries and testicles
• Nongestational choriocarcinoma tends to be less
responsive to chemotherapy and has a less favorable
prognosis than the gestational variant

Placental-Site Trophoblastic Tumor
(PSTT)
• Originate from intermediate cytotrophoblast
cells
• Secrete
human placental lactogen
(hPL)
• B-hCG often
normal
• Less vascular invasion, necrosis and
hemorrhage than choriocarcinoma
• Lymphatic spread
• Arise months to years after term pregnancy
but can occur after spontaneous abortion or
molar pregnancy

Placental-Site Trophoblastic Tumor
(PSTT)
• Most common symptom is vaginal bleeding
• Tend to:
- Remain in uterus
- Disseminate late
- Produce low levels of B-hCG compared to
other GTN
- Be resistant to chemotherapy (treat with
surgery)

Signs & Symptoms GTN
• Continued uterine bleeding, uterine
perforation, enlarged irregular uterus,
persistent bilateral ovarian enlargement
• From metastatic lesions: abdominal pain,
hemoptysis, melena, increased intracranial
pressure (headaches, seizures, hemiplegia),
dyspnea, cough, chest pain

Diagnosis of GTN
• Increase or plateau in B-hCG after molar
pregnancy
• Pathologic diagnosis by D&C or biopsy of
metastatic lesions
• WARNING: biopsy of metastatic lesions can
result in massive hemorrhage
• Metastatic workup: CXR (or CT chest), CT
abdomen/pelvis +/- CT/MR of brain

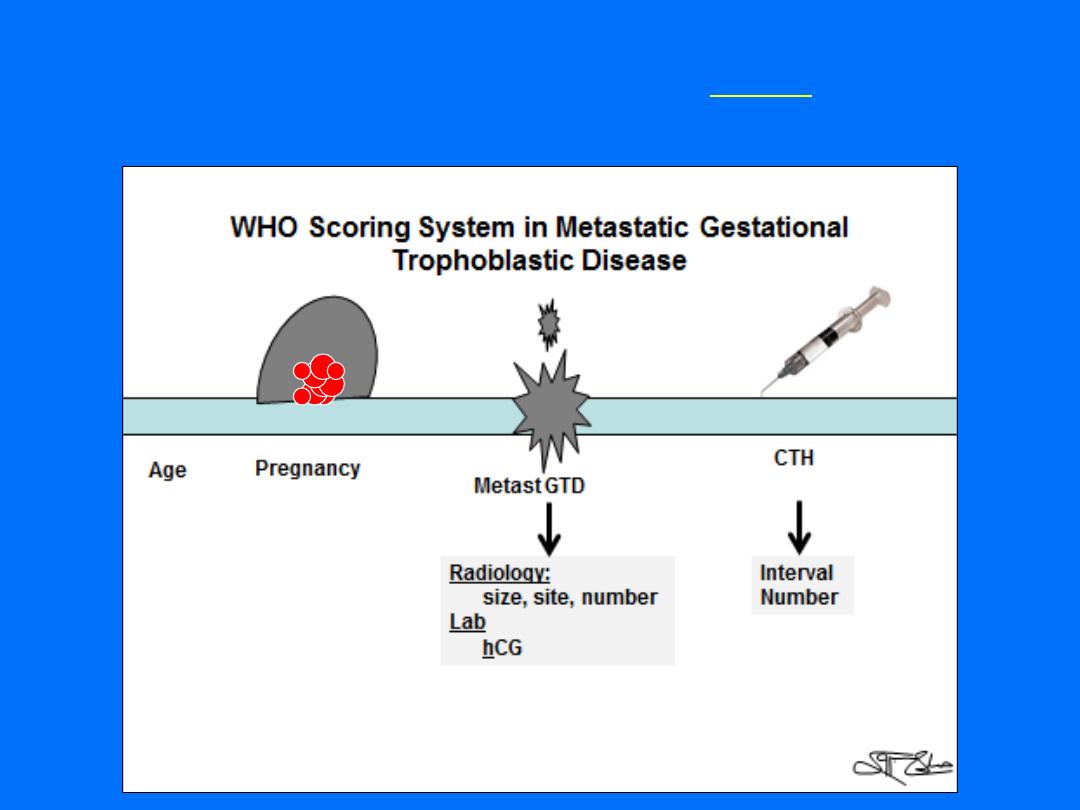
Classification & Staging of GTD
• FIGO Staging
– Describes anatomic distribution of disease
• World Health Organization (WHO) Scoring
Index
– Describes prognosis
FIGO Staging
Stage
Description
I
Disease confined to the
uterus
II
Disease extends outside the uterus but
limited to genital structures
(adnexa,
vagina, and broad ligament)
III
Disease extends to the
lungs
with or
without genital tract involvement
IV
Disease involves any
other metastatic sites
The World Health Organization (WHO) scoring
system for GTD
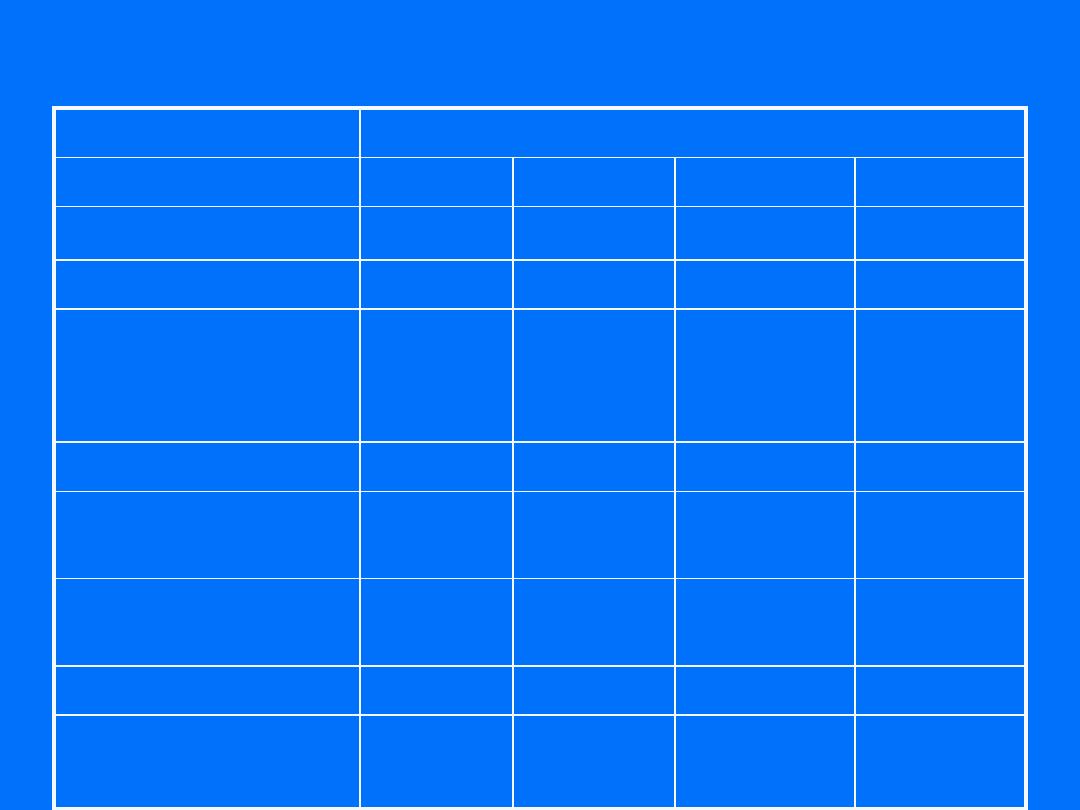
WHO Prognostic Score Index
Score
Characteristic
0
1
2
4
Age
<40
≥40
-
-
Antecedent preg
Mole
Abortion
Term
-
Pregnancy to
treatment
Interval (months)
<4
months
4-6
months
7-12 months >12 months
Pretreatment hCG
<10
3
10
3
- 10
4
10
4
-10
5
>10
5
Largest tumor size
(including uterus)
< 3cm
3-4 cm
≥5cm
-
Site of metastases
Lung
Spleen,
kidney
GI tract
Liver, brain
Number of metastases
-
1-4
5-8
>8
Previous failed
chemotherapy
-
-
Single drug
≥2 drugs

Therapy for GTN
• Single agent therapy for nonmetastatic
(stage I) or low-risk metastatic (stage II and
III) with score <7 → survival rates ~ 100%
• Combination chemotherapy +/- radiation
and/or surgery for high-risk metastatic
disease with score ≥7

Therapy: Nonmetastatic GTN
• Single-agent with either methotrexate or
dactinomycin
• Chemotherapy continued until hCG values normal
and then
2-3 cycles beyond
• Change to alternative single-agent for hCG plateaus
above normal or toxicities
• If significant elevation of hCG or new metastases,
switch to multiagent
• 85-90% cured with initial regimen, <5% will require
hysterectomy for cure

Therapy: Low-risk Metastatic GTN
• Low-risk metastatic disease can be treated
with single-agent therapy with 5-day
regimens
• Cure rates ~100% but 30-50% will be develop
resistance to first agent
• If resistance to sequential single-agent
chemotherapy (5-10% of patients), switch to
multiagent chemotherapy

Therapy: High-risk Metastatic GTN
• Stage IV
• Stage II/III with score > 7
• Disease refractory to single-agent chemotherapy
Combination Chemotherapy:
• EMACO:
– Day 1: Etoposide, Methotrexate and Dactinomycin
– Day 8: Cyclophosphamide and Vincristine
(Oncovorin)
– Repeat q2 weeks until remission
– Continue for at
least 2-3 cycles beyond first normal
hCG
• MAC (Methotrexate, Dactinomycin, Cyclophosphamide)
• EMA/EP – EMA + Etoposide and Cisplatin

Metastatic Gestational Trophoblastic Tumors
• Surgery
– It is indicated for tumor resistant to
chemotherapy and single metastases persisting
despite chemotherapy.
• RT
– RT, in combination with chemotherapy, is clearly
indicated for the primary management of patients
with brain metastases.

PSTT Therapy
• Hysterectomy
• Chemotherapy for metastatic disease or
nonmetastatic disease with poor prognosis:
- Interval from index pregnancy > 2 years
- Deep myometrial invasion
- Tumor necrosis
- Mitotic count > 6 per 10 high-power fields
• Survival rates:
– ~100% for nonmetastatic disease
– 50-60% for metastatic disease

Follow-up Care
• After completion of chemotherapy, follow
serial hCG every 2 weeks for three months,
then monthly for one year
• Physical examinations every 6-12 months and
imaging as indicated

Reproductive Performance
• Most women resume normal ovarian
function
• Women who undergo chemotherapy are
advised not to conceive for one year after
completion of treatment
• No increase risk of stillbirths, abortions,
congenital anomalies, prematurity, or major
obstetric complications

False Positive Serum hCG
• Phantom hCG syndrome/ phantom
choriocarcinoma
• 3-4% of healthy individuals have human-antimouse
antibodies that can mimic hCG immunoreactivity
• To verify:
– Urine hCG should be negative
– Should not show parallel decrease with serial dilutions
– Test at national B-hCG reference lab
Summary
• Hydatidiform mole is a benign condition, 80%
cured with suction D&C
• Malignant GTN:
– Persistent or invasive mole
– Choriocarcinoma
– PSTT
• WHO score > 7 represents high-risk disease
• GTN very sensitive to chemotherapy

Thank You For Your Time
